Case Report:
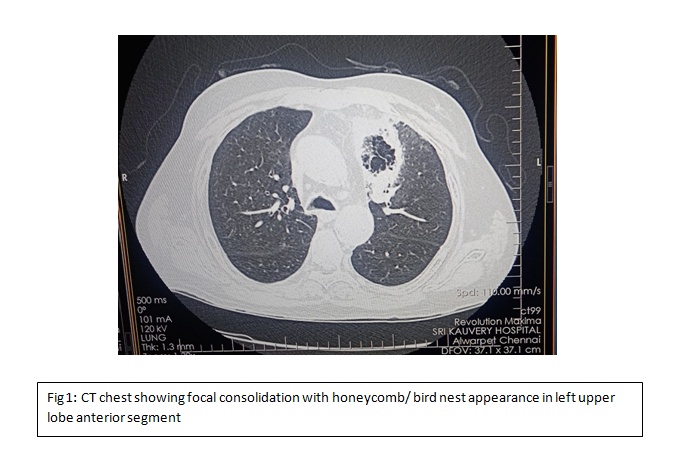
A 63 year old male, a known case of type 2 Diabetes Mellitus, Systemic Hypertension and chronic IgG4 pancreatitis for past 3 years on oral steroids presented to ER with complaints of fever on & off associated with productive cough with left eyelid drooping and loss of left eye vision since 10 days. He was diagnosed with IgG4 Pancreatitis on Oct 2020 and started on steroids. On arrival, patient was conscious, oriented, febrile, icteric, tachypneic and tachycardic with bilateral extensive crepitations on auscultation. On examination of left eye, eyelid was drooping and pupil not reactive with extraocular movements full. Patient was admitted in ICU with a provisional diagnosis of fungal pneumonia/ ARDS. CT chest showed focal consolidation with central honeycomb/ bird nest appearance in left UL anterior segment (Fig 1). Patient was started on Inj. CASPOFUNGIN empirically and samples sent for fungal culture and sensitivity and put on non-invasive ventilation. MRI Brain with orbit showed no meningeal enhancement; no cavernous sinus thrombosis/ SOV thrombosis. MRI PNS showed mucosal thickening in right maxillary, left sphenoid & ethmoid sinuses with heterogenous enhancing and non-enhancing areas, characteristic of fungal sinusitis. As patient condition remained the same, antifungal was escalated to liposomal amphotericin B & IV ceftriaxone were added. Bronchoscopic alveolar lavage (BAL) was done, and culture grew pseudomonas & MRSA. Furthermore, BAL fungal panel detected Rhizopus & Mucor. Nasal swab grew MRSA. IV Linezolid added according to sensitivity pattern. As patient condition remained the same, after anaesthetic clearance, patient was taken up for left anterior and posterior ethmoidectomy & left upper lobectomy. Anterior mediastinum was opened up, which showed invasive mucor lesions invading thoracic aorta (Fig 2), which is a severe form of mucormycosis and carries very poor prognosis. Left upper lobectomy and ethmoidectomy was done and patient was started on ionotroph support. Patient developed bradycardia and asystole the next day. In spite of resuscitative measures, reversal of spontaneous circulation was not obtained.
Discussion:
Mucormycosis represents a group of life-threatening infections caused by fungi, which are typically ubiquitous environmental organisms, primarily affects immunocompromised individuals. The fungal belong to the order Mucorales of the subphylum Mucormycotina. The most commonly isolated species are Rhizopus, mucor, rhizomucor & cunninghamella. Immunosuppressed individuals are at greater risk of being infected. These include patients with diabetes, post-transplant individuals, chronic steroid use, prolonged neutropenia, HIV, leukemia, etc.
Mucormycosis presents as several clinical forms – rhinoorbito cerebral, pulmonary, cutaneous, gastrointestinal and disseminated disease. However, its clinical manifestations are varied, the progression of the disease is very rapid and highly invasive. Rhino-orbito-cerebral mucormycosis is more common in patients with diabetes mellitus, whereas pulmonary form is more common in leukemia and post-transplant individuals. The route of entry of organism decides the type of infection. The most common form in the world being rhino-orbito-cerebral disease presents as facial pain, facial numbness, conjunctivitis and blurring vision which ultimately results in orbital cellulitis, vision loss and ophthalmoplegia. Pulmonary mucormycosis is the second most common form, presenting dyspnea, cough, fever and chest pain. Angio-invasion result in necrosis and/or haemoptysis. Cutaneous form may result from external implantation of the fungus such as soil exposure from trauma, penetrating injury from plant material, catheter insertion, use of tape to secure endotracheal tubes, etc. Cutaneous form is highly aggressive that it invades muscle, fascia and even bone rapidly.
Gastrointestinal form results in non-specific abdominal pain associated with nausea and vomiting. The disease may progress to visceral perforation and peritonitis. Hematogenously disseminated mucormycosis originate from primary site of infection and may affect any organs. Mortality rates for widely disseminated mucormycosis exceed 90%. Most of the symptoms are non-specific, for this reason, a clinician must have a high index of suspicion to diagnose the disease in any of its forms.
Imaging techniques (CT, MRI) helps in identifying the lesion but often yield subtle findings tat underestimate the extend of disease. However definitive diagnosis includes a positive culture from a sterile site or the detection of fungal elements from histopathological examination,
Successful treatment of mucormycosis involves four steps (1)Early initiation of therapy, (2)Surgical debridement when possible, (3)Rapid reversal of underlying predisposing risk factors if possible and (4)Proceeding to treat underlying malignancy, without waiting to complete antifungal therapy first.

 Dr Prabhakaran M
Dr Prabhakaran M
DNB Internal Medicine Resident (1st year)
Kauvery Hospital Chennai



