What is Mucormycosis and how do we get infected by it?
Mucormycosis (being called as black fungus) is a complication caused by a serious fungal infection, which typically does not act as a serious threat to those with a healthy immune system.
However, now a spike is observed in mucormycosis among individuals hospitalised for or recovering from COVID-19 infection. Therefore, it is emerging as the most significant challenge in the second wave of COVID-19 infections. It is a non-contagious disease.
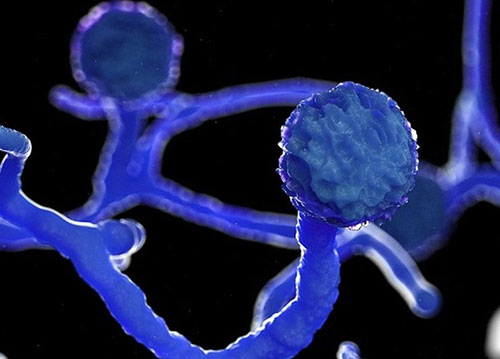
It belongs to a fungal family of Mucorales. Usually its fungal spores are present in our environment all around us. Normally, we inhale these spores, we even swallow them, but our immune system helps us avoid these spores from invading our body system and prevents us from getting infected.
People whose immune system is compromised with medical conditions including:
- uncontrolled diabetes,
- patients on immunosuppressive therapy, chemotherapy, cirrhosis,HIV,
- malignancy(cancer),
- post-transplant,
- medical conditions that suppress immunity are more prone to get infected.
Despite this, however, there have been cases of mucormycosis reported with no apparent predisposing factors present.
As mentioned earlier, recently, this disease is being found among patients who are in the process of recovering or have recovered from COVID-19.
- Both symptomatic and asymptomatic patients with COVID-19 may be at risk.
- Patients who have been hospitalized for COVID-19 illness are at a much higher risk.
- Moreover, anyone who is having diabetes and whose immune system is not functioning good needs to be very careful.
This fungal spore, once it enters the human body, can be really dangerous and spreads very fast. It can be fatal and has a mortality rate of 50 – 70 percent, depending upon the type and involvement.
Where in the body does the fungus infect the most?
Areas affected most by this aggressive infection include:
- The nose
- The sinuses
- The lungs
- The eyes
- The brain
- Exposed wounds
What are the most common symptoms?
The most common and early symptoms for patients who get infected with mucormycosis are:
Common symptoms – in case of nose and sinus involvement
- Excessive dryness in the nose
- Crust formation in nasal cavity leading to nasal block
- Unusual nasal discharge,
- bleeding from nose
- Decreased sensation over nose tip, cheeks, upper lips
- Facial pain
- One-sided facial swelling: over cheeks, around cheeks
- Discolouration (reddish, blackish) over nose, palate, cheeks
Common symptoms – in case of orbital (eye)/ brain
- Red eyes
- Bulge around eyes
- Decreased vision/ blurred or double vision
- Pain around the eye with watery eyes
- Headache
- Swelling around eyes
Common symptoms – in case of pulmonary (lungs) mucormycosis
- Fever
- Cough
- Chest pain
- Breathing difficulties
- Dyspnea: Shortness of breath
- Haemoptysis: Coughing with blood
Common symptoms – in case of Gastrointestinal mucormycosis
- Abdominal pain
- Nausea
- Vomiting
- Gastrointestinal bleeding
What happens when a patient comes in with these symptoms?
There are a set of treatment protocols to be followed once anybody shows up at the hospital with symptoms mentioned earlier.
The protocols are followed keeping in mind the utmost safety of the suspected patient and the health care workers present in the same environment.
Treatment protocols
- The suspected patient has to report to hospital immediately.
- He has to undergo clinical examination, and a nasal endoscopy should be performed.
- Then a series of CT and MRI investigations are done.
- If the fungal growth is found, its sample is collected and sent for biopsy.
- Later, surgical debridement has to be done, and medical management is started immediately.
Early intervention and treatment is strongly recommended for better outcomes.
How can the risk of mucormycosis be lowered?
There is no vaccine against the black fungus infection, and it is difficult to avoid breathing in the fungal spores that cause the infection as these are commonly present in the environment all around us.
These are the steps one can take to lower the risk.
- Observe warning signs and symptoms
- Do not discard all the cases with a blocked nose as those cases of bacterial sinusitis, specifically in the context of immunosuppression and/or COVID-19 patients on immunomodulators
- Do not fail to seek thorough examinations as apt for determining fungal etiology
- Do not waste precious time to begin treatment for mucormycosis
After recovering from coronavirus, one should closely monitor and should not miss any warning signs and symptoms mentioned above as the fungal infection is found to emerge even weeks or months after recovery.
Why is it seen mostly in COVID-related patients?

We know that the coronavirus affects the immunity of a body in such away that the immune system has been breached to a very dangerous level.
This signifies that the body is now prone to get infected by many more diseases and conditions that could have been avoided under normal immunity levels.
Therefore, the spores of fungi which are generally present all around the environment take advantage of such a situation and invade the human tissues, thereby adversely affecting them.
These are called opportunistic infections.
The picture above represents the coronavirus and mucor fungi together in the body of an infected individual whose immunity levels are breached.
Conclusion
While we wait to get vaccinated, we see newer and more serious conditions emerging in association with COVID-19. Mucormycosis (black fungus)is an example of a deadly fungal infection seen among COVID-19 patients across hospitals in India.
People having diabetes, those using steroids and humidified oxygen consistently, and COVID patients having pre-existing comorbidities are most susceptible to this infection. Others comprise those on long-term immunosuppressive drugs and also cancer patients.
It is crucial to cognize and be aware of such health complications and symptoms during the pandemic. It aids in starting the appropriate treatment on time.
Dr. Niraj Kumar Joshi
Senior Consultant ENT, Head and Neck Surgeon
Kauvery Hospital, Chennai

