Kauvery Heart & Lung Transplant Centre
by admin-blog-kh | January 28, 2022 2:27 pm
Table of Content
- Kauvery’s Heart Transplant Team[1]
- What is Advanced Heart Failure?[2]
- What is Mechanical Circulatory Support?[3]
- Heart Transplantation[4]
- Ventricular Assist Devices ( LVAD / RVAD / BiVAD /TAH)[5]
- Lung Transplantation [6]
- Success and survival rate after a Lung Transplant?[7]
- Interstitial Lung Disease [8]
- Chronic Obstructive Pulmonary Disease (COPD) [9]
- Pulmonary Hypertension (PH) [10]
- Bronchiectasis?[11]
Single destination. Trusted expertise.
Kauvery’s Heart Transplant Team
At Kauvery Hospital, we have a specialized and internationally trained team of Transplant Surgeons[12], Lung failure / Transplant Pulmonologist, Heart failure / Transplant Cardiologists[13], Thoracic transplant Anaesthetists, Intensivists, Perfusionists, Rehabilitation Physician, Psychologist, Pharmacist, Infectious Disease Specialist, Dietician and Transplant Co-ordinator with comprehensive backup team of other specialities. We have state of the art facilities dedicated to thoracic transplantation which includes Transplant theatre, four bedded ICU and six bedded heart and lung failure unit.
What is Advanced Heart Failure?
Heart failure[14] is considered to be advanced when patients are symptomatic. It is characterized by frequent episodes of decompensation and confers a poor survival. Patient needs to be referred to the dedicated heart failure / Transplant team for comprehensive evaluation and discussion about further medical and surgical options. These include the implantation of MCS (Mechanical Circulatory Support) or wait listing for heart transplant. A timely referral guarantees the best outcomes.

What is Mechanical Circulatory Support?
 These are devices used to support the failing heart of individuals already on maximal medical therapy.
These are devices used to support the failing heart of individuals already on maximal medical therapy.
They range from a temporary Intra-Aortic Balloon Pump (IABP) and Extra Corporeal Membrane Oxygenation (ECMO[15]) or the implantation of a more durable Ventricular Assist devices (VAD).
These therapies allow the options for bridging to recovery, decision making or bridging to heart transplantation.
In individuals who are not candidates for heart transplantation[17], VADs may be used for life long destination therapy when appropriate.
Heart Transplantation
The most common indications for heart transplantation are:
 Advanced heart failure due to dilated and ischemic cardiomyopathies, complex congenital heart disease and life-threatening arrhythmias despite optimal treatment. Prior to consideration of transplantation, a comprehensive evaluation of the patient is carried out including a thorough multiorgan and multidisciplinary workup. Some of the contraindications to a transplant include irreversible pulmonary hypertension, recent history of malignancies, active infection and multiple organ dysfunction. Suitable candidates are placed on the waitlist for transplantation. After surgery, they would be commenced on lifelong immunosuppression and managed by a multidisciplinary team with attention to rehabilitation and typical discharge from the hospital within two to three weeks. Post-transplant, they would be reviewed at regular intervals for surveillance of graft function and patient’s well being with emphasis on identifying episodes of acute rejection and infection. Currently the one-year survival post heart transplantation is 85-90%. About 30-40% may develop chronic rejection in the form of cardiac allograft vasculopathy by 5 years and 60% are expected to survive beyond 10 years post-transplant. Majority of heart transplant recipients return to a normal quality of life and 30% return to active employment.
Advanced heart failure due to dilated and ischemic cardiomyopathies, complex congenital heart disease and life-threatening arrhythmias despite optimal treatment. Prior to consideration of transplantation, a comprehensive evaluation of the patient is carried out including a thorough multiorgan and multidisciplinary workup. Some of the contraindications to a transplant include irreversible pulmonary hypertension, recent history of malignancies, active infection and multiple organ dysfunction. Suitable candidates are placed on the waitlist for transplantation. After surgery, they would be commenced on lifelong immunosuppression and managed by a multidisciplinary team with attention to rehabilitation and typical discharge from the hospital within two to three weeks. Post-transplant, they would be reviewed at regular intervals for surveillance of graft function and patient’s well being with emphasis on identifying episodes of acute rejection and infection. Currently the one-year survival post heart transplantation is 85-90%. About 30-40% may develop chronic rejection in the form of cardiac allograft vasculopathy by 5 years and 60% are expected to survive beyond 10 years post-transplant. Majority of heart transplant recipients return to a normal quality of life and 30% return to active employment.
Ventricular Assist Devices
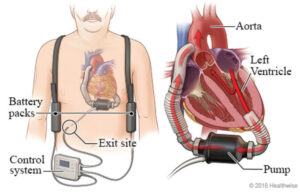 VAD could be classified as LVAD / RVAD / BiVAD / Total Artificial Heart (TAH) depending on whether they support Left / Right / both ventricles. LVAD’s have a cannula positioned in the LV cavity which connects to a centrifugal pump positioned in the pericardial space.
VAD could be classified as LVAD / RVAD / BiVAD / Total Artificial Heart (TAH) depending on whether they support Left / Right / both ventricles. LVAD’s have a cannula positioned in the LV cavity which connects to a centrifugal pump positioned in the pericardial space.
This propels the blood through an outflow cannula that is sutured to the ascending aorta, thereby decompressing the LV.
Latest devices such as the Heartmate 3 are designed with magnetically levitated propulsion which significantly reduces the trauma to blood components.
They typically provide a non-pulsatile flow and patients require anticoagulation and regular follow ups.
In the context of concomitant RV failure, some patients require both ventricles to be supported which in some instances is best configured with a single TAH.
Outcome with VAD therapy has improved significantly with survival of 75-85% at two years.
Lung Transplantation
Lung Transplantation[18] is an advanced life-saving treatment for patients with irreversible, progressive chronic lung failure. The common causes of irreversible lung failure include interstitial lung disease, chronic obstructive pulmonary disease, pulmonary artery hypertension and bronchiectasis, but several other less common lung diseases with respiratory failure can also be treated by transplantation. By transplantation, diseased lungs are replaced by healthy donor lungs, thereby stopping the worsening of lung disease, negating oxygen requirement and giving a second chance at a long, healthy and productive life.
Success and survival rate after a Lung Transplant?
More than 6000 lung transplants happen worldwide each year, but less than 100 are reported in India yearly. Kauvery Hospital[19] has a fully-dedicated, holistically staffed on-site Heart, Lung and Heart-Lung Transplant team, with good access to allied and necessary specialities of rehabilitation, nutrition, transplant infectious diseases, hematology and nephrology. It is critical to refer patients before they become frail and are in the “transplant window”, as indicated above, to have good outcomes and reduce the costs of transplantation.
Interstitial Lung Disease
Interstitial lung disease (ILDs) refers to a group of more than 400 diseases that cause progressive loss of lung volume and can cause chronic respiratory failure. The most common causes of ILDs are Idiopathic Pulmonary fibrosis (IPF), Hypersensitivity pneumonitis (commonly to pigeon exposure, exposure to fungal spores through humidifiers etc.), connective-tissue related ILDs (Scleroderma, Rheumatoid arthritis[20], Sjogren’s syndrome, MCTD and myositis-related) and occupation-related (Pneumoconiosis).
Other ILDs like Sarcoidosis, Lymphangioleiornyomatosis, Langerhans cell histiocytosis and rarer inherited ILDs also benefit from lung transplantation when treatments fail to stop worsening lung function, and respiratory failure worsens on oxygen. Anti-fibrotics reduce lung function decline by 50% but do not halt the decline in the vast majority of patients and do not reverse fibrosis when started in respiratory failure. Unfortunately, ILDs can also be associated with sudden, unexpected worsening (acute exacerbation) that can result in death. It is important to refer patients when their lung function worsens, rather than when they become bed-bound on oxygen and not fit for lung transplantation.
Chronic Obstructive Pulmonary Disease (COPD)
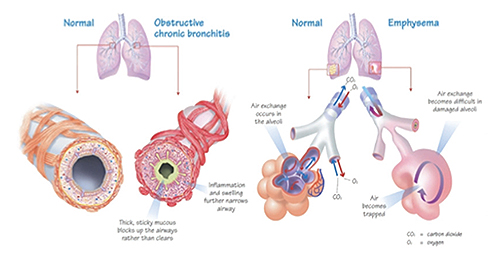 COPD is a common, preventable but progressive disease that is characterized by persistent symptoms, progressive lung function decline, repeated exacerbations that lead to hospitalizations. Most cases are related to smoking but 40-45% of patients in India are due to indoor air pollution (biomass fuel in childhood), occupational exposure, outdoor pollution, childhood respiratory infections and remodelled poorly managed asthma[21].
COPD is a common, preventable but progressive disease that is characterized by persistent symptoms, progressive lung function decline, repeated exacerbations that lead to hospitalizations. Most cases are related to smoking but 40-45% of patients in India are due to indoor air pollution (biomass fuel in childhood), occupational exposure, outdoor pollution, childhood respiratory infections and remodelled poorly managed asthma[21].
COPD[22] is the second most common cause of death annually in India and is the only top 5 cause of death that is increasing in India. About 8,33,000 patients are estimated to die annually due to COPD in India and it is estimated that 4.1% of our population has COPD (estimated 55.3 million). While India accounts for 18% of the world’s population, we contribute to 32% of the worldwide COPD deaths. Lung Transplant is an effective treatment for advanced COPD patients that have stopped smoking, are able to undergo rehabilitation, are using tallharisrom oxygen and/or BiPAP and have repeated exacerbations, need hospitalization or have pulmonary hypertension related to COPD. Appropriately referred patients have a survival benefit and a huge quality of life benefit from lung transplantation.
Pulmonary Hypertension (PH)
 Pulmonary hypertension can be due to pulmonary arterial hypertension (Group 1), left heart disease (Group 2), lung disease and hypoxemia (Group 3), chronic thromboembolic pulmonary hypertension (CTEPH, Group 4) and other specific conditions (Group 5 e.g sarcoidosis). Group 1 PH is a progressive disease and treatment options are limited in
Pulmonary hypertension can be due to pulmonary arterial hypertension (Group 1), left heart disease (Group 2), lung disease and hypoxemia (Group 3), chronic thromboembolic pulmonary hypertension (CTEPH, Group 4) and other specific conditions (Group 5 e.g sarcoidosis). Group 1 PH is a progressive disease and treatment options are limited in
India as prostacyclins are difficult to access due to cost and administration concerns. Bilateral Lung transplantation alone (without heart – lung transplantation) is an effective treatment and iPAH has the longest conditional survival among indications for transplantation. Pulmonary hypertension due to hypoxemic lung disease (ILD, COPD) indicates poor prognosis and these patients are candidates for early referral for bilateral lung transplant. Patients with CTEPH that are not candidates for pulmonary thromboendarterectomy are also candidates for lung transplant evaluation. As right ventricular function worsens with dysfunction, bilateral lung transplantation alone becomes difficult and heart – lung transplantation (HLT) becomes the only option. HLT increases costs of transplantation and monitoring for rejection post – transplantation and reduces heart donor pool. These are the reasons timely referral before significant right ventricular dysfunction sets in is direly needed.
Bronchiectasis
Bronchiectasis[23] is characterised by abnormal, permanent dilatation of the airways due to a variety of causes. Indian patients with bronchiectasis vary from western patients in significant ways. Cystic Fibrosis is relatively less common; tuberculosis, ABPA and post-infectious bronchiectasis are more common. Indian patients present with more advanced bronchiectasis and more symptoms. There are no approved treatment options for bronchiectasis, and treatment options include identification and treatment of the cause, postural drainage, vaccination, treatment and prevention of exacerbations. Patients often present with sufficiently advanced disease, and this is irreversible, by definition. Lung transplantation is a life-saving treatment at this stage, as indicated below.


Please contact us at +91 9150277712 for approx. cost details.
Frequently Asked Questions
1. When a heart transplant is considered necessary?
A heart transplant is considered for advanced heart failure when other treatments are no longer effective. Symptoms include frequent decompensation and poor survival rates.
2. What is a ventricular assist device (VAD/RVAD/LVAD/BiVAD )?
A VAD is a pump that supports a failing heart. It can be used as a bridge to recovery, decision-making, or heart transplantation. In some cases, it can be used for long-term support.
3. What are the most common reasons for lung transplantation?
Lung transplantation is used for irreversible lung failure caused by conditions like COPD, pulmonary hypertension, bronchiectasis, and interstitial lung disease.
4. How successful are heart and lung transplants?
One-year survival rates for heart transplants are around 85-90%. Long-term survival rates for lung transplants vary depending on the underlying condition.
5. What are some of the risks associated with heart and lung transplants?
Rejection and infection are major risks associated with both heart and lung transplants. Medications are used to manage rejection, and close monitoring helps to identify infections early.
6. Where can I find more information about advanced heart and lung failure treatment?
Consult a cardiologist or pulmonologist[24] for personalized advice. You can also visit the website of a hospital specializing in heart and lung transplants, like Kauvery Hospital.
Kauvery Hospital is globally known for its multidisciplinary services at all its Centers of Excellence, and for its comprehensive, Avant-Grade technology, especially in diagnostics and remedial care in heart diseases, transplantation, vascular and neurosciences medicine. Located in the heart of Trichy (Tennur, Royal Road and Alexandria Road (Cantonment), Chennai, Hosur, Salem, Tirunelveli and Bengaluru, the hospital also renders adult and pediatric trauma care.
Chennai – 044 4000 6000 • Trichy – Cantonment – 0431 4077777 • Trichy – Heartcity – 0431 4003500 • Trichy – Tennur – 0431 4022555 • Hosur – 04344 272727 • Salem – 0427 2677777 • Tirunelveli – 0462 4006000 • Bengaluru – 080 6801 6801
- Kauvery’s Heart Transplant Team: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q1
- What is Advanced Heart Failure?: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q2
- What is Mechanical Circulatory Support?: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q3
- Heart Transplantation: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q4
- Ventricular Assist Devices ( LVAD / RVAD / BiVAD /TAH): https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q5
- Lung Transplantation : https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q6
- Success and survival rate after a Lung Transplant?: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q7
- Interstitial Lung Disease : https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q8
- Chronic Obstructive Pulmonary Disease (COPD) : https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q9
- Pulmonary Hypertension (PH) : https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q10
- Bronchiectasis?: https://kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre#q11
- Transplant Surgeons: https://www.kauveryhospital.com/doctors/chennai/heart-and-lung-transplant/
- Transplant Cardiologists: https://www.kauveryhospital.com/doctors/chennai/cardiothoracic-surgery/dr-kumud-kumar-dhital/
- Heart failure: https://kauveryhospital.com/blog/heart-health/causes-and-types-of-congestive-heart-failure/
- ECMO: https://www.kauveryhospital.com/ecmo
- What is ECMO? How Does the ECMO Machine Work?: https://kauveryhospital.com/blog/heart-health/what-is-ecmo/
- heart transplantation: https://www.kauveryhospital.com/heart-failure-and-transplantation-centre
- Lung Transplantation: https://www.kauveryhospital.com/centers-of-excellence-and-specialties/lung-transplant-program
- Kauvery Hospital: https://www.kauveryhospital.com/
- Rheumatoid arthritis: https://kauveryhospital.com/blog/orthopedics/what-is-rheumatoid-arthritis/
- asthma: https://kauveryhospital.com/blog/pulmonology/what-is-asthma/
- COPD: https://kauveryhospital.com/blog/pulmonology/early-warning-signs-of-copd/
- Bronchiectasis: https://kauveryhospital.com/blog/pulmonology/bronchiectasis-symptoms-causes-treatment/
- pulmonologist: https://www.kauveryhospital.com/centers-of-excellence-and-specialties/pulmonology-doctors/chennai/
Source URL: https://www.kauveryhospital.com/blog/transplantation/kauvery-heart-lung-transplant-centre/