Journal scan: A review of 25 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
Drug-Induced Oxidative Hemolysis
(1). Wing Kit Lam et al, Published April 24, 2024, N Engl J Med 2024;390:1513,DOI: 0.1056/NEJMicm2312581, VOL. 390 NO. 16
A 57-year-old woman with a history of depression and insomnia presented to the emergency department with a 3-day history of shortness of breath and dizziness. The physical examination was notable for pallor. Laboratory studies showed a hemoglobin level of 4.4 g per deciliter (reference range, 11.6 to 15.5), an elevated reticulocyte count, an elevated lactate dehydrogenase level, and a low haptoglobin level. The results of hemoglobin electrophoresis and glucose-6-phosphate dehydrogenase testing were normal, and methemoglobin and direct antiglobulin tests were negative. A peripheral-blood smear (Panel A, Giemsa staining) showed poikilocytosis, nucleated red cells (black arrows), and polychromatic cells (white arrows).

The findings were also consistent with oxidative hemolysis, including the presence of bite cells (Panel A, red arrows), blister cells (Panel A, asterisks), and erythrocyte inclusions (Panel B, Giemsa staining). The erythrocyte inclusions were identified as Heinz bodies on the basis of positive staining with methyl violet (Panel C). Blood transfusions were administered. After a prolonged toxicologic investigation that involved multiple readmissions over the course of the next 7 months, the patient eventually reported having taken 10 times the recommended daily dose of zopiclone (a nonbenzodiazepine hypnotic) every night to treat insomnia since 1 month before the first presentation. Urine drug testing was positive for zopiclone.
A diagnosis of drug-induced oxidative hemolysis was made. The patient was counseled to cease zopiclone use and was referred to psychiatry for treatment.
Small-Bowel Bleeding
(2). Zongli Han et al, Published April 20, 2024, N Engl J Med 2024;390: e40,DOI: 10.1056/NEJMicm2312626, VOL. 390 NO. 16
A 45-year-old man who had been admitted to the hospital for a ruptured cerebral aneurysm reported a 2-hour history of abdominal pain; large-volume hematochezia subsequently developed. Five days before the onset of these symptoms, stent-assisted embolization of the ruptured cerebral aneurysm had been performed and treatment with aspirin and clopidogrel had been initiated. After the hematochezia started, intravenous fluids, transfusions, and vasopressors were administered to treat hemorrhagic shock. Findings on emergency endoscopy and colonoscopy were unremarkable.

Computed tomographic angiography (CTA) showed a dense focus of contrast material in the proximal jejunum (Panel A, black arrow [arterial phase]; inset, black arrow [portal venous phase]), extravasated contrast material in an adjacent loop of bowel (inset, white arrow [portal venous phase]), and intraluminal blood accumulation. CTA is a highly accurate imaging method for the localization of brisk gastrointestinal bleeding. Subsequently, a laparotomy was performed (Panel B). A bleeding small-bowel diverticulum was found and resected (Panel B, inset). The small intestines were dusky in color owing to the intraluminal accumulation of blood clots and ischemic edema of the intestinal wall. A final diagnosis of hemorrhagic shock from a small-bowel diverticular bleed was made. The patient was discharged home in good condition on hospital day 21 and resumed treatment with aspirin
Bizarre Wide-Complex Tachycardia in a Man in His 60s with Severe Chest Pain
(3) .https://edhub.ama-assn.org/jn-learning/module/2790775
A man in his 60s presented to the emergency department with chest pain of 18-hour duration. On admission, his pulse was 129 beats per minute, respiratory rate was 36 breaths per minute, and blood pressure was 126/77 mm Hg. An electrocardiogram (ECG) showed a regular wide-complex tachycardia, which raised concern about ventricular tachycardia (Figure, A).

We identified a 1:1 atrioventricular relationship in leads V4-5 but did not exclude ventricular tachycardia with 1:1 retrograde conduction.1 Rather than wide QRS complexes, the ECG tracing suggested a combination of QRS and extreme ST-deviation (Figure, B). The triangular or lambda-shaped QRS-ST ECG pattern appears to be an ominous sign with a malignant prognosis in patients with acute ST-elevation myocardial infarction.2,3 Emergent coronary arteriography showed a thrombotic completely occluded left anterior descending artery, which was effectively revascularized percutaneously. However, because the coronary artery thrombosis was complicated by polymorphic ventricular tachyarrhythmia and cardiogenic shock, the patient eventually required extracorporeal membrane oxygenation support. Unfortunately, the patient’s health status continued to deteriorate, and he died 1 day later.
Action demanded on alcohol as deaths hit record levels
(4). BMJ 2024; 385 doi: https://doi.org/10.1136/bmj.q963 (Published 26 April 2024) BMJ 2024;385:q963
With a record number of UK deaths from alcohol and drinking rates high among children, Bryan Christie examines the data and what is being done to reverse the trends
Campaigners are calling for action to tackle a worsening public health crisis after new data showed that the death toll from alcohol related causes has reached record levels in the UK.
At a time when 27 people in the UK are dying a day as a result of alcohol misuse, drinks companies are spending some £6bn promoting their products in major markets around the world
The latest figures from the Office for National Statistics (ONS)2 show that in 2022 there were 10 048 deaths (16.6 per 100 000 people) from alcohol specific causes registered in the UK, the highest number on record. This was 32.8% higher than in 2019, before the covid pandemic. Death rates stabilised in the period from 2012 to 2019.
Meanwhile, a report published on 25 April by the World Health Organization on substance misuse among children in 44 countries has found the highest prevalence of drinking among children in England
Big alcohol: Universities and schools urged to throw out industry-funded public health advice
(5). BMJ 2024; 385 (Published 24 April 2024)Cite this as: BMJ 2024;385:q851
The long term harms of alcohol are being minimised in industry funded education
The public health community is calling for a ban on materials by industry associated charities because they normalise drinking; because they “don’t treat alcohol as a problematic, difficult substance.”
These resources normalise drinking instead of presenting arguments for not drinking at all.
These materials teach students “responsible drinking” skills and downplay the long term health risks of alcohol, which include an increased risk of cancer and cardiovascular disease. But there is no level of regular drinking that can be considered completely safe in relation to some cancers.
“The guidelines are for low risk drinking, but drinking at any level is still associated with risk of harm. The stated aim of the guidelines is to inform people but not to stop them drinking alcohol, “as it is considered a normal activity.”
It added that the guide begins with the statement, “drinking doesn’t have to be a way of life at university” and that one in five young people choose not to drink. The guide also advises students to eat and drink plenty of water to go out to “help you not get too drunk.” “Food helps slow the absorption of alcohol, stopping it going to your head too quickly.”
“Food has no relevance to the longer term harms of alcohol, including cardiovascular disease, cancers and fetal alcohol spectrum disorders”..
“This advice is an example of assuming the drinking of alcohol, akin to teaching students how to pre-load ‘safely,’ rather than helping them question whether they should be pre-loading at all,”
“This type of initiative is interesting in that it is not about helping students to avoid getting drunk in the first place. It is after having consumed and therefore also having purchased large volumes of alcohol, trying to minimise the worst effects of those excesses.”
“5% of all men over 16 drink more than 50 units a week and 3% of women drink more than 35 units a week in England. Drinking at this level increases the risk of cancers (colon, breast, upper digestive tract), of heart disease and alcoholic liver diseases long-term. That’s why in the UK in 2019, 7565 people died from an alcohol-related illness, mainly from alcoholic liver disease.”
“Prolonged abuse of alcohol can lead to addiction and causes many life threatening conditions including heart disease, haemorrhagic stroke, cancers of the liver, breast, mouth and throat, as well as cirrhosis of the liver and addiction.
Editor’s Choice: Doctors can’t fix the alcohol problem by themselves
(6). BMJ 2024; 385 doi: https://doi.org/10.1136/bmj.q936 (Published 25 April 2024)Cite this as: BMJ 2024;385:q936.
Rebecca Coombes, head of journalism, The BMJ
A decade ago the jurisdiction of England and Wales was on the brink of introducing a policy that would have led to substantial reductions in the harms done by alcohol (doi:10.1136/bmj.f7646).1 Instead, politicians U turned, ignoring strong health advice in favour of protecting industry interests. Other, braver territories, including Ireland and Australian states, brought in minimum unit pricing, and today the policy saves lives and reduces consumption and hospital admissions (doi:10.1136/bmj-2023-077550).2 After Scotland introduced a minimum unit price, the biggest reduction in alcohol related deaths was seen among the most deprived groups.
As evidence mounts for the effect of minimum pricing on reducing alcohol consumption, those countries holding out are basing their reluctance on other factors, such as their cosy relationship with big alcohol. Over and over again we see how the industry is an active participant in policy development (doi:10.1136/bmj.q800).3 The sector still provides masterclasses in spin, most recently in a UK parliamentary inquiry, claiming credit for declines in youth drinking while downplaying historical highs in alcohol related deaths.
Public knowledge about the true extent of the harm done by alcohol lags behind the science. Where are the public health campaigns and mandatory product labelling to ensure that people know that alcohol causes cancer and that every additional drink increases the risk? And why would any country open its classroom doors or university campuses to the alcohol industry’s drama productions, “educational” shot glasses, and unit wheels? (doi:10.1136/bmj.q851).4 We have become so socialised to the “freshers’ week of oblivion” that we miss the misinformation being pumped out. These industry backed materials focus on what the individual drinker should do so they don’t get “too drunk” rather than on the need to restrict the sale and marketing of alcohol.
Public health advocates need to step up, as they did in Ireland to counter the industry’s influence on students. In her exit interview as royal college chair, paediatric leader Camilla Kingdon is a model of such medical advocacy (doi:10.1136/bmj.q877 doi:10.1136/bmj.q882).56 Children are often at greater risk of harm—witness the rising rates of whooping cough sweeping through Europe (doi:10.1136/bmj.q736) and the recent epidemic of scarlet fever (doi:10.1136/bmj-2023-077561).78 Kingdon is “ashamed” at the drift backwards in child health, chiefly the sustained rise in infant mortality in England over the past decade. One concern (among many) is vaccination rates falling below the World Health Organization’s target levels. Here doctors can play a direct role: 86% of parents say that healthcare professionals are their most trusted sources of vaccine information.
Kingdon’s deeply alarming impression of the shaming conditions facing too many children, including chronic hunger, shows that the problems are too big for doctors and other healthcare workers to be able to solve on their own. Helen Salisbury uses the analogy of not just fishing bodies out of the river but going upstream to find out who’s pushing people in (doi:10.1136/bmj.q918).9 With the honourable exception of colleagues in public health, she says, most doctors are downstream trying to “ease suffering when we can’t cure.”
Ultimately, it’s the government’s job to tackle the wider causes of ill health.
Differences across the lifespan between females and males in the top 20 causes of disease burden globally: a systematic analysis of the Global Burden of Disease Study 2021
(7). Vedavati Patwardhan et al, Open Access Published: May, 2024DOI:https://doi.org/10.1016/S2468-2667 (24)00053-7, Lancet Public Health 2024; 9: e270–74, Volume 9, Issue 5, E282-E294, May 2024
Summary
Background
Sex and gender shape health. There is a growing body of evidence focused on comprehensively and systematically examining the magnitude, persistence, and nature of differences in health between females and males. Here, we aimed to quantify differences in the leading causes of disease burden between females and males across ages and geographies.
Methods
We used the Global Burden of Disease Study 2021 to compare disability-adjusted life-year (DALY) rates for females and males for the 20 leading causes of disease burden for individuals older than 10 years at the global level and across seven world regions, between 1990 and 2021. We present absolute and relative differences in the cause-specific DALY rates between females and males.
Findings
Globally, females had a higher burden of morbidity-driven conditions with the largest differences in DALYs for low back pain (with 478·5 [95% uncertainty interval 346·3–632·8] more DALYs per 100 000 individuals among females than males), depressive disorders (348·3 [241·3–471·0]), and headache disorders (332·9 [48·3–731·9]), whereas males had higher DALY rates for mortality-driven conditions with the largest differences in DALYs for COVID-19 (with 1767·8 [1581·1–1943·5] more DALYs per 100 000 among males than females), road injuries (1012·2 [934·1–1092·9]), and ischaemic heart disease (1611·8 [1405·0–1856·3]). The differences between sexes became larger over age and remained consistent over time for all conditions except HIV/AIDS. The largest difference in HIV/AIDS was observed among those aged 25–49 years in sub-Saharan Africa with 1724·8 (918·8–2613·7) more DALYs per 100 000 among females than males.
Interpretation
The notable health differences between females and males point to an urgent need for policies to be based on sex-specific and age-specific data. It is also important to continue promoting gender-sensitive research, and ultimately, implement interventions that not only reduce the burden of disease but also achieve greater health equity.
Funding
Bill & Melinda Gates Foundation.
Antihypertensives and risk of falls in older people
(8). JAMA Intern Med
Falls are common and dangerous for older and more vulnerable people. The main modifiable risk factor for falls is prescription drugs, and the most commonly prescribed drugs in older people are antihypertensives. The problem is that they can make people fall over when they stand up as orthostatic hypotension kicks in, especially in the immediate period after treatment is started.
This cohort study of nearly 30 000 nursing home residents, 97% of whom were men with a mean age of 78 years, found that, compared with a matched control group, initiation of antihypertensives was associated with an increased risk of fractures (5.4 v 2.2 per 100 person-years) and falls, especially among residents with dementia, high baseline blood pressures, and no recent antihypertensive treatment. The key question for clinicians is whether the expected cardiovascular benefits of treating hypertension are likely to outweigh the clear hazards of starting treatment.
Steroids for prematurity
(9). JAMA
Corticosteroids are often given to pregnant women at high risk of late premature delivery to reduce neonatal respiratory problems and deaths. But corticosteroids can cause short term hypoglycaemia in the neonates, and there is concern that they could be linked to neurodevelopmental problems in the children once they get past 6 years old.
This randomised trial of 2831 children (mean age 7 years) found no significant differences in tests of thinking and problem solving (general conceptual abilities score) between the corticosteroid group (betamethasone 12 mg given intramuscularly twice in 24 hours) and placebo (17.1% v 18.5%). There was no differences in secondary outcomes such as motor function, social responsiveness, and behaviour. The study was smaller than planned because of the covid pandemic, but it will be reassuring for pregnant women who are urged to have the steroid jabs to help their baby.
Leukaemia lifeline?
(10). N Engl J Med
CAR T cells are a potential lifeline for people with aggressive blood cancers that have recurred or failed to respond to conventional treatments. The patient’s T cells are genetically manipulated to produce specialised surface receptors (chimeric antigen receptors (CARs)). Once they’re infused back into the patient, they latch onto antigens on the surface of cancer cells and kill them. The NHS has provided CAR T therapies for children with aggressive B cell acute lymphoblastic leukaemia since 2018.
Bridge therapy gives the CAR T cells after the patient’s T cells have been harvested but before haemopoietic stem cell transplant (HSCT). The problem is that the aggressive chemotherapy needed before HSCT and drugs given to prevent graft versus host disease (GVHD) weaken the patient and can kill residual CAR T cells before they’ve completed their job of mopping up rogue leukaemia cells.
A novel “all-in-one” strategy used CAR T cell therapy engineered against tumour antigen CD7 and haploidentical (half-matched donor, usually a family member) HSCT. This avoided the need for myeloablation or GVHD prophylaxis. It was tested in 10 patients with relapsed or refractory CD7-positive cancers. The strategy was safe and effective in achieving remission, though with serious but reversible side effects.
All that glisters is not gold
(11). N Engl J Med
Empagliflozin, an SGLT-2 drug originally developed for type 2 diabetes, is a bit of a wonder drug. It has also been shown to improve cardiovascular outcomes in patients with heart failure, type 2 diabetes at high cardiovascular risk, and chronic kidney disease. So can we assume it would reduce heart failure after acute myocardial infarction?
This randomised trial of patients at increased risk of heart failure after acute myocardial infarction found that, compared with placebo, empagliflozin was safe but ineffective in reducing the risk of hospital admission for heart failure (9.1% v 8.2%) or death from any cause (5.5% v 5.2%) over an 18 month period. Further trials with more women, older people, and a racially diverse population might still yield favourable results. But for now, it’s a no.
Full steam ahead for paratyphoid A vaccine
(12). Lancet
Enteric fever (typhoid and paratyphoid fever) caused by various subtypes of Salmonella enterica, may be rare in high income countries, but it certainly hasn’t gone away. In 2017, there were around 14.3 million cases worldwide with about 135 000 deaths from what should be a preventable disease. There are two effective vaccines against typhoid in widespread use, but none against paratyphoid.
This first ever phase 1 human study of a bivalent paratyphoid A-typhoid conjugate vaccine (Sii-PTCV) found that it was safe and immunogenic for both typhoid and paratyphoid antigens compared with the currently used typhoid vaccine—typhoid conjugate vaccine. There were no serious adverse effects over six months and robust immune responses to both typhoid and paratyphoid A. This implies that the new vaccine could potentially offer comprehensive protection against enteric fever of both types.
Brachial plexopathy: an unusual manifestation of Takayasu arteritis
(13). Nayan Patel Sureja et al, DOI:https://doi.org/10.1016/S2665-9913(23)00270-9, https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(23)00270-9/fulltext
A 45-year-old woman was admitted to hospital with myocardial infarction. Examination revealed absent pulses at bilateral radial and lower limb arteries, a pulsatile swelling above the medial end of the right clavicle, bruits over the neck vessels, a systolic blood pressure difference of 50 mm Hg between the upper limbs, and right upper limb wasting (figure A), with weak hand grip. On evaluation, erythrocyte sedimentation rate (ESR) was 90 mm/h and C-reactive protein (CRP) was 20 mg/L. Other routine blood tests were normal.
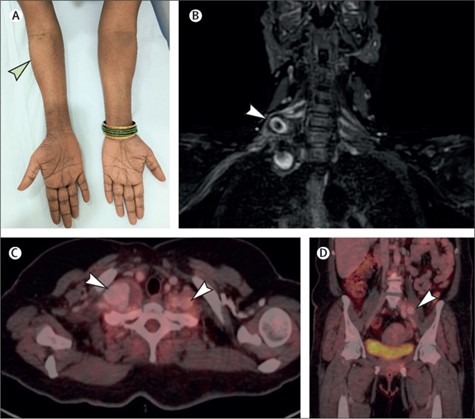
PET–CT showed circumferential vessel wall thickening with increased fluorodeoxyglucose uptake in the abdominal aorta, right renal and left iliac arteries, luminal narrowing at the origin of superior mesenteric and right iliac arteries, and saccular aneurysms of bilateral subclavian (figure B), left external iliac (figure C) and internal mammary arteries, with wall thickening and increased fluorodeoxyglucose uptake. MRI showed an aneurysm (5 × 4 × 3 cm) arising from the superior aspect of the right subclavian artery, compressing and displacing the brachial plexus (figure D). A diagnosis of Takayasu arteritis was made after ruling out other differential diagnoses (including Behcet’s disease) on history and physical examination. The patient was managed with 1 mg/kg prednisolone and 20 mg methotrexate per week, orally. Over the course of 3 months of treatment, both the ESR and CRP gradually decreased. Coronary artery bypass grafting and surgical intervention for the right subclavian artery aneurysm are planned, once disease activity is controlled. To the best of our knowledge, compressive brachial plexopathy in Takayasu arteritis has not been reported previously
Polyarteritis Nodosa
(14). Kaito Aoki et al, Published May 8, 2024, N Engl J Med 2024;390:1711,DOI: 10.1056/NEJMicm2309365, VOL. 390 NO. 18
A 62-year-old man presented to the hospital with a 1-month history of muscle aches and weakness in the anterior thighs and the lower posterior aspect of both legs and weight loss of 10 kg. On physical examination, there was numbness of the anterior thighs and posterior lower legs but no skin changes or abdominal tenderness. Laboratory tests showed elevated levels of inflammatory markers. Findings on computed tomography of the chest, abdomen, and pelvis were unremarkable. Tests for antineutrophil cytoplasmic antibodies and hepatitis B were negative. Owing to concern about polyarteritis nodosa, abdominal angiography was performed and revealed aneurysms and irregularity of the vessel walls in the axes of the celiac artery (Panel A), inferior mesenteric artery, and renal arteries (Panel B, right kidney). Treatment with oral glucocorticoids and cyclophosphamide was initiated.
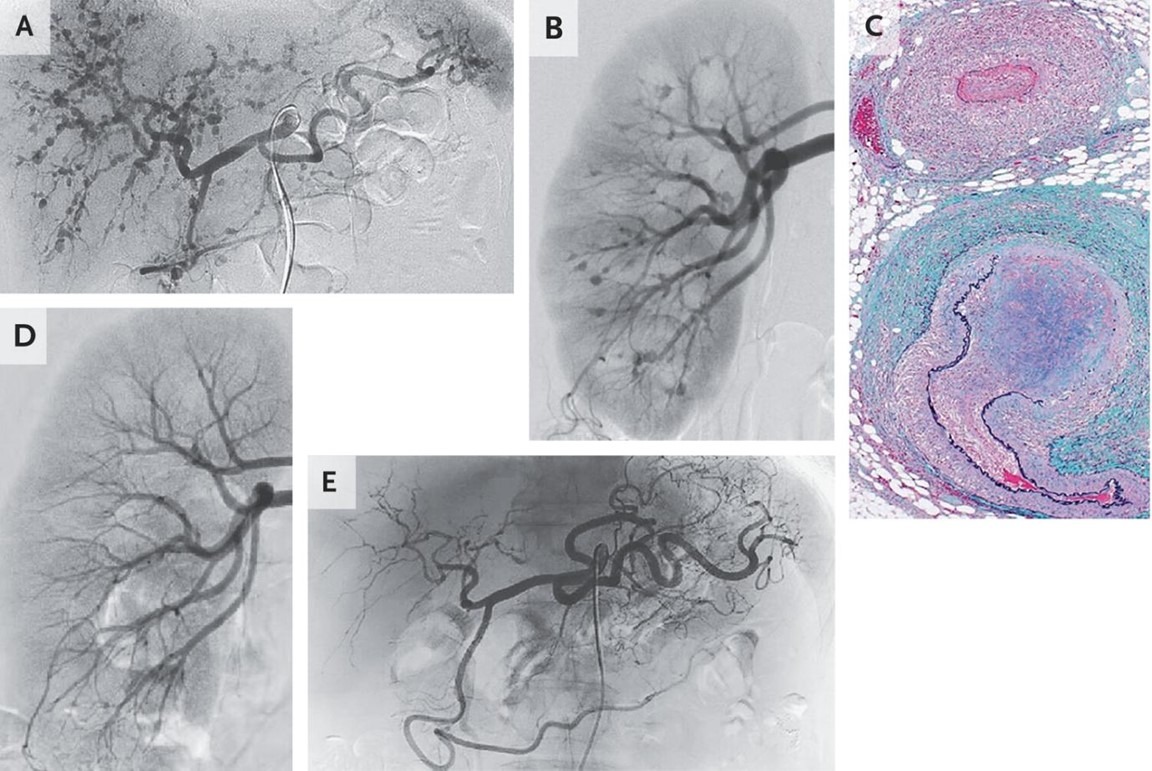
Ten days later, a bowel perforation developed. Histopathological examination of a resected segment of the transverse colon showed neutrophilic infiltration and fibrinoid necrosis of the walls of medium-size arteries, as well as disruption of the internal elastic lamina (Panel C, elastin stain). A final diagnosis of polyarteritis nodosa was made. During a prolonged postoperative hospital course, an intraabdominal abscess was treated and immunosuppression therapy was adjusted. At follow-up 5 months after presentation, angiography showed resolution of the vascular changes (Panel D [renal artery, right kidney] and Panel E [celiac artery axis])
(15). Matiar Madanchi, M.D, and Peter Itin, M.D., Ph.D. Published May 4, 2024, N Engl J Med 2024;390: e43,DOI: 10.1056/NEJMicm2313316,VOL. 390 NO. 18
A healthy 72-year-old man who had emigrated from Zimbabwe 20 years previously presented to the dermatology clinic with a 17-year history of swelling of the penis, scrotum, and left leg.

During a recent hospitalization, nonpitting edema of the left leg had been noted, and a urinary catheter had been placed temporarily (Panel A). At the current presentation, there was nonpitting edema of the penis and scrotum (Panel B), as well as ongoing swelling of the left leg. Laboratory testing showed an eosinophil count of 500 per cubic millimeter (normal range, 0 to 300). Magnetic resonance imaging of the pelvis showed swelling of the scrotal tissues on both sides; no hydrocele was present. An enzyme-linked immunosorbent assay and an indirect fluorescent antibody test for Wuchereria bancrofti were positive. A blood smear to identify microfilariae was not obtained. A diagnosis of chronic lymphatic filariasis — a mosquito-borne parasitic infection in which nematodes invade the lymphatic system — was made. The patient was treated initially with a course of doxycycline and single-dose albendazole. Single-dose diethylcarbamazine was given later, after tests for concomitant onchocerciasis and loiasis returned negative. Diethylcarbamazine administration is contraindicated in patients with lymphatic filariasis and concomitant onchocerciasis or loiasis owing to the risk of severe adverse reactions from the rapid killing of microfilariae. At follow-up 2 months after the completion of treatment, the patient’s symptoms had resolved.
JAMA Clinical Challenge: A 3-Year-Old With Gingival Hemorrhage and Musculoskeletal Pain
(16). Khanh Trinh et al, JAMA. Published online May 8, 2024. doi:10.1001/jama.2024.3580
Case
A3-year-old previously healthy boy presented to the dental office for gum bleeding that developed 2 weeks prior to presentation. His parents reported dark spots on his gums that appeared spontaneously over several days and bleeding during teeth brushing. He had no preceding oral trauma and no recent infections.

One week after onset of these oral symptoms, he developed a limp in the right leg. His parents also noticed he had difficulty standing up after sitting down to play. He was evaluated by a pediatrician, who diagnosed transient synovitis of the hip due to a viral infection. Findings on a radiograph of the right hip were normal. During the week prior to presentation, the patient developed spontaneous gingival bleeding and increased bilateral limb weakness with inability to bear weight. On presentation to the dental office, he appeared irritable. Physical examination revealed generalized gingival swelling and spontaneous gingival bleeding. He had no lesions on his lips and no edema or exudate in the oropharynx (Figure). The patient’s parents reported that he took no regular medications, had no recent use of aspirin or nonsteroidal anti-inflammatory medications, and that his diet was limited to primarily chicken nuggets and milk.
What Would You Do Next?
- Prescribe acyclovir (20 mg/kg) 4 times daily for 7 days
- Prescribe amoxicillin (125 mg/5 mL oral suspension) for 7 days
- Perform a gingival biopsy
- Check plasma level of vitamin C
Diagnosis
Scurvy (vitamin C deficiency)
What to Do Next
Do Check plasma level of vitamin C
The key to the correct diagnosis is recognizing that spontaneous gingival hemorrhage and limb weakness are characteristic manifestations of scurvy. Herpes infection (choice A) is incorrect because this typically presents with vesicular lesions on the lips and is not associated with diffusely hemorrhagic gingiva. Amoxicillin (choice B) is not indicated because the patient’s symptoms are not suggestive of a bacterial infection. Biopsy of the gingiva (choice C) is an invasive procedure that should be considered only if plasma vitamin C level is within reference range.
Discussion
Vitamin C, also known as L-ascorbic acid, is a water-soluble nutrient that is important for fatty acid transport, neurotransmitter synthesis, prostaglandin metabolism, nitric oxide synthesis, and collagen synthesis.1,2 Humans are unable to synthesize vitamin C, and it must be obtained through dietary intake.3 Food sources of vitamin C include citrus fruits and vegetables (eg, broccoli, tomatoes, cauliflower, brussels sprouts).4 Breast milk provides vitamin C to infants.2 Vitamin C has a half-life of 10 to 20 days, and because humans are unable to store
vitamin C, deficiency of vitamin C can develop within 1 to 3 months of inadequate vitamin C intake.2
Chronic vitamin C deficiency, also known as scurvy, is one of the oldest known nutritional disorders.4 Although its exact incidence is unknown, scurvy is reported sporadically in the US in both children and adults; the 2017-2018 National Health and Nutrition Examination Survey estimated that 5.9% of the US population had vitamin C deficiency.2 In high-income countries, scurvy may result from limited access to or inability to buy fruits and vegetables, or it may be associated with alcohol use disorder, eating disorders, and inflammatory bowel disease. Among children, risk factors include avoidant/restrictive food intake disorder, autism, and neglect.2,5 Infants who are exclusively fed cow’s milk are also at increased risk of scurvy.2
Initial signs of scurvy include loss of appetite, low-grade fever, and agitation,6 typically followed by generalized gingival swelling and spontaneous bleeding.4 Dermatologic features include petechiae, ecchymosis, perifollicular hemorrhage, and corkscrew hair.2 Scurvy may cause periodontal disease, loosening of teeth within their sockets, and loss of teeth.4 Musculoskeletal symptoms such as arthralgia of the knee, wrist, or ankle; myalgia; and asthenia develop in approximately 80% of patients with scurvy.7 The most common radiographic feature of scurvy is Frankel sign, consisting of increased calcification around the metaphysis.7
Symptoms of scurvy typically occur when plasma vitamin C levels are less than 0.2 mg/dL (reference, 0.6-2.0 mg/dL), although recent vitamin C intake can result in normal plasma levels even if tissue levels are low.8 Prompt resolution of symptoms after treatment with vitamin C is the best indicator of the diagnosis of scurvy.4 Laboratory evaluation reveals anemia in 75% of patients with scurvy,5 and values for inflammatory markers such as erythrocyte sedimentation rate may be elevated.9 The differential diagnosis includes osteomyelitis, septic arthritis, acute lymphoblastic leukemia, systemic lupus erythematosus, Henoch-Schönlein purpura, disseminated intravascular coagulation, immune thrombocytopenic purpura, leukocytoclastic vasculitis, and child neglect or abuse.4,7,9 Diagnosis is commonly delayed; in 9 studies of 42 children with scurvy, the median time from onset of clinical symptoms to diagnosis of scurvy was 2 months.10 A high index of suspicion is necessary to promptly diagnose scurvy. If untreated, scurvy can cause dyspnea, hypotension, gastrointestinal hemorrhage, and sudden death.2
Although there are no established treatment guidelines, initial therapy typically involves oral, intramuscular, or intravenous administration of high-dose vitamin C (300-1000 mg daily) for several days to 1 week, followed by 100 to 300 mg daily for 1 month.2,3,5 Three-times-daily dosing of vitamin C is recommended to maximize intestinal absorption.10 After initial treatment, a diet that contains sufficient fresh fruits and vegetables can prevent recurrence of scurvy.
Patient Outcome
The patient’s vitamin C level was undetectable. He started oral vitamin C, 600 mg/d. Within 48 hours, his parents reported resolution of gingival bleeding and improved muscle strength. Two weeks after starting vitamin C, the patient’s gingiva, muscle strength, and gait were normal. He is taking a multivitamin supplement daily, and his parents have incorporated more fruits and vegetables into his diet.
Chronic Silicosis
(17). Shan Kai Ing, et al , Published May 11, 2024, DOI: 10.1056/NEJMicm2312247
A 47-year-old man who had been admitted to the hospital with gastroenteritis was found to have abnormalities on a chest radiograph. He had a 25-pack-year smoking history and had worked in a quarry for more than 30 years. He had no respiratory symptoms, and the vital signs and physical examination were normal. The chest radiograph showed diffuse nodular opacities (Panel A). Computed tomography of the chest revealed lung nodules in a perilymphatic distribution (Panel B), as well as matted mediastinal lymphadenopathy with calcifications.
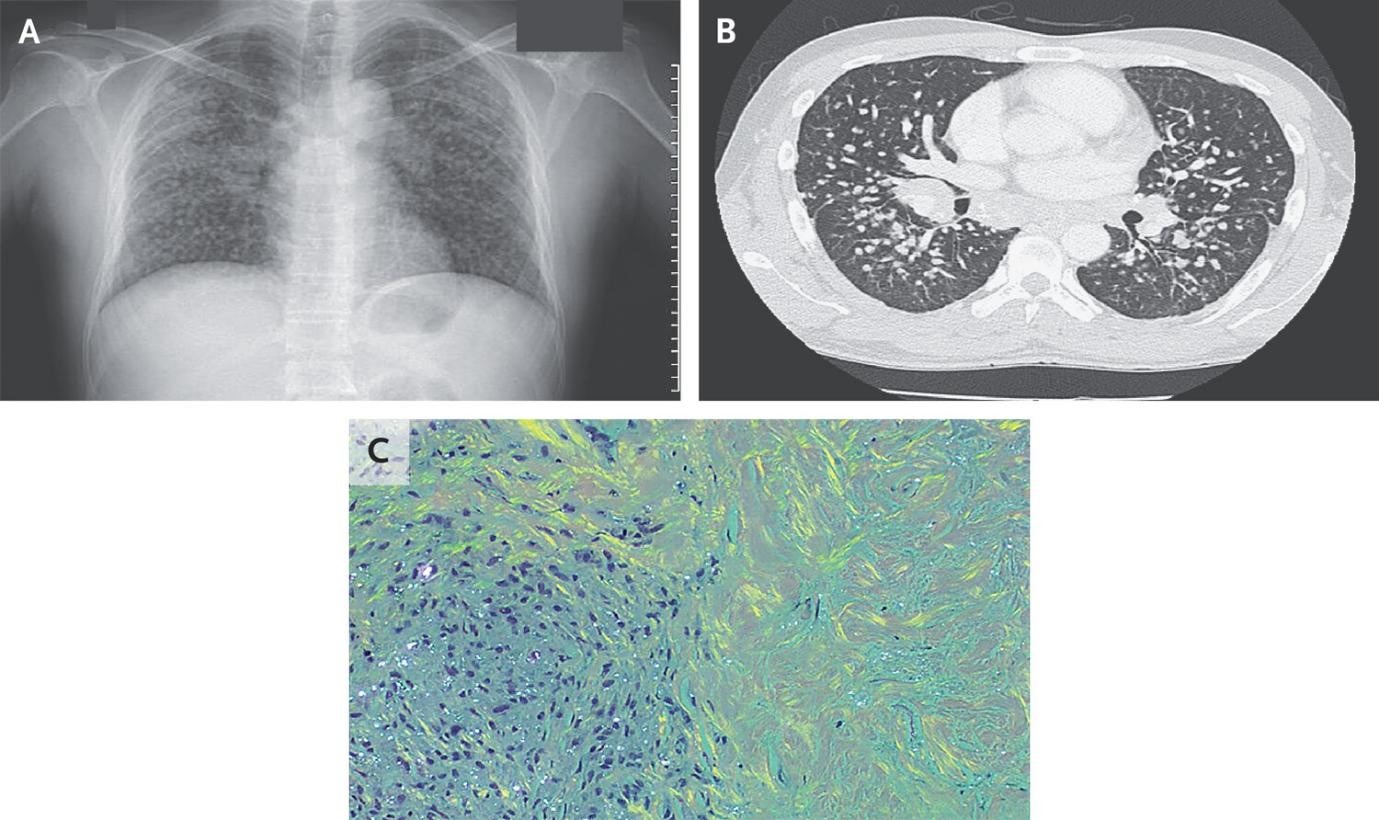
Spirometry showed a restrictive ventilatory pattern without evidence of obstruction. A bronchoscopy with bronchoalveolar lavage and a transbronchial lung cryobiopsy were performed. Tests for infectious diseases, including tuberculosis, were negative. Histopathological analysis of a biopsy specimen under polarized light revealed abundant silica crystals (Panel C). A diagnosis of chronic silicosis — an occupational pneumoconiosis caused by the inhalation of crystalline silicon dioxide — was made. The condition afflicts workers in occupations such as coal mining, sandblasting, and quarrying, as in this case. Smoking-cessation counseling was provided, and nicotine replacement therapy was initiated. A report was filed with an occupational safety office. The patient was provided with a respirator and resumed working in the quarry owing to his difficulty with finding other work. At a 6-month follow-up visit, he remained asymptomatic.
Pacemaker-Lead Dislodgement and Cardiac Perforation
(18). Christina Menexi et al, Published May 15, 2024, N Engl J Med 2024;390:1802,DOI: 10.1056/NEJMicm2312569, VOL. 390 NO. 19
A 96-year-old woman presented to the emergency department with a 1-day history of pleuritic chest pain 4 days after a single-chamber transvenous pacemaker had been implanted for complete heart block. Her blood pressure was 100/60 mm Hg, and her heart rate was 40 beats per minute. An electrocardiogram showed complete heart block with an atrial rate of 84 beats per minute, a junctional escape with a right bundle-branch block and a rate of 42 beats per minute, and pacing spikes without ventricular capture (Panel A, arrows).
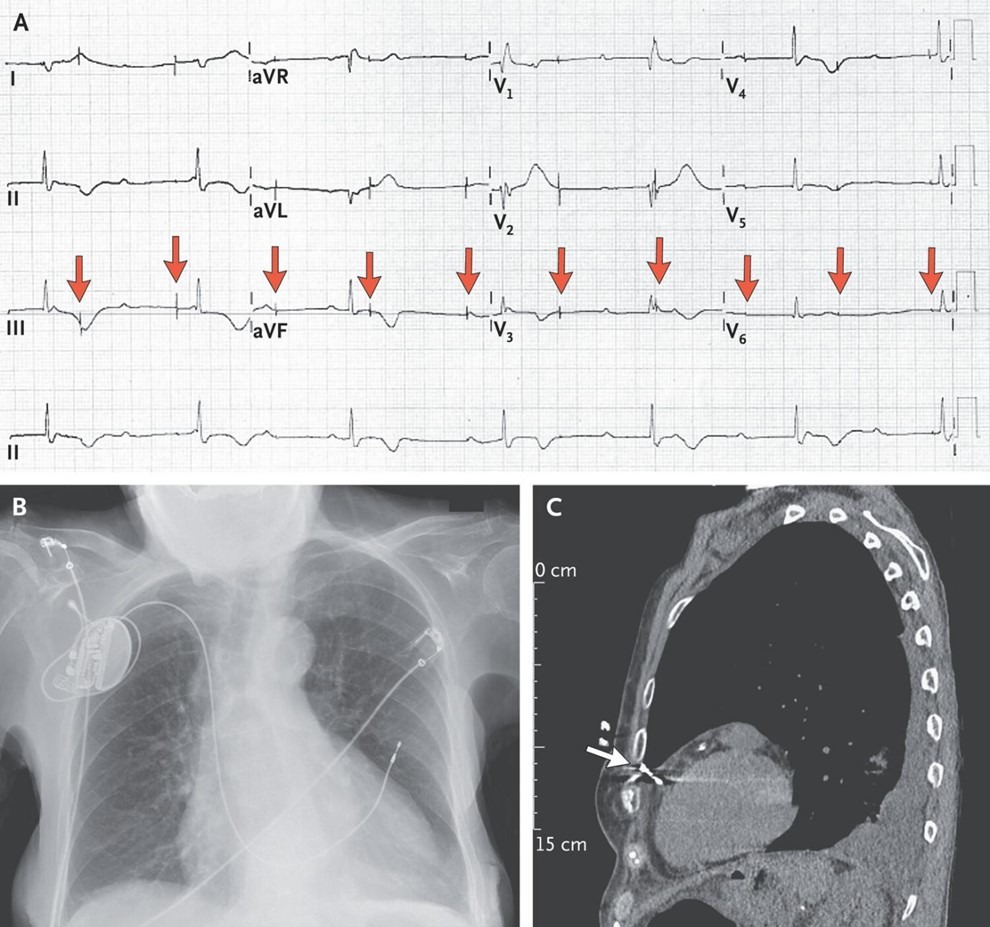
A chest radiograph showed the tip of the right ventricular lead positioned over the left mid-hemithorax (Panel B, anteroposterior view). A computed tomographic scan of the chest showed the pacing lead tip traversing the right ventricle, ending in the left pleural space (Panel C, arrow; sagittal view), and a moderate pleural effusion on the left side. There was no pneumothorax or pericardial effusion. A diagnosis of pacemaker-lead dislodgement with cardiac perforation was made. A patient with pacemaker-lead dislodgement may present with chest pain, dyspnea, syncope, or symptoms of cardiac tamponade or pneumothorax. A percutaneous lead revision was performed urgently with a cardiothoracic surgical team available as backup. There were no complications. The patient was discharged home 3 days after presentation.
Esophageal Varices, White-Nipple Sign, and Portal Hypertensive Gastropathy
(19). Michael Najem et al, Published May 15, 2024, N Engl J Med 2024;390: e47, DOI: 10.1056/NEJM icm2307201,VOL. 390 NO. 19
A 66-year-old man with recently diagnosed cirrhosis secondary to metabolic dysfunction–associated steatohepatitis presented to the emergency department with a 1-day history of melena and hematemesis. The patient had not had an endoscopy to screen for esophageal varices. The physical examination was notable for scleral icterus; moderate, nontender abdominal distention without a fluid wave; and melena on digital rectal examination. He had Child–Pugh class C liver function with a score of 11, indicating severe, decompensated liver disease. An upper endoscopy showed three columns of esophageal varices without active bleeding (Panel A). However, one varix had a “white-nipple sign” (Panel A, arrow), which indicates recent variceal hemorrhage and results from the formation of a fibrin plug at the site of a resolved thrombus. Severe portal hypertensive gastropathy was also seen (Panel B). A diagnosis of variceal hemorrhage was made. Endoscopic variceal ligation therapy was performed. Courses of octreotide, pantoprazole, and antimicrobial therapy were completed, and carvedilol was initiated. The patient was deemed not to be a candidate for a transjugular intrahepatic portosystemic shunt. One month after hospital discharge, the patient was readmitted with upper gastrointestinal bleeding that resulted in hemorrhagic shock and multiple organ failure. The patient was ineligible for liver transplantation, and he opted to transition to comfort care.
Assessing safety and efficacy of a novel glucose-free amino acid oral rehydration solution for watery diarrhea management in children: a randomized, controlled, phase III trial
(20). Pradip Kumar Bardhan et al, Published:May 17, 2024DOI:https://doi.org/10.1016/j.eclinm.2024.102630. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00209-8/fulltext
Summary
Background
Diarrhoeal disease poses a significant global health challenge, especially in children under three years old. Despite the effectiveness of oral rehydration therapy (ORT), its adoption remains low. Glucose-based ORS (GORS) is the standard, but novel formulations like glucose-free amino acid-based VS002A have emerged as potential alternatives. This study aimed to compare the safety and efficacy of VS002A against the standard WHO-ORS in treating non-cholera acute watery diarrhoea in children.
Methods
A triple-blind, randomized trial enrolled 310 male infants and children aged 6–36 months, who were assigned to receive WHO-ORS or VS002A over a 16-month period, from June 2021 to September 2022. Both groups received standard of care, including zinc supplementation. The Primary study outcome measured was the duration of diarrhoea. Secondary outcomes included stool output, treatment failure and adverse events. Exploratory endpoints included urinary output, body weight changes, blood biochemistry, stool microbiology and gut health biomarkers.
Findings
Both VS002A and WHO-ORS were well-tolerated with a low adverse event rate. While not different statistically (p = 0.10), duration of diarrhoea was shorter in children treated with VS002A vs. WHO-ORS (65.4 h vs. 72.6 h). Similarly, stool output was also lower vs. WHO-ORS in children treated with VS002A, though not statistically different (p = 0.40). Serum citrulline levels, an indicator of gut health, were higher in the VS002A group at 24 h suggesting a potential protective effect (p = 0.06).
Interpretation
The findings of this study support the non-inferiority of VS002A, a glucose-free amino acid-based ORS compared to the WHO-ORS standard of care. VS002A was shown to be safe and effective in treating non-cholera acute watery diarrhoea in young children. VS002A may offer advantages in pathogen-driven diarrhoea, supported by trends toward a lower duration of diarrhoea and stool output within the per protocol group. Furthermore, individuals with prolonged diarrhoea, severe malnutrition, environmental enteric dysfunction or have issues with obesity or insulin resistance, could benefit from a glucose-free ORS. This research contributes to addressing the persistent challenge of childhood diarrhoea by presenting an alternative glucose-free ORS formulation with potential advantages in select scenarios, offering a promising avenue for improving paediatric diarrhoea management worldwide.
Funding
The study was funded by Entrinsic Bioscience, LLC., Norwood, MA, USA.
AMA Clinical Guidelines Synopsis, April 24, 2024: Lower Gastrointestinal Hemorrhage
(21). Hira Imran etal, JAMA. 2024;331(19):1666-1667. doi:10.1001/jama.2023.25841
Guideline title: Management of Patients With Acute Lower Gastrointestinal Bleeding, Release date February 2023, Developer American College of Gastroenterology (ACG)
Target population Patients with gastrointestinal (GI) bleeding originating from a suspected colorectal source
Selected recommendations
Risk stratification tools (eg, Oakland score) are suggested to aid clinical judgment in identifying low-risk patients with GI bleeding who are appropriate for early discharge and outpatient diagnostic evaluation (conditional recommendation; low-quality evidence).
For patients with hemodynamic instability and hematochezia presenting within 4 hours of onset, computed tomography angiography (CTA) is the suggested initial diagnostic test (conditional recommendation; low-quality evidence).
For patients with a positive CTA, prompt referral to interventional radiology for transcatheter arteriography and possible embolization is recommended. Colonoscopy can also be considered in specialized, experienced centers (strong recommendation; moderate-quality evidence).
Anticoagulant reversal is suggested for life-threatening bleeding in patients with significantly prolonged international normalized ratio (INR) or direct oral anticoagulant (DOAC) use within the previous 24 hours who do not respond to initial resuscitation (conditional recommendation; very low-quality evidence).
After resolution of lower GI bleeding (LGIB), patients who require anticoagulation to reduce the risk of thromboembolism should resume anticoagulation, typically within 7 days (strong recommendation; moderate-quality evidence).
Patients with a high-quality colonoscopy showing diverticulosis with no colorectal neoplasia within the last 12 months may not need repeat inpatient colonoscopy if bleeding has subsided and no new symptoms are present (conditional recommendation; low-quality evidence).
Red-Cell Rosette Formation in Malaria
(22). Irene Frances et al, Published May 25, 2024, DOI: 10.1056/NEJMicm2313699,
A 57-year-old woman with a history of recently treated malaria presented to the hospital with a 2-week history of fatigue and anorexia and a 2-day history of fever.
Three months before presentation, she had completed a course of piperaquine and dihydroartemisinin to treat a Plasmodium vivax infection and had returned to normal health. Her temperature was 39°C, and blood pressure 98/50 mm Hg.
A physical examination was notable for splenomegaly. Laboratory testing showed a hemoglobin level of 10.6 g per deciliter (reference range, 12.0 to 15.5). A peripheral-blood smear that was prepared with May–Grünwald–Giemsa stain showed red cells containing malaria gametocytes (black arrow) and mature trophozoites (white arrows) surrounded by uninfected erythrocytes in rosette formations.
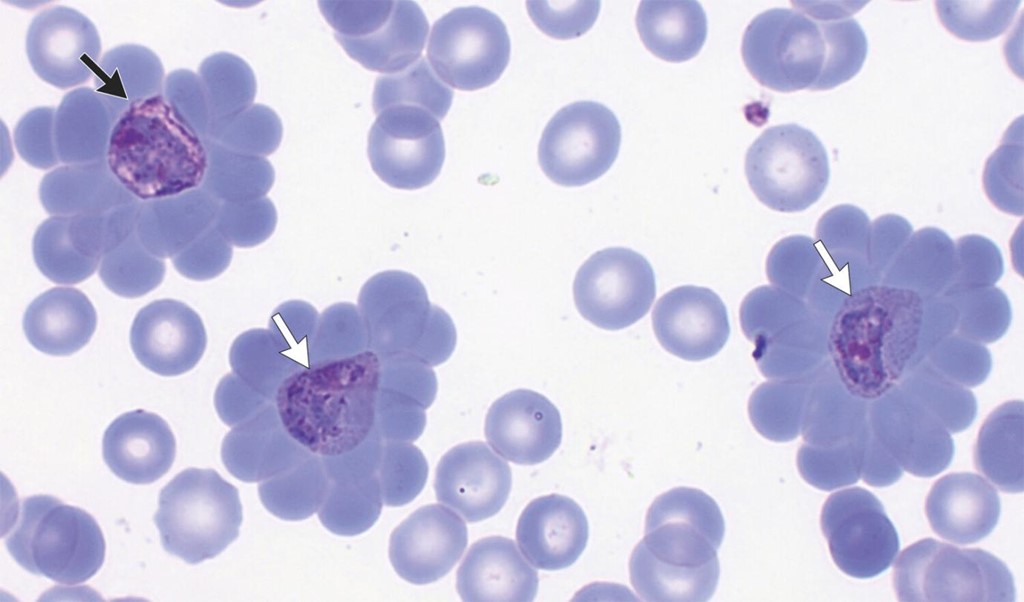
Red-cell rosette formation, which may be seen in P. vivax or P. falciparum infection, is thought to be a mechanism by which infected cells can escape splenic sequestration, phagocytosis, and possibly, exposure to antimalarial agents. Antigen testing for P. vivax was positive, and the parasite load was less than 1% in red cells. A diagnosis of malaria due to relapsed P. vivax infection was made. Treatment with another course of antimalarial agents was given. At 3 weeks of follow-up, the patient was reevaluated and found to be afebrile and asymptomatic.
JAMA Oncology Clinical Challenge: A Patient With Slow Communication and Difficulty Walking
(23). Hirokazu Matsushima, et al, JAMA Oncol. Published online May 23, 2024. doi:10.1001/jamaoncol.2024.0978
Case
A70-year-old woman with hypertension and dyslipidemia presented with slow communication and difficulty walking 90 days after 6 courses of postoperative chemotherapy (docetaxel plus cyclophosphamide) following right breast cancer surgery (pT2N2aM0, stage IIIA). She had been hospitalized for anorexia 1 week before, had good oral intake after admission, and was discharged the day prior. After the third course of postoperative chemotherapy, she experienced severe nausea, leading to poor food intake and 28% loss of body weight over the following 6 months. She did not consume alcohol or illegal drugs. At presentation, she was fever free with a blood pressure of 102/64 mm Hg, was expressionless and disoriented, and had delayed responses, which made the accurate assessment of memory impairment difficult. Aphasia was not observed. She was able to follow her gaze but had nystagmus during the left gaze. She could not move her upper and lower extremities smoothly and had an ataxic gait. Results of a manual muscle test were normal. No stiff neck or involuntary movements were observed. Physical examination revealed no signs of meningeal irritation. Blood test results showed a white blood cell count of 14 580/μL (to convert to ×109/L, multiply by 0.001), C-reactive protein of 7.81 mg/dL (to convert to mg/L, multiply by 10), sodium of 129 mEq/L (to convert to mmol/L, multiply by 1), potassium of 3.4 mEq/L (to convert to mmol/L, multiply by 1), calcium of 8.9 mg/dL (to convert to mmol/L, multiply by 0.25), inorganic phosphorus of 4.0 mg/dL (to convert to mmol/L, multiply by 0.323), and magnesium of 1.4 mg/dL (to convert to mmol/L, multiply by 0.4114). Creatinine level and liver, thyroid, and adrenal function were normal. Urinalysis suggested a urinary tract infection. Magnetic resonance imaging (MRI) was performed (Figure).

Diffusion-weighted imaging (DWI) demonstrated diffusion restriction in the medial thalamus (A), and fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) showed high bilateral signal areas in the medial thalamus (B).
What Is Your Diagnosis?
- Encephalitis
- Meningitis
- Nonalcoholic Wernicke encephalopathy
- Paraneoplastic syndrome
Diagnosis
Nonalcoholic Wernicke encephalopathy
Discussion
The key to the diagnosis was the patient’s background of anorexia during adjuvant chemotherapy for early-stage breast cancer and recognition that the physical findings of impaired consciousness (delayed response), nystagmus, and ataxic gait were characteristic of nonalcoholic Wernicke encephalopathy. Furthermore, MRI findings were suggestive of Wernicke encephalopathy. Therefore, vitamin B1 measurements were recommended. Although an elevated inflammatory response was observed, there was no fever or neck stiffness; therefore, meningitis was unlikely. Lumbar puncture is essential when the 3 signs of meningitis are fever, impaired consciousness, and stiff neck, or when physical examination reveals signs of meningeal irritation. It is also useful in cases of suspected encephalitis associated with abnormal behavior or sudden cognitive decline. Furthermore, because the patient had undergone breast cancer surgery and there was no evidence of distant metastasis, meningeal carcinomatosis and paraneoplastic syndrome were unlikely.
Wernicke encephalopathy, an acute neurological disorder, results from vitamin B1 (thiamine) deficiency. Early diagnosis is required because prolonged exposure can lead to Korsakoff syndrome, a medical emergency. Thiamine functions as a cofactor in organic pathways and plays an essential role in brain energy metabolism.1 Thiamine deficiency causes oxidative stress, leading to neuronal death. It can damage the periaqueductal gray matter of the midbrain, medial thalamus, and mammillary bodies of the central nervous system.1
Malignant tumors are a risk factor for Wernicke encephalopathy. Thiamine deficiency in patients with malignant tumors is attributed to increased thiamine consumption by rapidly growing cancers, decreased food intake associated with nausea, substantial malabsorption, and use of fluoropyrimidine chemotherapeutic agents (which induce increased thiamine metabolism).2,3 Most cancers associated with Wernicke encephalopathy cases are gastrointestinal or hematologic cancers.4 There are few reports of Wernicke encephalopathy occurring during postoperative chemotherapy after breast cancer surgery.
Wernicke encephalopathy is often associated with altered mental status, ocular dysfunction such as nystagmus, and unstable gait, which are present in only 16% of patients.1 MRI is used to diagnose Wernicke encephalopathy with high specificity (93%) but low sensitivity (53%).5 Wernicke encephalopathy can also cause Korsakoff syndrome with severe outcomes.6,7 Patients without alcohol use disorder have a better prognosis than patients with alcohol use disorder, with fewer cases of residual memory dysfunction,2 but symptom onset is more acute in patients without alcohol use disorder than those with it.8 Therefore, Wernicke encephalopathy should be suspected based on a comprehensive history, physical examination, and MRI findings, and affected patients should be given thiamine as a supplement.
Glucose intake increases thiamine demand, which may lead to thiamine deficiency. Herein, the patient was hospitalized for anorexia and was able to eat, which may have led to progressive thiamine deficiency, resulting in symptoms of Wernicke encephalopathy after discharge. Therefore, if Wernicke encephalopathy is suspected, it is imperative to supplement with thiamine before administering glucose.1
Results of the patient’s blood tests revealed levels of vitamin B1 at 9 μg/dL (to convert to nmol/L, multiply by 29.6), vitamin B2 at 64 μg/dL (to convert to nmol/L, multiply by 26.6), vitamin B12 at greater than 1500 pg/mL (to convert to pmol/L, multiply by 0.7378), folic acid at 4.2 ng/mL (to convert to nmol/L, multiply by 2.266), copper at 81 μg/dL (to convert to μmol/L, multiply by 0.157), and zinc at 50 μg/dL (to convert to μmol/L, multiply by 0.153). A lumbar puncture was also performed. The spinal fluid was clear and colorless, and there was no increase in the number of cells or protein concentration in the spinal fluid or any decrease in sugar concentration. Thiamine, 500 mg, was administered intravenously 3 times daily for 4 days. Immediately after, the patient recovered completely and was able to communicate and walk normally. After discharge, nutritional management by a dietitian was provided on an outpatient basis to prevent recurrence of Wernicke encephalopathy.
Systemic lupus erythematosus, seminar
(24). Alberta Hoi et al , DOI:https://doi.org/10.1016/S0140-6736(24)00398-2, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00398-2/abstract
Summary
Systemic lupus erythematosus (SLE) is a multisystemic autoimmune disease characterised by the presence of autoantibodies towards nuclear antigens, immune complex deposition, and chronic inflammation at classic target organs such as skin, joints, and kidneys. Despite substantial advances in the diagnosis and management of SLE, the burden of disease remains high. It is important to appreciate the typical presentations and the diagnostic process to facilitate early referral and diagnosis for patients. In most patients, constitutional, mucocutaneous, and musculoskeletal symptoms represent the earliest complaints; these symptoms can include fatigue, lupus-specific rash, mouth ulcers, alopecia, joint pain, and myalgia. In this Seminar we will discuss a diagnostic approach to symptoms in light of the latest classification criteria, which include a systematic evaluation of clinical manifestations (weighted within each domain) and autoantibody profiles (such as anti-double-stranded DNA, anti-Sm, hypocomplementaemia, or antiphospholipid antibodies). Non-pharmacotherapy management is tailored to the individual, with specific lifestyle interventions and patient education to improve quality of life and medication (such as hydroxychloroquine or immunosuppressant) adherence. In the last decade, there have been a few major breakthroughs in approved treatments for SLE and lupus nephritis, such as belimumab, anifrolumab, and voclosporin. However the disease course remains variable and mortality unacceptably high. Access to these expensive medications has also been restricted across different regions of the world. Nonetheless, understanding of treatment goals and strategies has improved. We recognise that the main goal of treatment is the achievement of remission or low disease activity. Comorbidities due to both disease activity and treatment adverse effects, especially infections, osteoporosis, and cardiovascular disease, necessitate vigilant prevention and management strategies. Tailoring treatment options to achieve remission, while balancing treatment-related comorbidities, are priority areas of SLE management.
Music for health: Philip Ball
(25). Published:May 25, 2024DOI:https://doi.org/10.1016/S0140-6736(24)01037-7, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)01037-7/abstract
Many people (including me) will have experienced a family member or loved one who, rendered essentially non-verbal by dementia, will nonetheless sing along to the lyrics of a well-known song, often with evident delight at this reawakened ability to commune with others. Distressed babies can be soothed by gentle song when words do not work. People who stammer might find fluency in singing their speech. Some people with Parkinson’s disease can discover an otherwise unattainable ease of movement when they dance. Music and Mind: Harnessing the Arts for Health and Wellness, edited by acclaimed American singer Renée Fleming, reports all of these benefits, and many others, that music can bring, whether through listening or active participation. The book’s contributors come from a broad range of disciplines and include neuroscientists of music such as Aniruddh Patel, Daniel Levitin, and Robert Zatorre, novelists Ann Patchett (author of the 2001 novel Bel Canto) and Richard Powers, virtuoso cellist Yo-Yo Ma, and leading figures in the arts such as Deborah Rutter, President of the John F Kennedy Center for the Performing Arts in Washington, DC, USA

