Clinical examination arbitrating the need of investigations: Importance of Red-flags
When an 86 years old gentle lady arrived in our emergency room with back pain, right shoulder pain, difficulty in walking and fever, the initial assessment revealed no striking finding other than severe painful restriction of right shoulder movement. Her neurological examination was normal, but she was too tired even to attempt walking. She had an MRI done four days earlier which showed age-related degenerative changes only. These MRI findings precluded any further thoughts about the acute spinal disorder, whereas the severe shoulder pain blocked the gateway of supposed to be severe back pain. She was admitted for fever evaluation and pain management. On the next day, patient’s pain was better but had tachypnoea, hyperthermia and malaise. White blood cell counts were elevated and Creactive protein was 226(very high) denoting sepsis. There was a slight decrement in her lower limb power (4/5 MRC grade) which alarmed us.
What should be done at this scenario? What is a red-flag and what are the red-flags in the spine?
Red Flag – low back pain
- Indicate possible serious pathology
- Indicate the need for further investigation and, possibly, specialist referral
-
Possible fracturePossible tumour/infectionPossible significant neurological deficit
-
* Major trauma
* Minor trauma in elderly or osteoporotic patient
* Age < 20 or < 50 years
* History of cancer
* Constitutional symptoms (fever, chills, weight loss)
* Recent bacterial infection
* IV drug use
* Immunosuppression
* Pain worse at night or when supine
* Severe or progressive sensory alteration or weakness
* Bladder or bowel dysfunction
* On physical examination: evidence of neurological deficit (in legs or perineum in the case of low back pain)
Our patient was more than 50 years old and had fever, rest pain and weakness – four red flags definitely warranting an MRI. Unfortunately, she just had an MRI done 4 days back which was normal. This had brought up two issues – patient and attendants were reluctant to repeat the scan, and the burden of convincing them. While they were hesitating to proceed further, on the same day evening there was further worsening of neurology (right lower limb- 3/5 and left- 2/5 MRC grade). Thus, we rushed her to the MRI room immediately.
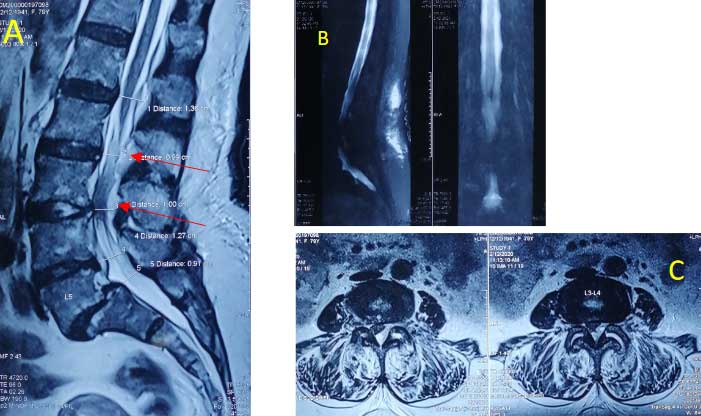
Fig. A – sagittal image and C – axial cut showing dorsal epidural abscess compressing the cauda equina; B – MR myelogram showing “cut-off” sign.
MRI revealed infective arthritis at left L3-4 facet with epidural abscess from L1 to L4 with severe compression at L3-4 level, which explained her sepsis and neurodeficit. L3-4 wide decompression, debridement and biopsy was done on an emergency basis. Empirical antibiotics were started which were switched later assenting culture and sensitivity reports (MRSA was identified). The lower limb power gradually improved with remarkable progress in general condition and she was back on her legs at 2 weeks post-op.
In our day-to-day clinical practice, we often face this kind of situation with a hesitation of “to do or not to do”. The growing dissonance in the doctor-patient relationship further fan the flames. A good counselling of the patient and making them understand the treatment plan usually avoids most of these issues. Quoting Hippocratic Oath “I will apply, for the benefit of the sick, all measures [that] are required, avoiding those twin traps of overtreatment and therapeutic nihilism”, When the clinical findings dictate and the existing protocols concur, do not hesitate to repeat the investigations.

Dr. P. Keerthivasan
Consultant Orthopaedic & Spine Surgeon
Kauvery Hospital, Chennai

