The future of advanced cardiology.
The Kauvery heart failure and transplantation centre provides comprehensive multidisciplinary care for heart failure patients to promote and restore their quality of life. The highly qualified team of heart transplant surgeons and supportive staff including the specialised heart failure nurses will strategise a personalised care plan taking into account the co-morbidities. The treatment offered takes a comprehensive approach to healing the heart starting from diet, exercise, and psychosocial help to medications, device implants and heart transplants.
Advantages of the Heart Failure and Transplantation Centre

- The safest facility for complex cardiac procedures according to European and American Standards
- Dedicated heart emergency department with internationally skilled cardiologists
- Dedicated Cardiac ICU and CCU
- Specialised cardiac electrophysiology and interventional cardiology team
Heart Transplant Specialists at Kauvery Hospital, Chennai
Book an Appointment
The Hybrid Cath Lab Operating Room
Kauvery Hospital houses India’s first flex-arm hybrid cath lab operating room. A one of its kind technology that boosts clinical precision and accuracy. It is the safest facility for complex cardiovascular interventions according to American and European guidelines and standards…

Frequently Asked Questions About Heart Transplantation
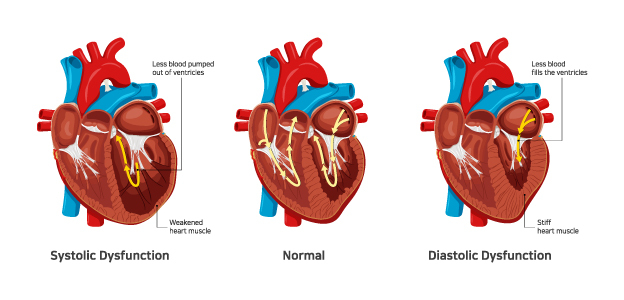
One in five people will develop heart failure, a life-threatening condition where the heart is unable to pump enough blood around the body. There are two types of heart failure:
- Systolic: A condition where the heart muscle is weakened. This usually happens when the left ventricle is enlarged and can’t contract the way it should. As a result, it can’t pump with enough force to push blood through the body.
- Diastolic: A condition where the heart muscle is stiff and unable to relax or contract properly. As a result, the heart can’t fill up with enough blood, which reduces the amount of blood pumped through the body.
If your heart issues don’t respond to treatment with medications, devices or other surgeries, you may be a candidate for a heart transplant. In a heart transplant, the diseased heart is replaced with a healthy, working heart from a donor.
Our heart failure team works with you and your family to treat and monitor your condition. From lifestyle changes like diet and exercise to medications, device implants and transplants, we personalize a care plan that best meets your needs.

Cardiomyopathy is a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure.
The main types of cardiomyopathy include
Dilated Cardiomyopathy: The main pumping chamber of the heart – left ventricle — becomes enlarged (dilated) and can’t effectively pump blood out of the heart. Although this type can affect people of all ages, it occurs most often in middle-aged people and is more likely to affect men. The most common cause is coronary artery disease or heart attack.
Hypertrophic Cardiomyopathy: This type involves abnormal thickening of the heart muscle, particularly affecting the muscle of the heart’s main pumping chamber (left ventricle). The thickened heart muscle can make it harder for the heart to work properly.
Hypertrophic cardiomyopathy can develop at any age, but the condition tends to be more severe if it becomes apparent during childhood. Most affected people have a family history of the disease, and some genetic mutations have been linked to hypertrophic cardiomyopathy.
Restrictive cardiomyopathy: The heart muscle becomes rigid and less elastic, so it can’t expand and fill with blood between heartbeats. This least common type of cardiomyopathy can occur at any age, but it most often affects older people. Restrictive cardiomyopathy can occur for no known reason (idiopathic), or it can be caused by a disease elsewhere in the body that affects the heart, such as when iron builds up in the heart muscle (hemochromatosis).
Arrhythmogenic right ventricular dysplasia: In this rare type of cardiomyopathy, the muscle in the lower right heart chamber (right ventricle) is replaced by scar tissue, which can lead to heart rhythm problems. It’s often caused by genetic mutations.
Treatment might include medications, surgically implanted devices or other interventional/surgical procedures, in severe cases, a heart transplant may be needed.

Treating Heart Failure with Implanted Devices
Implantable cardiac defibrillators (ICD): are small, battery-powered devices that generate electrical impulses and perform pacing / give direct current shock to revive a patient from cardiac arrest due to ventricular tachycardia/fibrillation.
Cardiac Resynchronization Therapy (CRT): This treatment uses a special pacemaker by a heart transplant surgeon that syncs the left and right ventricles of heart failure patients, to make it pump more efficiently. This can be combined with an implantable cardiac defibrillator.
Mechanical-Assist Devices
- An intra-aortic balloon pump (IABP) increases cardiac output and blood flow, which is usually placed inside the main blood pipe (aorta) through a blood vessel in the groin.
- Temporary assist devices are mechanical pumps that help the heart pump blood through the body. They allow the heart to stabilize while the care team decides what other treatment options are best.
- Ventricular assist devices (VADs) are permanent mechanical pumps that help the heart pump blood through the body. This can be a left ventricular assist device (LVAD) or right ventricular assist device (RVAD)
LVADs are a therapy for end-stage heart failure and an alternative to heart transplants for some patients.
Heart Transplant



Advanced heart failure due to dilated and ischemic cardiomyopathies, complex congenital heart disease and life-threatening arrhythmias despite optimal treatment. Prior to the consideration of heart transplant in Chennai, India, a comprehensive evaluation of the patient is carried out including a thorough multiorgan and multidisciplinary workup. Some of the contraindications to a transplant include irreversible pulmonary hypertension, recent history of malignancies, active infection and multiple organ dysfunction. Suitable candidates are placed on the waitlist for transplantation. After surgery, they would be commenced on lifelong immunosuppression and managed by a multidisciplinary team with attention to rehabilitation and typical discharge from the heart transplant hospital within two to three weeks. Post-transplant, they would be reviewed at regular intervals for surveillance of graft function and patient’s well-being with emphasis on identifying episodes of acute rejection and infection. Currently, the one-year survival post heart transplantation is 85-90%. About 30-40% may develop chronic rejection in the form of cardiac allograft vasculopathy by 5 years and 60% are expected to survive beyond 10 years post-transplant. The majority of heart transplant recipients return to a normal quality of life and 30% return to active employment. To book an appointment with our experts or to learn more about heart transplant costs, contact us at +91 9150277712.
Transplant FAQ
Can heart failure be treated with a transplant?
Yes, heart failure can indeed be treated with a transplant, which becomes an option when other treatments like medications or surgeries prove ineffective. For those in need, highly skilled surgeons perform these life-saving procedures at specialized heart transplant hospitals, such as those found in Chennai, India.
What conditions might lead to consideration for a heart transplant?
Conditions that might lead to consideration for a heart transplant include advanced heart failure due to dilated and ischemic cardiomyopathies, complex congenital heart disease, and life-threatening arrhythmias despite optimal treatment. In such cases, patients may be referred to a specialized heart transplant hospital for evaluation and potential transplantation.
What is involved in the evaluation process for heart transplantation?
The evaluation process for heart transplantation is comprehensive and led by transplant specialists at a specialized heart transplant hospital. It involves a meticulous review of the patient’s medical history and current health status to determine their suitability for the procedure.
What is the survival rate post-heart transplantation?
The survival rates post-heart transplantation are encouraging, with a one-year survival post-heart transplantation rate of approximately 85-90%. Moreover, about 60% of recipients are anticipated to live beyond 10 years post-transplant.
What is the quality of life like for heart transplant recipients?
The majority of heart transplant recipients return to a normal quality of life, with around 30% able to return to active employment, highlighting the success of the procedure in restoring function and well-being.



