Journal scan: A review of 26 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Neeraj Dhaun, et.al. Endothelin antagonism: stepping into the spotlight. The Lancet. 2023;402(10416):19412044.
Background
Endothelin 1, the most potent endogenous vasoconstrictor, was discovered in 1988, 1 followed closely by the identification of its two receptors, endothelin A and endothelin B. Many clinical trials have not shown efficacy of either selective endothelin A or mixed endothelin A and endothelin B antagonists in various cardiovascular diseases 2 and the only licensed indications for these agents are pulmonary arterial hypertension and scleroderma digital ulceration, both rare diseases. However, chronic kidney disease might give endothelin antagonists a more common indication.
(2). Richard Horton, et al. The moral clarity of WHOs Director-General. The Lancet. 2023;402(10416):1953.
Background
Amid the claims and counterclaims about war crimes in Gaza and Israel, one voice has stood out as a beacon of moral claritythat of WHOs Director-General Tedros Adhanom Ghebreyesus. The day after the Oct 7, 2023 terror attacks on Israel, recognising that the Israeli Government would strike back, he presciently called on X, formerly Twitter, for urgent steps to: protect and safeguard civilians, health workers and health facilities. By Oct 10, as Israel escalated attacks against Hamas, with widespread killing of civilians, he demanded access to health and humanitarian assistance and an end to the hostilities that are causing untold suffering. Israels bombing brought Gazas hospitals to breaking point. On Oct 13, Tedros wrote We implore Israel to reverse this decision to evacuate Al Awda Hospital. And later: I plead to the Israeli government to revoke this decision and avoid a human tragedy. WHO was now flying medical supplies to Al Arish in Egypt, close to the Rafah crossing. Tedros stepped up his advocacy. He pointed to the lack of access to clean water as a risk for waterborne disease outbreaks. He underlined the impossibility of implementing Israels orders to evacuate hospitalsa death sentence for the sick and injured. And he advised all parties that the only solution is dialogue, understanding, compassion and peace.
Im speechless over this tragedy, he wrote on Oct 24. He has intensified his calls for a humanitarian ceasefire, instead of the current reality of cease-food, cease-water, cease-fuel, cease-care imposed on Gazans.
(3). Emmanuelle Vigarios et al. Difficulty diagnosing oral cancer: seeking an early specialist opinion is key. The Lancet. 2023;402(10416):2018
Background
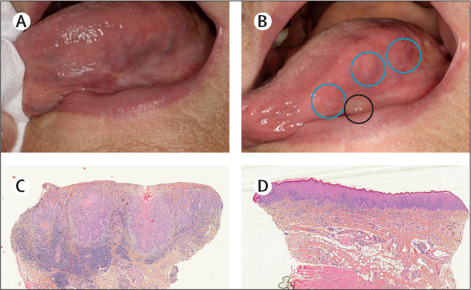
A 95-year-old woman attended our oral medicine department reporting a painful white plaque on the left margin of her tongue. The patient had been seen by her dentist 8 months earlier, who concluded that the small, nodular, white patch (figure), opposite a broken tooth, had been caused by trauma; he polished the broken tooth and arranged no follow-up appointments. However, 8 months later, the patient went back to her dentist because of persistent pain; the white patch had progressed, and the dentist referred her to us.
The patient had a history of hypertension treated with candesartan; she reported no tobacco use or alcohol consumption.
View related content for this article
On examination
She was generally well; in her mouth the original white plaque had developed an ulcerated lichenoid appearance, and three new plaques were present on her tongue (figure). Regional lymph nodes in the neck were not palpable. Two biopsies were taken and each examined at three levels: the first showed squamous cell carcinomatous proliferationessentially in situ, locally ulcerated, with focal budding of the basal layer and micro-infiltrative subepithelial small clumps or squamous epithelial cells (figure); the second biopsy found an acanthotic leukokeratotic mucosa with sparse subepithelial lymphocytic inflammation, and a few apoptotic bodies (figure). Well differentiated micro-invasive squamous cell carcinoma of the tongue was diagnosed. The second biopsy also showed lichenoid inflammation.
The patient had a partial glossectomy and a sentinel lymph node biopsy which showed no signs of metastasis; no adjuvant treatment was indicated. At her last follow-up 1 year after surgery, the patient was in clinical remission.
Diagnosis
Late diagnosis of oral cancers as with many malignancies results in poorer prognosis. Notably, oral traumatic lesions typically resolve within 4 weeks once the causative agent is removed.
All new oral white and red patches, whether they appear malignant or not, should be monitored and investigated. Importantly, any plaque, patch, ulcer, lump, or anything that appears atypical needs to be explored and the aetiology found; many head and neck cancers present initially with lesions in the oral cavity. The persistence of pain and any persistent or progressive lesion should be biopsied to avoid missing an oral squamous cell carcinoma or misdiagnosing a lesion that appears to be benign. The National Institute for Health and Care Excellence (NICE), in the UK, guidelines recommend that any non-healing oral ulcer or a lump on the tongue should be referred to a specialist so that patients with a suspected cancer are seen within 2 weeks.
(4). Mandip Aujla, et. al. The cycling of self-care through history. The Lancet. 2023;402(10408):113346
Background
Self-care: when taken as the ability of individuals, families and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a health worker, as defined by WHOextends far beyond the common perception of individual acts of self-interest, to a set of behaviours and practices determined by a persons cultural, environmental, and socioeconomic circumstances.
The roots of self-care lie in antiquity. Until medicine was professionalised, maintenance of health typically took place in an individuals home and community
In Ayurveda, the classical text Astanga Samgraha encourages individuals to take responsibility for their own health in balanced interaction with other beings and the environment.
In ancient Greece, Galen described factors that were important for the maintenance of health and over which a person had some influence: air and environment, diet, sleep and waking, exercise and rest, evacuation and retention, and passions and emotions.
The arrival of hospital and laboratory based biomedicine led to a change not only in how diseases were conceived, but also in the role of health care in society.
Knowledge concentrated in the hands of experts, in contrast with self-care in domestic and community settings where knowledge was largely in the hands of everyone, widely shared, and dependent on social support.
Public policies in support of self-care must function to demystify health care, creating enabling environments in which people can more readily promote their health and care for themselves during illness.
While self-care during illness may be a new and challenging idea to health professionals, it is and always has been a dominant form of care in illness
The need for self-care arises out of systematic and institutional failures in existing medical systems.
For some people self-care is therefore a necessity; others choose it.
The 2019 WHO living guideline on self-care interventions views individuals as active decision makers in their own health and describes modern evidence-based interventions that can be provided fully or partly outside of formal health services and used with or without a health worker, such as self-management of medical abortion during early pregnancy, self-monitoring of blood pressure, and home-based self-testing for some diseases.
People always have and always will engage in self-care. While self-care sometimes intersects with modern medicine, traditional values and belief systems are also foundational to many of those self-care practices.
(5). Kmietowicz Z. Thalassaemia: NHS to offer stem cell transplants to adults who need transfusions. BMJ. 2023;383:2837
Adults who have transfusion dependent thalassaemia are being given access to stem cell transplantations on the NHS, a treatment previously available only to children.
Advances in transplant treatment, such as better drugs to manage a patient before, during, and after transplantation, mean that allogeneic haematopoietic stem cell transplant (HSCT) has been recommended for eligible adults over 18 in new guidance from NHS Englands clinical priorities advisory group.
Transfusion dependent thalassaemia is a severe form of the condition.
(6). Elisabeth Mahase. Valproate prescribing rules will tighten from January, says MHRA. BMJ. 2023;383:2836
From January 2024 valproate must not be started in new patients aged under 55 unless two specialists agree that there are no alternative options or that compelling reasons mean that the reproductive risks do not apply, the UK Medicines and Healthcare Products Regulatory Agency (MHRA) has said.
(7). Michaela Waibel et al. Baricitinib and -Cell Function in Patients with New-Onset Type 1 Diabetes. N Engl J Med 2023; 389:2140-2150
Abstract
Background
Janus kinase (JAK) inhibitors, including baricitinib, block cytokine signaling and are effective disease-modifying treatments for several autoimmune diseases. Whether baricitinib preserves -cell function in type 1 diabetes is unclear.
Methods
In this phase 2, double-blind, randomized, placebo-controlled trial, we assigned patients with type 1 diabetes diagnosed during the previous 100 days to receive baricitinib (4 mg once per day) or matched placebo orally for 48 weeks. The primary outcome was the mean C-peptide level, determined from the area under the concentrationtime curve, during a 2-hour mixed-meal tolerance test at week 48. Secondary outcomes included the change from baseline in the glycated hemoglobin level, the daily insulin dose, and measures of glycemic control assessed with the use of continuous glucose monitoring.
Results
A total of 91 patients received baricitinib (60 patients) or placebo (31 patients). The median of the mixed-mealstimulated mean C-peptide level at week 48 was 0.65 nmol per liter per minute (interquartile range, 0.31 to 0.82) in the baricitinib group and 0.43 nmol per liter per minute (interquartile range, 0.13 to 0.63) in the placebo group (P=0.001). The mean daily insulin dose at 48 weeks was 0.41 U per kilogram of body weight per day (95% confidence interval [CI], 0.35 to 0.48) in the baricitinib group and 0.52 U per kilogram per day (95% CI, 0.44 to 0.60) in the placebo group. The levels of glycated hemoglobin were similar in the two trial groups. However, the mean coefficient of variation of the glucose level at 48 weeks, as measured by continuous glucose monitoring, was 29.6% (95% CI, 27.8 to 31.3) in the baricitinib group and 33.8% (95% CI, 31.5 to 36.2) in the placebo group. The frequency and severity of adverse events were similar in the two trial groups, and no serious adverse events were attributed to baricitinib or placebo.
Conclusions
In patients with type 1 diabetes of recent onset, daily treatment with baricitinib over 48 weeks appeared to preserve -cell function as estimated by the mixed-mealstimulated mean C-peptide level. (Funded by JDRF International)
(8). Eleanor L. Ramos et al. Teplizumab and -Cell Function in Newly Diagnosed Type 1 Diabetes. N Engl J Med 2023; 389:2151-2161
Abstract
Background
Teplizumab, a humanized monoclonal antibody to CD3 on T cells, is approved by the Food and Drug Administration to delay the onset of clinical type 1 diabetes (stage 3) in patients 8 years of age or older with preclinical (stage 2) disease. Whether treatment with intravenous teplizumab in patients with newly diagnosed type 1 diabetes can prevent disease progression is unknown.
Methods
In this phase 3, randomized, placebo-controlled trial, we assessed -cell preservation, clinical end points, and safety in children and adolescents who were assigned to receive teplizumab or placebo for two 12-day courses. The primary end point was the change from baseline in -cell function, as measured by stimulated C-peptide levels at week 78. The key secondary end points were the insulin doses that were required to meet glycemic goals, glycated hemoglobin levels, time in the target glucose range, and clinically important hypoglycemic events.
Results
Patients treated with teplizumab (217 patients) had significantly higher stimulated C-peptide levels than patients receiving placebo (111 patients) at week 78 (least-squares mean difference, 0.13 pmol per milliliter; 95% confidence interval [CI], 0.09 to 0.17; P<0.001), and 94.9% (95% CI, 89.5 to 97.6) of patients treated with teplizumab maintained a clinically meaningful peak C-peptide level of 0.2 pmol per milliliter or greater, as compared with 79.2% (95% CI, 67.7 to 87.4) of those receiving placebo. The groups did not differ significantly with regard to the key secondary end points. Adverse events occurred primarily in association with administration of teplizumab or placebo and included headache, gastrointestinal symptoms, rash, lymphopenia, and mild cytokine release syndrome.
Conclusions
Two 12-day courses of teplizumab in children and adolescents with newly diagnosed type 1 diabetes showed benefit with respect to the primary end point of preservation of -cell function, but no significant differences between the groups were observed with respect to the secondary end points. (Funded by Provention Bio and Sanofi)
(9). Johnny Ludvigsson et al. Immune Interventions at Onset of Type 1 Diabetes: Finally, a Bit of Hope. N Engl J Med. 2023; 389:2199-2201
Huge improvements in the treatment of many serious diseases have been made in the past half century, during which I have had the privilege of working first as a pediatric oncologist and later as a diabetologist. In the field of pediatric oncology, scientific progress has dramatically changed the prognosis for many forms of cancer from very high mortality to a cure for most children who are affected. Furthermore, effective therapy for other disabling diseases such as juvenile idiopathic arthritis now exists, and severe symptoms of childhood asthma are rare, owing to advances in care. The list goes on
(10). Jiang-Wei Cheng et al. Intravascular Large B-Cell Lymphoma. N Engl J Med 2023; 389:2188
Case Presentation
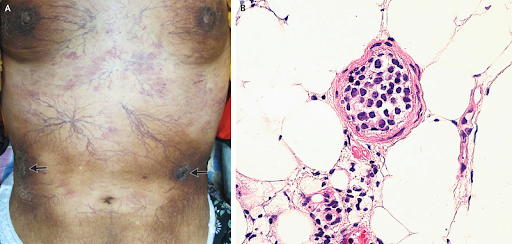
A 53-year-old woman presented to the dermatology clinic with a 3-month history of worsening vascular skin lesions and a 1-month history of fever.
On physical examination, diffuse telangiectasias, hyperpigmented plaques, and several ulcerated nodules (arrows) were observed on the skin across the chest and abdomen (Panel A) and the legs. No palpable lymphadenopathy or hepatosplenomegaly was noted.
Laboratory studies were notable for a lactate dehydrogenase level of 356 U per liter (reference range, 120 to 250).
A deep skin-biopsy specimen from the abdomen showed intravascular aggregation of round, atypical lymphocytes (Panel B, hematoxylin and eosin staining). Subsequent immunohistochemical staining was positive for CD20, PAX-5, and MUM-1 in the neoplastic cells.
A positron-emission tomographiccomputed tomographic scan was negative.
A diagnosis of intravascular large B-cell lymphoma was made.
Intravascular large B-cell lymphoma is a rare, often aggressive extranodal lymphoma characterized by malignant involvement within the lumens of small vessels. The disease is challenging to diagnose owing to its nonspecific symptoms and signs (e.g., fever, fatigue, and absence of lymphadenopathy) and heterogeneous presentation. In this case, the patients isolated skin involvement was consistent with the cutaneous subtype of intravascular large B-cell lymphoma.
Treatment with systemic chemotherapy was initiated. At the 6-month follow-up visit, the patient continued to be in remission.
(11). Chun-Hao Lin. Toddlers Fracture. N Engl J Med 2023; 389:50
Case Presentation
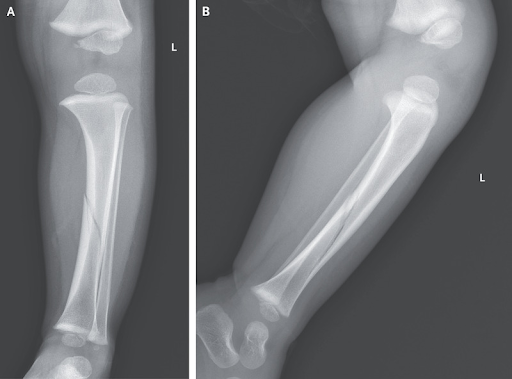
A previously healthy 20-month-old boy was brought to the emergency department with a 2-hour history of pain and swelling in the left lower leg. The pain had started immediately after he had twisted his leg and fallen to the ground when pushed by his sibling. On physical examination, the child was crying and unable to bear weight on the left leg. The left lower leg was tender to palpation and painful with passive dorsiflexion of the ankle. Radiographs of the left lower leg showed a minimally displaced spiral fracture of the tibial shaft (Panel A, anteroposterior view; Panel B, lateral view; L denotes left). A diagnosis of a toddlers fracture was made. Toddlers fractures are a type of spiral fracture of the tibia that occurs in children between the ages of early walking and preschool. Such fractures result from low-energy twisting movements or falls. Toddlers fractures are typically nondisplaced and thus radiographically subtle, unlike the fracture in this patient. Radiographically occult toddlers fractures often become more visible on repeat radiographs obtained 1 to 2 weeks after the initial injury. Treatment with splinting and analgesic agents was given, along with a recommendation to avoid weight-bearing activities. At the 6-week follow-up, the fracture had healed, allowing the child to engage in weight-bearing activities, and he subsequently resumed normal activities.
(12). Tetsuhiro Yoshino, et al. Sigmoid Volvulus. https://doi.org/10.7326/aimcc.2023.1059
Case Presentation
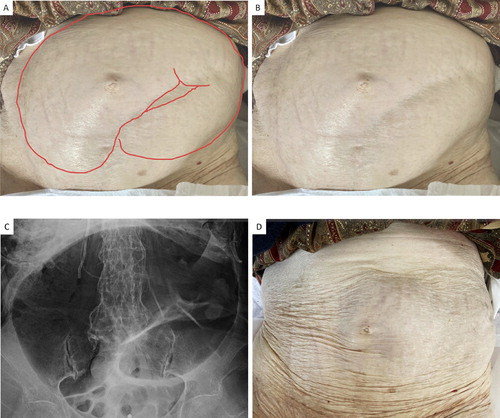
An 83-year-old woman who resided in a nursing home presented to the emergency department with abdominal pain and vomiting resulting in the diagnosis of sigmoid volvulus. She needed intermittent catheter reduction of the colonic air but no surgical intervention has been performed so far.An 83-year-old woman who resided in a nursing home presented to the emergency department with abdominal pain and vomiting for 1 hour after breakfast. She had chronic constipation, postendoscopic cannulation for common bile duct stones, type 2 diabetes, chronic atrial fibrillation, and history of myocardial infarction. On physical examination, 2 distended ridges running parallel from upper left to lower right were seen in the abdomen (Figure 1AandB) and intestinal peristalsis was apparent; there was no fever, melena, abdominal solid mass, or peritoneal signs such as rebound tenderness. A plain radiograph of the abdomen showed a coffee bean sign (Figure 1C) which is consistent with the diagnosis of sigmoid volvulus and computed tomography of the abdomen ruled out the perforation. Transanal air aspiration with a Foley catheter was performed, which resolved the distension (Figure 1D) and symptoms immediately. Afterward, we carefully observed her, sparing endoscopic or surgical management. She needed weekly intermittent catheter reduction of the colon for abdominal distension, but abdominal pain and vomiting have not occurred
Sigmoid volvulus is an uncommon cause of intestinal obstruction but can occur in older institutionalized adults with a history of constipation. Management of patients with sigmoid volvulus depends on the presence of intestinal perforation or peritonitis, and endoscopic detorsion could be applied as an initial management option in stable cases. A decompression with a Foley catheter could be an alternative and temporary measure for carefully selected poor surgical candidates with stable conditions like the presented case.
(13). David Ouyang et al. Electrocardiographic deep learning for predicting post-procedural mortality: a model development and validation study. The Lancet. DOI: https://doi.org/10.1016/S2589-7500(23)00220-0
Summary
Background
Preoperative risk assessments used in clinical practice are insufficient in their ability to identify risk for postoperative mortality. Deep-learning analysis of electrocardiography can identify hidden risk markers that can help to prognosticate postoperative mortality. We aimed to develop a prognostic model that accurately predicts postoperative mortality in patients undergoing medical procedures and who had received preoperative electrocardiographic diagnostic testing.
Methods
In a derivation cohort of preoperative patients with available electrocardiograms (ECGs) from Cedars-Sinai Medical Center (Los Angeles, CA, USA) between Jan 1, 2015 and Dec 31, 2019, a deep-learning algorithm was developed to leverage waveform signals to discriminate postoperative mortality. We randomly split patients (8:1:1) into subsets for training, internal validation, and final algorithm test analyses. Model performance was assessed using area under the receiver operating characteristic curve (AUC) values in the hold-out test dataset and in two external hospital cohorts and compared with the established Revised Cardiac Risk Index (RCRI) score. The primary outcome was post-procedural mortality across three health-care systems.
Findings
45969 patients had a complete ECG waveform image available for at least one 12-lead ECG performed within the 30 days before the procedure date (59975 inpatient procedures and 112794 ECGs): 36839 patients in the training dataset, 4549 in the internal validation dataset, and 4581 in the internal test dataset. In the held-out internal test cohort, the algorithm discriminates mortality with an AUC value of 083 (95% CI 079087), surpassing the discrimination of the RCRI score with an AUC of 067 (061072). The algorithm similarly discriminated risk for mortality in two independent US health-care systems, with AUCs of 079 (075083) and 075 (074076), respectively. Patients determined to be high risk by the deep-learning model had an unadjusted odds ratio (OR) of 883 (5571320) for postoperative mortality compared with an unadjusted OR of 208 (077350) for postoperative mortality for RCRI scores of more than 2. The deep-learning algorithm performed similarly for patients undergoing cardiac surgery (AUC 085 [077092]), non-cardiac surgery (AUC 083 [079088]), and catheterisation or endoscopy suite procedures (AUC 076 [072081]).
Interpretation
A deep-learning algorithm interpreting preoperative ECGs can improve discrimination of postoperative mortality. The deep-learning algorithm worked equally well for risk stratification of cardiac surgeries, non-cardiac surgeries, and catheterisation laboratory procedures, and was validated in three independent health-care systems. This algorithm can provide additional information to clinicians making the decision to perform medical procedures and stratify the risk of future complications.
Funding
National Heart, Lung, and Blood Institute.
(14). Eric J Topol. Machines and empathy in medicine. The Lancet. 2023;402(10411):1411
Digital Medicine
The human bond between patient and clinician is fundamental. But the patientdoctor relationship is affected by the limited time allotted for a clinic visit or bedside rounds and the way clinicians need to update electronic records during a consultation (figure A). Such factors can result in the perception that clinicians lack compassion and empathy. Artificial intelligence (AI) could help restore the essential humaneness in medicine, primarily by providing the gift of timethe premise of my 2019 book Deep Medicine. What might more time help achieve? The ability to listen to a patients story and deep concerns (figure B); the necessity of a careful physical examination, reinforcing human touch and trust; and the genuine sense of care and compassion that lies in direct contrast to what software or machines can offer.
AI could generate more time with patients in various ways. Large language models (LLMs) of clinic visit conversations could offload many data clerk functions, such as health insurance pre-authorisations, scheduling of follow-up visits, tests, and prescriptions. Meanwhile, the emergence of deep learning apps to screen for certain medical conditions, including heart arrhythmias, skin lesions, and urinary tract infections, could also free up clinician time. Additionally, patient autonomy has been extended via chatbots that answer medical questions, decompressing the need for direct contact with doctors and nurses (figure C). Other time-saving AI functions in development include the rapid synthesis and data visualisation for the complete medical records of a patient, the up-to-date review of the corpus of medical literature pertinent to an individual, and provision of a differential diagnosis. Beyond these initiatives, there is the longer-term expectation that some patients who are currently admitted to hospital could instead be monitored at home with validated multimodal AI algorithms. Such advances are likely to increase clinical efficiency and productivity. In these indirect ways AI could pave the way for more time for patients and doctors to come together.
What I did not anticipate when I wrote Deep Medicine was the potential for promotion of empathy by machines. For example, a 2023 study of 195 patient questions to the social media forum Reddits volunteer physicians and to ChatGPT showed the AI responses were 98 times more likely to be considered empathetic than the doctors responses. LLMs also have the capability to coach physicians. In their book The AI Revolution in Medicine: GPT-4 and Beyond Peter Lee, Carey Goldberg, and Isaac Kohane highlight such uses, including GPT-4 review of doctors performances with recommendations to ask more open-ended questions or be more sensitive to a patients concerns. Lee and coauthors propose that While an A.I. system might not ever be a replacement for the human touch in medicine, this response suggests A.I. could help doctors and nurses muster even more empathy and humanity [figure D] to engage well with their patients and also continue a path of growth and self-improvement.
Yet the challenge is that the machine promotion of empathy is actually pseudo-empathy. It is empathetic in appearance, but the AI cannot truly connect with the patient or share the experience. The LLM performs a task without understanding its meaning, parroting the text from the vast inputs of its training, and is one-dimensional because of its focus on words. By contrast, a physician can exude empathy in many non-verbal ways, including eye contact and holding hands. Another shortcoming is that current LLMs such as Bard, LLaMA, PaLM 2, and GPT-4, have not had specialised fine-tuning for medical inputs. Even though the ChatGPT compared with Reddit doctor study showed high quality and accurate responses, the questions informing the model were limited. Thus, there is a danger of mistaken answers and advice from these models, as has been seen with erroneous chatbot responses to diet questions from people with eating disorders. As LLMs improve and are trained with high-quality medical inputs, this problem may improve but is unlikely to be eradicated. Nevertheless, the potential of AI coaching clinicians to be more compassionate and sensitive by review of their patient interactions could emerge as a vital educational tool in the future, not only for medical students but for all health professionals.
(15). Amber Hsiao et al. Recombinant or Standard-Dose Influenza Vaccine in Adults under 65 Years of Age. N Engl J Med 2023; 389:224555
Abstract
Background
Quadrivalent recombinant influenza vaccines contain three times the amount of hemagglutinin protein as standard-dose egg-based vaccines, and the recombinant formulation is not susceptible to antigenic drift during manufacturing. Data are needed on the relative effectiveness of recombinant vaccines as compared with standard-dose vaccines against influenza-related outcomes in adults under the age of 65 years.
Methods
In this cluster-randomized observational study, Kaiser Permanente Northern California facilities routinely administered either a high-dose recombinant influenza vaccine (Flublok Quadrivalent) or one of two standard-dose influenza vaccines during the 20182019 and 20192020 influenza seasons to adults 50 to 64 years of age (primary age group) and 18 to 49 years of age. Each facility alternated weekly between the two vaccine formulations. The primary outcome was influenza (A or B) confirmed by polymerase-chain-reaction (PCR) testing. Secondary outcomes included influenza A, influenza B, and influenza-related hospitalization outcomes. We used Cox regression analysis to estimate the hazard ratio of the recombinant vaccine as compared with the standard-dose vaccines against each outcome. We calculated the relative vaccine effectiveness as 1 minus the hazard ratio.
Results
The study population included 1,630,328 vaccinees between the ages of 18 and 64 years (632,962 in the recombinant-vaccine group and 997,366 in the standard-dose group). During this study period, 1386 cases of PCR-confirmed influenza were diagnosed in the recombinant-vaccine group and 2435 cases in the standard-dose group. Among the participants who were 50 to 64 years of age, 559 participants (2.00 cases per 1000) tested positive for influenza in the recombinant-vaccine group as compared with 925 participants (2.34 cases per 1000) in the standard-dose group (relative vaccine effectiveness, 15.3%; 95% confidence interval [CI], 5.9 to 23.8; P=0.002). In the same age group, the relative vaccine effectiveness against influenza A was 15.7% (95% CI, 6.0 to 24.5; P=0.002). The recombinant vaccine was not significantly more protective against influenza-related hospitalization than were the standard-dose vaccines.
Conclusions
The high-dose recombinant vaccine conferred more protection against PCR-confirmed influenza than an egg-based standard-dose vaccine among adults between the ages of 50 and 64 years. (Funded by Sanofi)
(16). V. Ruxandra Moroti Constantinescu et al. Acute Human Immunodeficiency Virus Infection. N Engl J Med 2023; 389:2276
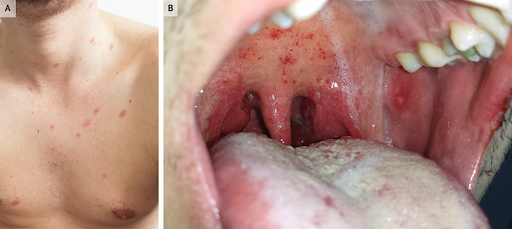
A previously healthy 26-year-old man presented to the emergency department with a 5-day history of an asymptomatic rash, sore throat, fevers, chills, and malaise. On physical examination, scattered, erythematous papules and macules could be seen across the upper chest and anterior neck (Panel A). In the mouth, palatal petechiae, buccal mucosal ulcerations, and pharyngeal erythema were observed (Panel B). There was no palpable lymphadenopathy. Laboratory testing showed leukopenia, lymphopenia, mild thrombocytopenia, and an elevated C-reactive protein level. Tests for several respiratory viral pathogens, EpsteinBarr virus, measles, rubella, and syphilis were negative. A rapid antibody test for human immunodeficiency virus (HIV) was negative. However, a subsequent fourth-generation combination HIV antigen and antibody test was positive, and the HIV viral load was greater than 10 million copies per milliliter (reference value, undetectable). A diagnosis of acute HIV infection was made. The patient reported having had condomless sex with a new partner 2 weeks before presentation. In acute HIV infection, HIV antibodies do not form until several weeks after infection, whereas HIV viremia and the p24 antigen are detectable much earlier. Antiretroviral therapy was started, and the patients symptoms rapidly abated.
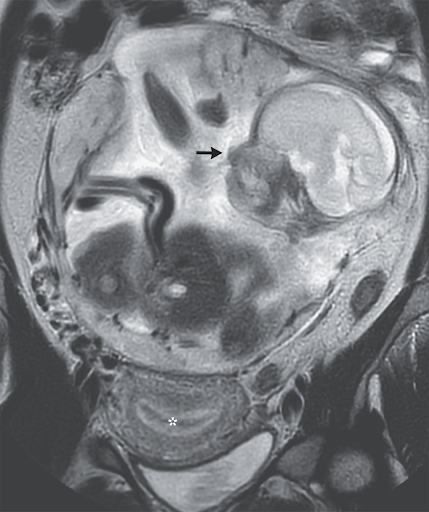
(17). Guillaume Gorincour et al. Abdominal Ectopic Pregnancy. N Engl J Med 2023;389:51
Case Presentation
A 37-year-old woman who lived on a remote island presented to the emergency department with a 10-day history of abdominal pain. She had a history of two vaginal deliveries at full term, one miscarriage, and no sexually transmitted infections or previous surgeries. The physical examination was notable for a gravid abdomen. Ultrasonography revealed a thickened endometrium, empty uterus, and abdominal pregnancy at 23 weeks gestation. Magnetic resonance imaging of the abdomen subsequently showed a nongravid uterus (asterisk), a normally formed intraabdominal fetus (arrow), and a placenta that attached to the peritoneum above the sacral promontory. A diagnosis of abdominal pregnancy a rare type of ectopic pregnancy was made. Owing to the high risk of maternal hemorrhage and fetal demise, the patient was transferred to a tertiary care hospital. At 29 weeks gestation, a laparotomy with infant delivery, placental arterial embolization, and partial removal of the placenta was performed. The baby, who had Apgar scores of 2 and 6 at 1 minute and 5 minutes, respectively, was admitted to the neonatal intensive care unit. On postoperative day 12, the remaining placenta was surgically removed. The mother and the baby were discharged home 25 days and 2 months, respectively, after the birth. The mother, who had declined contraception post partum, was lost to follow-up.
(18). Fatema Mollah et al. What Is Alpha-Gal Syndrome? JAMA. 2023; doi:10.1001/jama.2023.23097
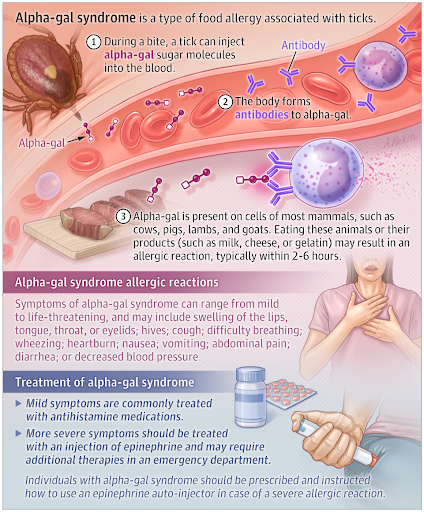
Background
Alpha-gal syndrome is a type of food allergy to mammalian (red) meat products.
Alpha-gal syndrome is associated with tick bites, most commonly from the Lone Star tick in the US, but also from different types of ticks in other areas of the world. During a bite, a tick injects a type of sugar molecule (galactose-alpha-1,3-galactose), also called alpha-gal, which leads to formation of an antibody. Because alpha-gal is present on cells of most mammals, including cows, pigs, lambs, and goats, when affected individuals eat these animal products, an allergic reaction may occur.
What Are the Symptoms of Alpha-Gal Syndrome?
Alpha-gal allergic reactions can range from mild to life-threatening (anaphylaxis) and typically occur about 2 to 6 hours after ingestion of mammalian meat or other mammalian products (such as cows milk, cheese, or gelatin). Symptoms may include hives; swelling of the lips, tongue, throat, or eyelids; cough; difficulty breathing; wheezing; heartburn; nausea or vomiting; abdominal pain; diarrhea; or decreased blood pressure.
How Common Is Alpha-Gal Syndrome and Who Is Affected?
In the US, 110 000 cases of alpha-gal syndrome were reported from 2010 to 2022; however, many more cases were likely undiagnosed and/or unreported. Alpha-gal syndrome is most frequently diagnosed in the southern, central, and eastern US, but cases have been reported across the US and worldwide. Alpha-gal syndrome can affect both children and adults.
How Is Alpha-Gal Syndrome Diagnosed and Treated?
The diagnosis of alpha-gal syndrome is made when individuals have a delayed allergic reaction to red meat or other mammalian products and blood testing reveals an antibody against the alpha-gal sugar molecule. Mild alpha-gal allergic symptoms are commonly treated with an antihistamine medication. More severe reactions are treated with an intramuscular injection of epinephrine and may require additional therapies in the emergency department. Individuals diagnosed with alpha-gal syndrome are typically prescribed an epinephrine auto-injector to use if they develop a severe allergic reaction.
An individual with alpha-gal syndrome should completely stop eating mammalian meat (such as beef, pork, or lamb) and should be vigilant to avoid future tick bites. Some individuals may also need to stop ingesting mammalian-based products (such as cows milk, cheese, or gelatin). Certain medications, such as a blood thinner (heparin), snake antivenom, and certain cancer medications (such as cetuximab), as well as mammal-based organ replacements (such as heart valves) can cause allergic reactions in patients with alpha-gal syndrome and should be avoided.
How to Prevent Alpha-Gal Syndrome
Alpha-gal syndrome can be prevented by avoiding grassy, brushy, and wooded areas where ticks often live. Individuals who are outdoors in these areas should walk in the center of trails, use Environmental Protection Agency (EPA)registered insect repellants, wear clothing that covers exposed skin, and apply insecticide (permethrin) to clothing and gear. After coming indoors, individuals should check their skin and clothing for ticks. If a tick is found on the body, it should be removed using fine-tipped tweezers to grasp the tick close to the skin and pull upward with steady, even pressure.
(19). Jason W Busse et al. Management of chronic pain associated with temporomandibular disorders: a clinical practice guideline. BMJ. 2023;383:076227
Abstract
Clinical question: What is the comparative effectiveness of available therapies for chronic pain associated with temporomandibular disorders (TMD)?Current practiceTMD are the second most common musculoskeletal chronic pain disorder after low back pain, affecting 6-9% of adults globally. TMD are associated with pain affecting the jaw and associated structures and may present with headaches, earache, clicking, popping, or crackling sounds in the temporomandibular joint, and impaired mandibular function. Current clinical practice guidelines are largely consensus-based and provide inconsistent recommendations.RecommendationsFor patients living with chronic pain (≥3 months) associated with TMD, and compared with placebo or sham procedures, the guideline panel issued: (1) strong recommendations in favour of cognitive behavioural therapy (CBT) with or without biofeedback or relaxation therapy, therapist-assisted mobilisation, manual trigger point therapy, supervised postural exercise, supervised jaw exercise and stretching with or without manual trigger point therapy, and usual care (such as home exercises, stretching, reassurance, and education); (2) conditional recommendations in favour of manipulation, supervised jaw exercise with mobilisation, CBT with non-steroidal anti-inflammatory drugs (NSAIDS), manipulation with postural exercise, and acupuncture; (3) conditional recommendations against reversible occlusal splints (alone or in combination with other interventions), arthrocentesis (alone or in combination with other interventions), cartilage supplement with or without hyaluronic acid injection, low level laser therapy (alone or in combination with other interventions), transcutaneous electrical nerve stimulation, gabapentin, botulinum toxin injection, hyaluronic acid injection, relaxation therapy, trigger point injection, acetaminophen (with or without muscle relaxants or NSAIDS), topical capsaicin, biofeedback, corticosteroid injection (with or without NSAIDS), benzodiazepines, and blockers; and (4) strong recommendations against irreversible oral splints, discectomy, and NSAIDS with opioids.–
(20). Zosia Kmietowicz. NICE lowers cholesterol target for people with cardiovascular disease. BMJ 2023;383:2946
Doctors should aim to reduce low density lipoprotein (LDL) cholesterol levels among people with cardiovascular disease to 2.0 mmol/L or less, or non-high density lipoprotein (HDL) cholesterol levels to 2.6 mmol/L or less, the National Institute for Health and Care Excellence (NICE) has advised.
(21). Stefan Sauerland et al. Managing symptomatic gallstone disease. BMJ. 2023;383:2624
We must move away from a one size fits all approach
Symptomatic gallstone disease (cholelithiasis) is the classic indication for elective cholecystectomy.1 In addition to relieving symptoms, cholecystectomy reduces the risk of gallstone related complications such as acute cholecystitis, cholangitis, and pancreatitis. Since the late 1980s, when the advent of laparoscopic surgery reduced postoperative morbidity and enabled outpatient surgery,2 the threshold for surgery has been lowered. Today, cholecystectomy has largely replaced alternative interventions such as shock wave lithotripsy and bile salt dissolution treatment,3 and it is now one of the most commonly performed surgical procedures, resulting in high costs for healthcare systems.
The clinical indication for and the timing of surgery, however, remains a grey area. In general, about 20% of patients with a first episode of biliary colic undergo cholecystectomy,4 but some experts argue that all patients with definite symptoms should have their gallbladder removed quickly.
(22). Marcel H A Muskie et al. Diabetes care in older people: a call for action. The Lancet. 2023;4(12):65759
Few areas of medicine have changed as much in the past 25 years as the field of pharmacotherapy for type 2 diabetes. Diabetes management has seen a shift from a traditional strategy that emphasises lowering glycated haemoglobin A1C (HbA1c) as the primary consideration in therapy selection to prevent microvascular complications, to a more holistic approach that seeks to tailor the pharmacotherapeutic regimen to the specific characteristics of each patient.1 Presence or risk for atherosclerotic cardiovascular disease, chronic kidney disease, and heart failure, as well as patients needs, preferences, values, socioeconomic determinants of health, barriers to care, susceptibility to adverse effects, comorbidities or competing illnesses, and life expectancy are now all considered alongside HbA1c when designing the most appropriate management plan.1
This change in approach resulted largely from the rise in available glucose-lowering drugs, and the US Food and Drug Administrations 2008 regulatory requirements for conducting rigorous long-term cardiovascular outcome trials to establish these drugs cardiovascular safety.2 Since 2015, cardiovascular outcome trials conducted with several GLP-1 receptor agonists and SGLT2 inhibitors yielded important results in patients with type 2 diabetes at high risk of cardiovascular disease.3 Aside from their glucose-lowering efficacy and cardiovascular safety, these new-generation glucose-lowering drug classes conferred protection against major adverse cardiovascular events, decreased the risk of chronic kidney disease and admission to hospital for heart failure, and reduced cardiovascular and all-cause mortality compared with the standard of care at the time.3 These benefits occurred after only a few years of treatment, irrespective of the patients glycaemic control and without independently increasing hypoglycaemia risk, which highlights that improved outcomes might be determined not only by the degree of HbA1c reduction achieved, but also by the choice of drugs used to achieve that reduction.2, 3 In recognition of this concept and results, diabetes-related guidelines have undergone frequent revisions since 2018 to keep abreast of the rapidly evolving evidence. Although metformin remains the preferred initial drug for management of type 2 diabetes in most guidelines, the American Diabetes Association and the European Association for the Study of Diabetes now recommend a GLP-1 receptor agonist or SGLT2 inhibitor (or both) as add-on therapies in patients with or at high risk for atherosclerotic cardiovascular disease, chronic kidney disease, or heart failure.1 The more traditional glucose-lowering medications, such as sulfonylureas and insulin, have since been deprioritised due to their increased risk of causing hypoglycaemia, which in turn is associated with a risk of acute and long-term cognitive impairment, injurious falls, frailty, and myocardial infarction and mortality, particularly in older patients.4, 5
A patient-centred and outcomes-driven approach to diabetes management, and the availability of new-generation drugs (which have relatively short times to benefit), are hopeful developments for older (>65 years) patients with type 2 diabetes, who comprise a large and growing proportion of patients with diabetes worldwide. Diabetes care in older patients requires careful individualisation, as it faces unique challenges linked to the age-related changes in pharmacokinetics and pharmacodynamics, and these patients substantial heterogeneity in clinical, cognitive, and functional status.4, 5 Theoretically, older patients are the group that are likely to benefit most from GLP-1 receptor agonists and SGLT2 inhibitors, given their increased risk of cardiovascular or renal disease. Post-hoc analyses of cardiovascular outcome trials and emerging real-world evidence have shown similar or even greater cardiovascular benefits of GLP-1 receptor agonists and SGLT2 inhibitors in patients who are older or frail, along with improvements in symptoms, physical function, and quality of life.6 Although guidelines recommend less strict glycaemic control for older patients,4, 5 none suggest using different drugs than for younger patients. However, the American Diabetes Association4 and American Geriatrics Society7 recommend minimising the use of drugs that can cause hypoglycaemia, such as sulfonylureas and insulin, rendering GLP-1 receptor agonists and SGLT2 inhibitors the more attractive treatment options.
Paradoxically, in The Lancet Healthy Longevity, Karl Sebastian Johansson and colleagues8 report in a nationwide Danish cohort of 290 890 people with type 2 diabetes between 2019 and 2020, that the uptake of GLP-1 receptor agonists and SGLT2 inhibitors in the real world has not been consistent across all age groups, particularly disadvantaging older people. After adjusting for relevant confounders (ie, socioeconomic factors, renal function, and several comorbidities), older patients (>80 years) were 55% less likely to receive GLP-1 receptor agonists or SGLT2 inhibitors compared with their younger counterparts. Conversely, older patients were 65% more likely to be treated with insulin and sulfonylureas despite the increased risk of hypoglycaemia, and despite having low HbA1c (sometimes even <6%, which is indicative of overtreatment). These surprising prescription patterns are in line with another Danish cohort involving patients who are frail.6 The underuse of evidence-based drugs in older patients raises some concerns, and warrants examination of potential factors or barriers at the clinician and patient level that could explain the apparent age-related hesitancy towards guideline-concordant prescribing. Although the underuse of these drugs could be the consequence of reasonable caution or a well considered rational decision by the prescribing clinician, it could also be driven by factors that can be modified or resolved to ultimately improve care in older patients.
Among the principal factors associated with reduced prescription of drug therapies in older patients are fears of adverse events (ie, placing a greater emphasis on risk than benefit) and scarce age-specific evidence from clinical trials. Indeed, older patients, particularly those who have evidence of functional loss, frailty, and cognitive impairment, are under-represented in current trials leading to management guidelines that largely rely on extrapolations and expert opinions.9 The current cardiovascular outcome trials were done in carefully selected patients with a mean age of 6266 years, and only a small proportion of patients older than 65 years were recruited.9 Implementation of practices on the basis of these findings in older populations therefore might not yield the desired effectiveness and safety in older or very-old age groups. Concerns with SGLT2 inhibitors relate to the potential risk of volume depletion, genital mycotic infections, and fractures, which are all particularly pertinent in older people. Also, the effect of weight loss and gastrointestinal side-effects with GLP-1 receptor agonists on sarcopenia, bone mass, and falls in frail or underweight older patients is yet to be studied. Post-hoc analyses of outcome trials can alleviate some of these concerns and have shown that adverse events were not more common in older or frail patients than in younger patients, but additional real-world evidence is needed.6 Also, the 2020 guidance from the US Food and Drug Administration10 for evaluating the safety of new drugs for type 2 diabetes will help to improve enrolment of participants older than 65 years (the guidance recommends that studies provide safety data from at least 600 people in this age group) and people with comorbidities (eg, stage 3 or 4 chronic kidney disease, or established cardiovascular disease) in new trials for glucose-lowering drugs. However, we stress the risk of ageism; chronological age is not a specific risk factor for adverse drug events and should not be the defining factor in therapeutic decision making.
The suggestion that the prescription pattern in Johansson and colleagues study might partly be due to older patients treatment being initiated before marketing of the new-generation drugs warrants attention. Individualisation of care should be supported by periodic rereviews, not only to identify changes in patient characteristics over time, but also to look for new developments that might better suit the needs of the patient. Being satisfied with a patients HbA1c and tolerability does not justify endless drug prescribing. Reducing the drugs prescribed to avoid unnecessary medication and polypharmacy, or the prescription of medication associated with harm (such as hypoglycaemia and hypotension), are important considerations for older patients.3, 4
The rapidly expanded therapeutic armamentarium and frequent guideline updates could overwhelm clinicians, leading to uncertainty, decision paralysis, and therapeutic inertia. Primary care physicians might also be slow in making therapeutic changes due to different patient selections and slower developments in primary care guidelines, which could possibly explain the disparity in medication use between health-care sectors at the time of the study (201920) in Denmark.8 Reanalysing data from real-world evidence (with the understanding that new prescriptions are rapidly increasing and experience in their use is expanding) for both younger and older populations, tackling remaining gaps in knowledge, and addressing clinical inertia is paramount to resolve this disparity.
The current study highlights that despite having increased opportunities to pharmacologically improve patients lives, several known (and unknown) factors still hinder the prescription of guideline-recommended medications for older patients with type 2 diabetes, and will need to be addressed more strongly. Calling for a broader use of GLP-1 receptor agonists and SGLT2 inhibitors in older patients with type 2 diabetes is reasonable, given their cardiorenal benefit and reduced hypoglycaemia risk. However, caution is still advised when individualising treatment plans, as more efficacy, safety, and cost-effectiveness data are needed for this heterogeneous population to develop the evidence base for true clinical guidance. With these data and additional relevant geriatric outcomes being expected to emerge soon, clinicians have both the ability and the responsibility to integrate the wealth of this newfound evidence into everyday clinical practice.
(23). Marek Lommatzs et al. Pioneering a paradigm shift in asthma management: remission as a treatment goal. The Lancet. 2023. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(23)00415-0/fulltext
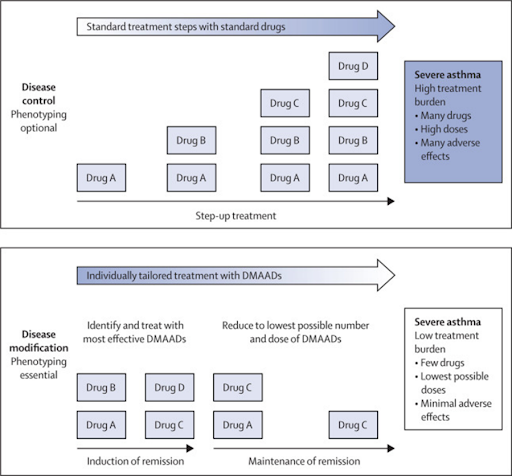
Until 2023, guidelines focused on asthma control as the primary goal of asthma treatment, 1 with the step-wise addition of drugs until the best possible disease control was achieved (figure). Phenotyping was optional. One drug could simply be added to another following the standard scheme, with treatment failure rather than the presence of a particular characteristic being the stimulus for treatment escalation. The more severe the disease, the more drugs in increasing doses were given. Patients with severe asthma were, therefore, treated with multiple drugs at high doses, often with substantial side-effects. With the availability of highly effective, anti-inflammatory disease-modifying anti-asthmatic drugs (DMAADs)for example, treatments containing inhaled corticosteroids (ICS), biologics, or allergen immunotherapiesasthma management has changed fundamentally. The new concept of disease modification does not warrant the simple addition of one drug to another, but the identification of the right DMAAD(s) for the right patient at the right time. According to this new concept, phenotyping is an essential prerequisite to establish individually effective treatment (figure).
(24).The promise of genetic therapies in sickle cell disease. The Lancet. 2023;402(10419):2265
The eagerly awaited news that the US Food and Drug Administration (FDA) had approved two gene therapies for sickle cell disease, including the first CRISPR-based treatment for any disorder, was announced on Dec 8. The treatmentsexagamglogene autotemcel (exa-cel) and lovotibeglogene autotemcel (lovo-cel)were approved for use in patients aged 12 years or older with a history of vaso-occlusive events. Genetic therapies are potentially transformative for people with sickle cell disease, who continue to be neglected and discriminated against due to the disease disproportionately affecting Black people. Coming a little over a decade since the initial discovery of CRISPR, the success of genetic therapies is also a triumph for science and medicine. However, substantial barriers will need to be overcome if the prospect of a cure for sickle cell disease is to become a reality for all patients.
Affecting an estimated 77 million people worldwide, sickle cell disease is a chronic, debilitating disorder that causes severe pain, organ damage, reduced quality of life, and a shorter life expectancy when compared with the general population. The only proven cure is a stem-cell transplant from a matched donor, but morbidity can be high and a paucity of donors limits the availability of allotransplantation. The newly approved therapies involve extraction, genetic modification, and reinfusion of a patients own haematopoietic stem cells. While lovo-cel works in a conventional manner by using a lentiviral vector to deliver a modified -globin gene into the cells, exa-cel harnesses CRISPR technology to deactivate the BCL11A gene, which, in turn, restarts production of normal fetal haemoglobin and inhibits the polymerisation of sickled haemoglobin.
Both therapies were highly effective in clinical trials, showing a complete resolution of vaso-occlusive crises for at least 12 months in more than 90% of patients treated. However, genetic therapies cannot reverse existing damage and it is premature to consider these therapies as curative until long-term data are availableincluding whether the therapies can prevent chronic kidney disease or eliminate the need for kidney transplantation. Although off-target genome editing was not seen in the clinical trials of exa-cel, the risk of off-target editing cannot be ruled out due to individual genetic variation. Two patients treated with an earlier version of lovo-cel developed acute myeloid leukaemia and the FDA label includes a black-box warning that patients taking lovo-cel must be monitored closely for evidence of malignancy every 6 months.
The FDAs approval follows the world-first approval of exa-cel in the UK on Nov 16. A decision from the National Institute for Health and Care Excellence on whether exa-cel will be available on the NHS is expected in March, 2024. In the USA, exa-cel has a price tag of US$22 million and lovo-cel $31 million. Factoring in other associated costs, such as myeloablative conditioning with busulfan, the lengthy in-hospital stays required, and access to psychological support, overall treatment costs are likely to be substantially greater. However, the high initial cost of genetic therapies must be weighed against the lifetime costs of managing the disease in people with recurrent vaso-occlusive crises, which are estimated to reach up to $6 million in the USA. According to 2021 data, a majority of the estimated 100 000 people with sickle cell disease in the USA are covered by public health insurance; any decision on eligibility is thus likely to depend on the number and severity of vaso-occlusive events. Infertility can occur with myeloablative conditioning, yet public insurance in most US states does not cover fertility preservation. Whether private health insurers are willing to pay such a hefty price is unclear.
Because genetic therapies require the infrastructure and expertise to perform stem-cell transplantation, they are currently out of reach in much of sub-Saharan Africa and India, where most people with sickle cell disease live. Many countries even have patchy access to hydroxyurea, which reduces the incidence of vaso-occlusive episodes. In these settings, as highlighted in the recent Lancet Haematology Commission, it is important to continue to focus on practical goals, such as newborn screening for early diagnosis, penicillin prophylaxis and vaccination, education, and expanding availability of hydroxyurea.
The speed of progress in CRISPR technology is unparallelled in science, and genetic therapies have immense potential to transform the lives of people with serious monogenic disorders. Medical breakthroughs such as these also bring unique social and ethical dilemmas. The challenge now is of equity and accessibility: ensuring these transformative therapies are available to everyone who needs them.
(25). Jeanne Rini Poespoprodj et al. Malaria. The Lancet. 2023;402(10419):232845
Summary
Malaria is resurging in many African and South American countries, exacerbated by COVID-19-related health service disruption. In 2021, there were an estimated 247 million malaria cases and 619000 deaths in 84 endemic countries. Plasmodium falciparum strains partly resistant to artemisinins are entrenched in the Greater Mekong region and have emerged in Africa, while Anopheles mosquito vectors continue to evolve physiological and behavioural resistance to insecticides. Elimination of Plasmodium vivax malaria is hindered by impractical and potentially toxic antirelapse regimens. Parasitological diagnosis and treatment with oral or parenteral artemisinin-based therapy is the mainstay of patient management. Timely blood transfusion, renal replacement therapy, and restrictive fluid therapy can improve survival in severe malaria. Rigorous use of intermittent preventive treatment in pregnancy and infancy and seasonal chemoprevention, potentially combined with pre-erythrocytic vaccines endorsed by WHO in 2021 and 2023, can substantially reduce malaria morbidity. Improved surveillance, better access to effective treatment, more labour-efficient vector control, continued drug development, targeted mass drug administration, and sustained political commitment are required to achieve targets for malaria reduction by the end of this decade.
(26). Durairaj Arjunan et al. Thyroid Dermopathy in Graves Disease. N Engl J Med 2023;389:2376

Case Presentation
A 49-year-old woman with a history of Graves disease presented to the endocrinology clinic with a 3-year history of skin changes on her arms and legs and a 1-year history of thyrotoxicosis symptoms. She had intermittently adhered to carbimazole therapy since her diagnosis 10 years earlier. On physical examination, violaceous, nonpitting, indurated nodules were observed on the dorsa of her hands, distal forearms, and shins (Panel A). A goiter (Panel B, arrow), proptosis, and lid lag were also noted. Laboratory testing showed an undetectable thyrotropin level and elevated total and free thyroxine and triiodothyronine levels. Testing for thyrotropin receptor and antithyroid peroxidase antibodies was positive. A skin biopsy of the pretibial region revealed nodular deposition of mucin with elastotic degeneration. A diagnosis of thyroid dermopathy in Graves disease was made. Thyroid dermopathy results from the accumulation of glycosaminoglycans in the dermis. Although the pretibial area is the most frequently involved site, thyroid dermopathy may occur on the feet, arms, and upper back. A biopsy is not typically needed for diagnosis. A total thyroidectomy was performed, after which levothyroxine therapy was given. Topical and intralesional glucocorticoid treatment was administered for the skin lesions. Ten months later, the patients symptoms had abated.

