Ventricular Septal Defect (VSD): Echocardiography
Vishalini
Cardiac Technician, Kauvery Heartcity, Trichy
Background
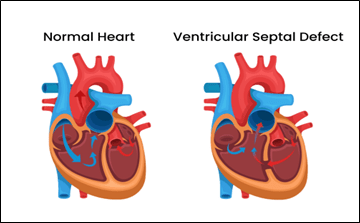
Ventricular septal defect (VSD) — also known as a “hole in the heart” — is a congenital heart defect. It involves a hole in the wall between the heart’s lower chambers.
Ventricular septal defects can be further described by;
1) Size of the defect,
2) Location of the defect,
3) Whether there is more than one defect present,
4) The presence or absence of a ventricular septal aneurysm.
The size of the defect is usually described as small, moderate, or large. In general, small defects cause no symptoms during infancy or childhood and often close spontaneously. Moderate and large defects are less likely to close spontaneously, may result in congestive heart failure, and more often require surgical closure.
Ventricular septal defects also occur in association with more complex heart defects such as Tetralogy of Fallot and transposition of the great vessels. It may also occur as a single component of a wide variety of intracardiac anomalies, including Tetralogy of Fallot (TOF), complete atrioventricular (AV) canal defects, transposition of the great arteries, and corrected transpositions.
Types of VSD
There are four basic types of VSD
1- Perimembranous VSD: Perimembranous ventricular septal defects (also called membranous VSD’s) are located in the membranous septum, a relatively small portion of the septum located near the heart valves.
Perimembranous VSD’s are observed as septal dropout in the area adjacent to the septal leaflet of the tricuspid valve and below the right border of the aortic annulus. They are further subdivided into one of the 4 types of perimembranous VSD
- Type A: VSD with absent aortic rim
- Type B: VSD with thick aortic margin
- Type C: VSD with membranous septal aneurysm
- Type D: Defects restricted by tricuspid valve attachments


2- Muscular VSD: This is a hole in the lower, muscular part of the ventricular septum and is the most common type of ventricular septal defect.
Muscular VSDs, may be found anywhere in the muscular intraventricular septum – apical, anterior, midmuscular, or posterior. Doppler color flow mapping is very helpful for identifying muscular defects.

3- Atrioventricular canal (Inlet VSD): It occurs posterior and superior between the annulus of the tricuspid valve and the attachments of the tricuspid valve to the ventricular septum.

4- Subpulmonic (Supracristal, infundibular, doubly committed subarterial, outlet VSD): It located below the aortic and pulmonary valves in the outlet of the septum of the right ventricle.

Electrocardiographic changes
The ECG changes reflect the size of shunt and degree of pulmonary hypertension
- left atrial overload – broad notched P wave
- Left ventricular overload – Deep ‘Q’ wave, tall ‘R’ wave, tall ‘T’ wave in lead V5 and V6
- Atrial fibrillation can also be seen
- Large VSD will produce right ventricular hypertrophy with right axis deviation

Impression
- Right atrial enlargement (peaked P waves in lead II)
- Left atrial enlargement (biphasic P waves in lead v3R)
- Biventricular hypertrophy
Echocardiographic evaluation:
- Determine the location & size of the heart
- Establishing the number of defects
- Measurement of defect margins
- Guidance of interventional and surgical treatment
Classification: Based on size
- Small VSD: Defect size is less than one- third of the size of aortic root.
- Moderate VSD: Defect size is less than one- half of the size of aortic root.
- Large VSD: Defect size is equal to or larger than the size of aortic root.
Diagnostic imaging
Electrocardiogram
This quick and painless test records the electrical activity of the heart. It can show how fast or how slowly the heart is beating.
Chest x-ray
It may indicate left atrial enlargement, right ventricular hypertrophy, left ventricular hypertrophy or pulmonary artery enlargement.
Echocardiogram
This is the most commonly used test to diagnose a ventricular septal defect. Sound waves are used to create pictures of the heart in motion. It Determines location & size.
Transesophageal Echocardiogram (TEE)
It’s a picture taken by numbing the throat and then sliding a thin tube containing an ultrasound device down the throat and into the esophagus, close to the heart.
Cardiac magnetic resonance imaging (MRI) scan:
Magnetic fields and radio waves are used to create detailed images of the heart. A health care provider might request this test if more information is needed after an echocardiogram.
Treatment
Ventricular septal defect treatment may include regular health checkups, medications and surgery. Many babies born with a small ventricular septal defect (VSD) won’t need surgery to close the hole. Some small VSDs close on their own.
If the VSD is small, regular health checkups may be all that’s needed. Medication may be prescribed to treat any symptoms.
Babies who have large VSDs or who tired easily during feeding may need extra nutrition to help them grow. Some babies may require medication to help treat heart failure symptoms.
Medications
Medications won’t repair a ventricular septal defect, but they may be given to treat symptoms or complications. The specific medications used depend on the symptoms and their cause. Water pills (diuretics) are used to decrease the amount of fluid in the body and reduce the strain on the heart.
Ventricular Septal Defect (Device Closure), with a Case example:
Case presentation 1
Baby of Saravanavel was diagnosed with a VSD issue when he was just 15 days old. His parents consulted pediatric cardiologist, and was on regular check-ups & follow ups.
When he was 6 Years old, his health condition was discussed with Consultant Pediatric Cardiologist. After carefully examining the entire situation, pediatrician advised VSD device Closure surgery for the child.
The VSD causes lots of issues / complications to the patients, therefore, it necessitates immediate medical attention. However, the patient’s family showed complete faith in the doctor’s prognosis and agreed for the surgery.
After the successful completion of VSD Device Closure Surgery, the patient and his family were happy seeing the minimally invasive procedure leaving no marks on his body. He was discharged within a couple of days and is now doing well in his life.
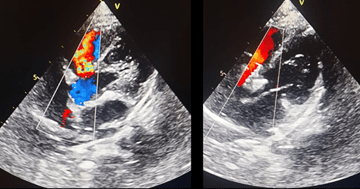
Echocardiography: five-chamber view with VSD, from preoperative.
VSD:ventricular septal defect; occluder: the device closed the defect without residual shunt.
Ventricular Septal Defect (Surgical Closure), with a Case example:
Case presentation 2
Baby Prashitha was born, there were no indications that she was anything but a healthy baby. But Prashitha’s family noticed she had trouble with feedings. She tired easily and at most feedings would only drink an once or two.
At Pranitha’s one-month check-up, her parents asked his pediatrician about the frequent feedings and if anything was wrong with their daughter. The pediatrician heard a murmur and performed an echocardiogram to look at Pranitha’s heart.
She was diagnosed with a ventricular septal defect (VSD), a hole in the heart lower chambers. After this diagnosis, doctors monitored her heart with fetal echocardiograms, waiting to see if the hole would close on its own.
When VSD openings are small, they can close naturally as the baby’s heart grows. When the VSD openings are large — and if they don’t close naturally — surgery is required.
After one month, the VSD hadn’t closed. Because of its shape and location, the VSD was unlikely to close & that their baby would need surgery.
A few weeks later, the family came to hospital, would perform the procedure.
During Pranitha’s open-heart surgery, doctor placed a small patch to close the hole between the left and right ventricles of heart.
The procedure was a success, and Pranitha remained in the Hospital for a few days to recover and help her body heal. At first she had some pain. Her condition continued to improve.
Within a few weeks she was really fine.
There are no restrictions on her activities. She will visit her primary cardiologist once a year.

Echocardiography: five-chamher view with VSD, from preoperative.
Surgical repair of ventricular septal defect.
Post repair follow-up
- Residual/additional VSDs
- RV pressure
- Abnormalities of adjacent valves
- Monitor LV size and function
Conclusion
Echocardiography is the method of choice for the first diagnosis and follow-up of VSDs, allowing assessment of both morphological characteristics and hemodynamic data as well as rule out late complications of both repaired and unrepaired defects. Integration of novel techniques including 3D TTE and speckle tracking echocardiography permits early detection of LV dysfunction and better defect sizing.

Vishalini
Cardiac Technician

