CASE REPORT:
Our patient is a 50-year-old lady diagnosed with Scleroderma (SSc) eight years ago. She developed Interstitial lung disease (ILD) five years ago and was being managed with Mycophenolate mofetil 540 mg twice a day. Unfortunately, she continued to worsen with breathlessness on daily activities and worsening lung function detected by pulmonary function testing (PFTs) and fibrosis on Computed Tomography (CT) scans. Nintedanib was added but she continued to have an absolute 10% fall in Forced vital capacity (FVC 1.5L, 58% Pred to 1.3L, 49%) and DLco at 3 months of Nintedanib 150 mg twice a day. She was not on oxygen at this stage but had desaturation (resting 94% to 75% on six-minute walk test) on exertion. She was referred to us for lung transplant evaluation. She underwent a thorough evaluation for lung transplantation (LT) that revealed a set of complex challenges. Several centers abroad do not accept SSc-ILD because of the concern of aspiration due to poor movement of the esophagus which can cause permanent damage to the lung graft. Additional concerns in her were frailty; body-mass index (BMI) of 34 kg/m2; severe pre-capillary pulmonary hypertension (mPAP 36, PVR 6 WU, PcWP 8 mm Hg) and immunological sensitization-she had antibodies (multiple anti-HLA Class I and DRB16) against potential donor lungs. If the potential donor lungs were to react with these pre-formed antibodies, it could lead to hyperacute or acute rejection.
Esophageal function was evaluated with 24-hour impedance manometry, pH studies and gastric emptying tests. Motility was improved through medical management and care was taken to ensure no reflux into the proximal part of her esophagus, to limit the risk of aspiration into the lungs. Her disease was optimized with input from our Rheumatologist and gastroenterologist. Nutrition and rehabilitation support were intensified to reduce her BMI to 32 kg/m2, while keeping her physically active. She was added to the transplant list and was awaiting a suitable donor for nine months. Over this period, she continued to worsen, needing 8 liters of oxygen at rest during the day and home ventilator support at night. She also had two episodes of exacerbations. Given our concern was initially to avoid anti-HLA cross-matches, several blood group and size-matched donor lungs were declined and she continued to worsen without transplant. Subsequently, we changed our strategy and accepted low-level single antigen virtual cross match (VXM) as long as actual crossmatch (AXM, AHG-CDC) was negative; we planned to manage this with adjustment of her immunosuppression. Finally, an appropriate age and size-matched donor who was actual cross-match negative (single allele A*11 VXM+) became available after 14 months on the transplant list. Bilateral lung transplant with central ECMO support was done. She was weaned off the ventilator support within 24 hours and oxygen support by 4th day post-transplant. She was able to walk normally and use the stairs without difficulty by day 10. She was discharged home on the 12th post-operative day. Her lung function continues to improve and she is doing well with resumption of independent daily activities at home.
DISCUSSION:
Lung involvement in Scleroderma is typically Non-specific Interstitial Pneumonia (NSIP), but can be Usual interstitial Pneumonia (UIP), organizing pneumonia, sarcoidosis, Pulmonary hypertension (PH) and veno-occlusive disease. Early detection of lung disease and pulmonary hypertension is crucial as disease is better treated at this stage (Table 1). While up to 90% of patients can have interstitial abnormalities on CT chest, about 25% develop clinically relevant ILD, often within three years of diagnosis. Spirometry and DLco performed biannually in the initial five years after diagnosis and then annually detects early lung disease. CT scans are reserved for those with abnormal lung function tests only. In the current era, ILD is the leading cause of SSc-related mortality.
Echocardiography performed annually to detect PH has several limitations. It is observer-dependent and tricuspid regurgitant jet (TR) is not present in all patients and TR jet velocity does not accurately reflect invasive pressures. The DETECT algorithm is a validated model to diagnose early SSc-PH. SSc patients are evaluated in step 1 based on their risk profile (prior telangiectasia, anti-centromere antibodies) annually with a panel of tests including ECG; Lung function (FVC, DLco); urate and NT-Pro-BNP levels. Based on this step 1 results and findings on Echocardiography, a decision on right heart catheterization is made (Figure 1).
SSc-ILD is managed with immunosuppression. Currently, Mycophenolate mofetil (MMF) is the first choice as the SLS study showed similar efficacy with better toxicity profile of MMF over Cyclophosphamide. Cyclophosphamide or Rituximab is often used in patients progressing on MMF, but there is no evidence of superiority of either over MMF in this situation. Toclizumab 162 mg weekly subcutaneously (fascinate, focuSSced) is another option for patients not tolerating MMF or CYC and having ongoing Ground-glass opacity on CT or elevated CRP. In patients with worsening fibrosis on CT or worsening lung functions and symptoms, the anti-fibrotic nintedanib has shown an attenuation in the rate of lung function decline (difference 41 mL/year, 95% CI 2.9-79 at 52 weeks, SENCIS). Prognostic models for SSc-ILD are limited. In general, SSc-ILD has a 9-year survival of 30% compared to 72% in SSc without any organ involvement (p<0.0001, N=953 patients, 19% had ILD over a 10-year follow up period and 45-50% developed in the first 3 years).
Among patients with SSc-ILD enrolled in clinical trials, mortality has 25% at 4 years, and 45-50% at 8 years. Good scoring models are lacking in SSc-ILD to select for lung transplantation. Using a scoring system with smoking (never, ever), age (55-70, >70) and DLco (40-60%, <40%), higher scores (6-7) had a 1-year, 2-year and 3-year mortality of 12.8%, 34% and 56.8%. These figures are substantially lower than survival figures after LT for SSc-ILD. In general, patients progressing on MMF should be evaluated for LT while nintedanib or Rituximab are being instituted, especially in those with low FVC and DLco at baseline. Transplant listing should occur when FVC declines >10% and DLco declines>15% on nintedanib or Rituximab.
Lung transplantation (LT) may be an option for carefully selected SSc patients with severe ILD and SSC-PAH that is not responsive to pharmacologic interventions. However, there are several additional concerns while evaluating a candidate with SSc-ILD for lung transplantation. These include
- Esophageal dysmotility and concerns over aspiration and pneumonia (and concerns over mycophenolate related GI side effects and worsening gastroparesis)
- High incidence of PH
- Abnormal chest wall mechanics due to skin tightening
- Systemic involvement including concern over renal disease (and the effect of steroids and CNI post lung transplantation)
- Nutrition and its management, including while on wait list
- Concern over disease recurrence
With careful selection, outcomes after LT in carefully selected patients with SSc-ILD and PAH are comparable to other ILDs (Table 2)
CONCLUSIONS:
Scleroderma is a common connective tissue disease and clinically relevant Interstitial lung disease can complicate the course in 25-40%. While the rate of decline in lung function is lower than idiopathic pulmonary fibrosis, SSc-ILD patients are younger and and can develop respiratory failure on anti-fibrotics even with attenuated lung function decline. Carefully selected patients with SSc-ILD and SSc-PAH benefit from bilateral lung transplantation with similar outcomes.
Table 1. Approach to SSc-related lung disease
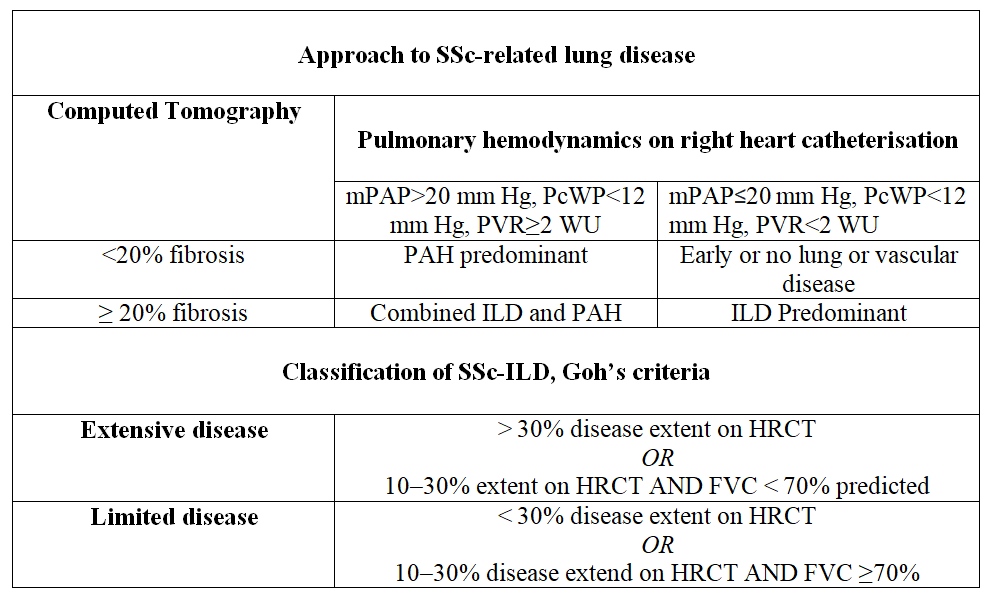
Table 2. Studies Evaluating Safety of Lung Transplantation In Scleroderma
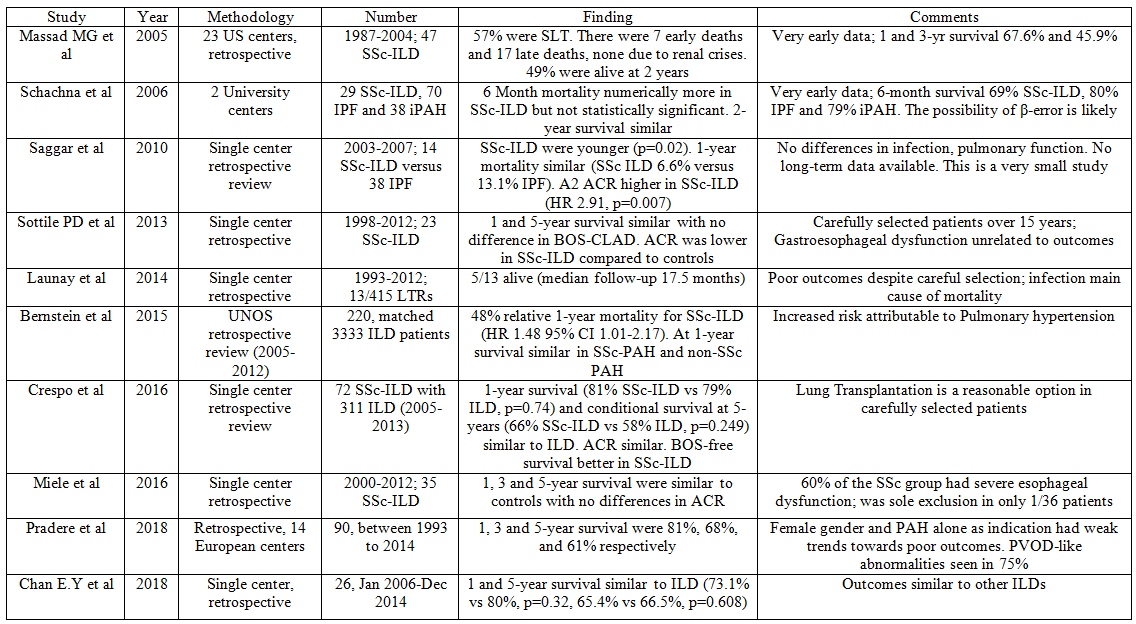
Abbreviations: SSc-ILD Systemic sclerosis interstitial lung disease, iPAH idiopathic pulmonary arterial hypertension, IPF Idiopathic pulmonary fibrosis, US United States, UNOS, United Network for Organ Sharing, SLT Single lung transplantation, ACR Acute cellular rejection, BOS bronchiolitis Obliterans syndrome, CLAD Chronic Lung Allograft dysfunction, PVOD Pulmonary veno-occlusive disease, LTs Lung transplant recipients
Corresponding Author:
 Dr. Srinivas Rajagopala
Dr. Srinivas Rajagopala
Senior Consultant, Interventional Pulmonology & Sleep Medicine,
Director, Transplant Pulmonology & Lung Failure Unit
Kauvery Hospital



