The Electrocardiogram remains a crucial tool in the identification and management of acute myocardial infarction. A detailed analysis of patterns of ST segment elevation may influence decisions regarding the perfusion therapy. This study is undertaken to identify the culprit vessel from ECG in patients with acute ST elevation myocardial infarction and correlate with coronary angiogram.
This study is a prospective study. The study population consisted of 100 patients with STEMI. With inclusion criteria of Adults ≥ 18 years with symptoms of ACS, patients with new myocardial infarction, ST segment elevation of >1mm in Limb leads and >2mm in chest leads and the exclusion criteria includes patients with known history of structural heart disease that could alter ECG interpretation, previous MI patient, patients who have undergone revascularization procedures before ECG recording, individuals who already have a pacemaker.
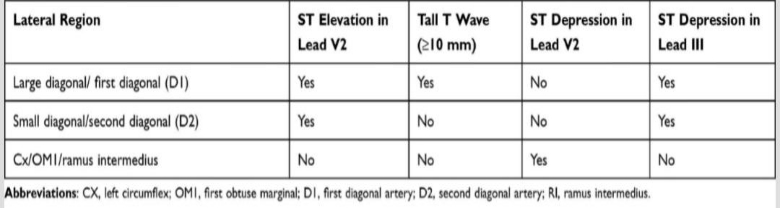
The development of a reliable protocol for identifying the culprit vessel in ACS based on ECG findings. ILKAY Classification to specifically identify the culprit vessel in cases of lateral wall MI with coronary angiography.
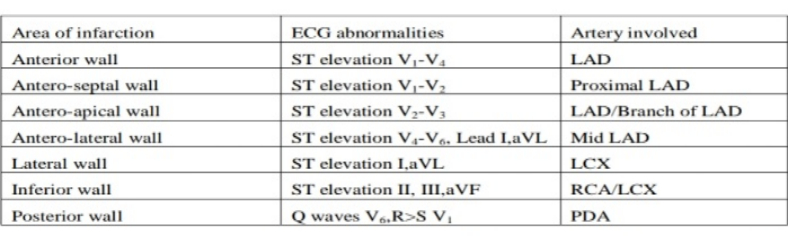
For Inferior Wall MI:
# RCA occlusion:
- ST ↑ in Lead III> Lead II
- ST ↓ > 1mm in Lead I & avL
- Proximal RCA occlusion:
- ST ↑ > 1mm Lead V4
- ST ↑ in Lead V1
- ST ↓V3 / ST ↑ lead III < 0.5
- Distal RCA occlusion:
- . ST coving without ST ↑ in lead V4
- . ST↓ V3/ ST↑ lead III 0.5 to 1.2
# LCX (Left circumflex occlusion):
- ST ↑in lead II > III
- Isoelectric on ST ↑ in Lead I , avL
- ST↓ V3/ST ↑ lead III > 1.2
- ST V4 that slopes into negative T wave
For Anterior Wall MI:
# Occlusion Proximal to S1:
- .ST↑ in Lead V1 > 2.5mm
- Complete RBBB
- ST ↑ in lead aVR
- ST ↓ in Lead V5
- ST ↓ in inferior leads > 1.0 mm( II, III, avF)
# Occlusion Proximal to D1:
- Q wave in Lead aVL
- ST ↓ in inferior leads
# Occlusion Distal to S1:
- Q wave in Lead V4- V6
- Absence & ST & in inferior leads
#Occlusion distal to D1:
- ST ↓ in Lead avL
- Absence of ST ↓ in inferior loads
Categorical variables will be presented as number and percentage (%) and continuous variables will be presented as mean ± SD.
Odds ratio with 95% confidence intervals and positive predictive values (PPV), negative predictive value (NPV) will be calculated for selected variables and their significance. A p value of <0.05 was considered statistically significant.
This protocol outlines a systematic approach to identifying the culprit vessel in ACS using ECG data, with defined inclusion and exclusion criteria.
The admission ECG in patients with ST elevation acute myocardial infarction is valuable not only for determining who should and should not receive early reperfusion treatment, but also for providing information regarding the location and extent of acute myocardial injury. By reflecting the pathophysiology of the myocardium during acute ischemia important information to guide management and determine prognosis can be derived from the electrocardiogram. Electrocardiographic markers of proximal coronary artery occlusion identify relatively large myocardial infarctions that benefit most of the early and complete revascularization strategies such as angioplasty. These criteria although are not the substitute of invasive procedure for differentiating the culprit artery in acute myocardial infarction, but provides an economical, reliable and quick method of differentiating infarct related artery in acute myocardial infarction.
REFERENCES:
1.World Health Organization. The World Health Report 2002: Reducing risks, promoting healthy life.: WHO; 2002.
2.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary. A report of the American College of Cardiology/American Heart Association task Force on practice guidelines (Committee on management of acute Myocardial infarction)CCirculation.
3.Bertrand ME, Simoons ML, Fox KA, et al. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation. Recommendations of the Task Force of the European Society of Cardiology. Eur Heart J
4.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, et al. 2007 focused update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction:. J Am coll Cardiol.
5.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study):case-control study.


 Dr. Niveda R
Dr. Niveda R Guide: Dr. Aslesha Sheth
Guide: Dr. Aslesha Sheth