Abstract
Fat embolism is a life threatening complication following a major orthopedic trauma. Diagnosis is only by strong clinical suspicion. Treatment is only supportive care. Here, we report a young male who presented with altered sensorium 48 hours after trauma, diagnosed as fat embolism and managed effectively with multi-disciplinary approach.
Introduction
Fat embolism is defined by the presence of fat globules in pulmonary circulation. Fat embolism syndrome refers to the systemic manifestations due to presence of fat globules in circulation. Fat embolism was first described by Zenker et al in 1873(1). Von Bergmann first clinically diagnosed fat embolism. Fat embolism syndrome presents with a triad of hypoxemia, neurological abnormalities and petechial rash. The actual incidence of fat embolism syndrome ranges from 1 to 30% due to lack of universal diagnostic criteria(2). This case report describes the management of fat embolism in our hospital.
Case presentation
A 21 years old male had a history of fall while playing on beach. There was no history of loss of consciousness or ENT blood. He sustained injury over his right hip. He was initially taken to nearby hospital where he was diagnosed as fracture of shaft of right femur. His fracture was stabilized with POP. He was hemodynamically stable at admission. He developed respiratory distress 48 hours after admission and intubated for the same and shifted to kauvery hospital for further management. On arrival he was confused, agitated, moved all 4 limbs. On examination he had petechial rashes over his chest as shown in figure 1.

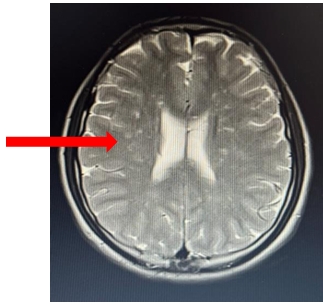
His MRI brain showed symmetrical non confluent high DWI, microhaemorrhagic signal foci in bilateral centrum semiovale, subcortical white matter, basal ganglia, thalami, splenium of corpus callosum & brain stem. The MRI image is shown figure 2
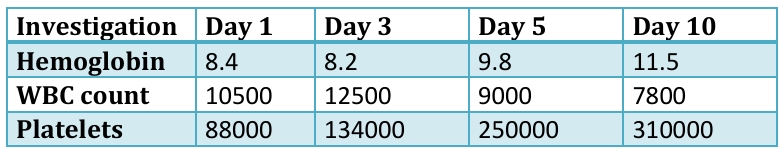
He was on mechanical ventilation in ICU. His lab investigatons was illustrated in table.1.
He was diagnosed as fat embolism syndrome (FES). His sensorium improved and he was extubated. Right femur nailing was done as early as possible, mobilized and shifted to ward. He was discharged in stable condition.
Discussion
Fat embolism occurs following major orthopedic trauma involving fracture of long bones like femur, tibia or pelvic bone fracture or following orthopedic procedures like knee arthroplasty and intra medullary nailing.
Other non-traumatic causes include
- Acute or chronic pancreatitis
- Therapy with corticosteroid
- Infusion of fat emulsion
- Lymphography
- Hemoglobinopathies- Sickle cell disease and Thalassemia
Pathophysiology
Exact pathophysiology is not known. Two theories have been proposed.
Mechanical theory
Fat from disrupted bone marrow or adipose tissue enters torn venules following trauma. This is supported by the presence of echogenic material passes through the right heart during orthopedic surgeries (3,4). Fat embolism sufficiently explains the respiratory symptoms of fat embolism syndrome since fat globules collect and obstruct pulmonary capillaries. In addition, it is thought that circulating fat cells may have prothrombotic potential and may trigger the aggregation of platelets and fibrin resulting in further obstruction of the pulmonary vascular bed. When massive, this process may lead to right ventricle failure and obstructive shock. Effects on systemic circulation can be explained by the presence of right –left shunts or by microembolism.
Biochemical theory
Production of toxic intermediaries of circulating fat is an alternative theory about the mechanism of FES, which may occur instead of or in addition to the mechanical mechanism described above. This theory is based upon the hypothesis that embolized fat degrades into toxic intermediaries with proinflammatory effects and is supported by elevated levels of the free fatty acids and cytokines which can explain ARDS in fat embolism(5).
Clinical features
Fat emulsion syndrome usually has an asymptomatic interval for about 12 to 72 hours after initial insult and is then followed by a classical triad of findings—respiratory insufficiency, petechial rash, and neurologic manifestation. Pulmonary manifestation is the earliest symptom and can be seen in 75% of patients[6]. Symptoms are usually nonspecific, for example, headache, acute confusion, convulsion, or as severe as coma. Dermatologic manifestation is usually seen within 24 to 36 hours and usually distributed in nondependent regions of the body such as conjunctivae, head, neck, anterior thorax or axillary areas. Most rashes typically disappear within a week. Other nonspecific symptoms include fever, thrombocytopenia, jaundice, lipuria, haematuria, and retinopathy [7]. In severe cases, FES can be complicated by disseminated intravascular coagulation, right ventricular dysfunction, shock, and death.
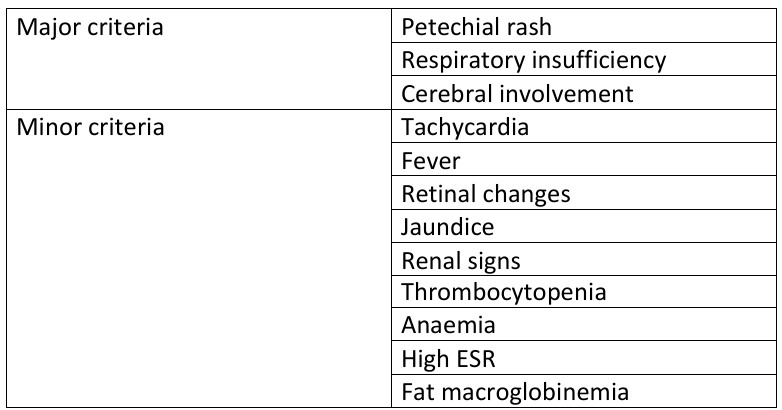
There are no universal criteria for diagnosis of FES. Diagnosis is made by clinical suspicion and characteristic findings on imaging methods. However, there have been three previously proposed criteria by different authors: Gurd, Schonfeld, and Lindeque. Gurd’s criteria were used most widely, and the diagnosis of FES requires at least two major criteria or one major criterion plus two minor criteria. This is explained in following table
Diagnosis
Laboratory findings in FES are usually nonspecific. Some patients may develop thrombocytopenia, anemia, or even hypofibrinogenemia. Many imaging modalities can facilitate the diagnosis of FES, but none is specific. Chest radiographic findings may show diffuse bilateral patchy infiltrates. Noncontrast CT scans of the brain may be normal or reveal diffuse white matter petechial hemorrhage. MRI of the brain is sensitive for detecting FES.
Its findings consist of diffuse, non-confluent, and hyperintense lesions in both white and gray matter on diffuse wedge images and T2-weighted images, also called “star-field” pattern. These lesions gradually disappear within a few weeks to a few months [7]. Transcranial Doppler ultrasound (TCD) can also be used for detecting microembolic signals (MES) in patients with FES.
Treatment
The mainstay management of FES is preventive and supportive. Supportive correction of hypoxemia with supplement oxygen or mechanical ventilation. Additionally, monitoring of hemodynamic status and maintenance of blood volume is important in FES because shock can exacerbate the lung injury caused by FES. If patients exhibit neurologic involvement, frequent neurological examination should be done. No specific drug is recommended or has strong evidence for treatment of FES. Systemic corticosteroids, which may reduce inflammation, perivascular hemorrhage, and edema, may have benefit in patients with deterioration of lung functions, but there is no systematic evidence to back up such benefit(8). Heparin has been proposed as a treatment of FES, due to its stimulatory effect on lipase activity and clearance of lipid from the circulation. Early stabilization of long bone fracture is recommended to minimize bone marrow embolization into the venous system.
Prognosis
Most patients with FES fully recover spontaneously. In most cases, findings are transient and fully reversible, often within a few days, although features may persist beyond one week when FES is severe(9). Mortality rate ranges from 5 to 15 % (10, 11). Cause of death in FES will be respiratory failure, refractory shock or brain death.
Conclusion
Patients presented with long bone fracture complicated by fat embolism needs comprehensive care. Early diagnosis and early stabilization of fracture prevents further fat embolism. Although treatment modality is only supportive therapy, timely diagnosis early fracture stabilization is the key.
Referances
- F. A. Zhenker, Beitrage zur Anatomie und Physiologie de Lung, J Braunsdorf, Dresden, Germany, 1861.
- Stein PD, Yaekoub AY, Matta F, Kleerekoper M. Fat embolism syndrome. Am J Med Sci 2008; 336:472.
- Pell AC, Hughes D, Keating J, et al. Brief report: fulminating fat embolism syndrome caused by paradoxical embolism through a patent foramen ovale. N Engl J Med 1993; 329:926.
- Takahashi S, Kitagawa H, Ishii T. Intraoperative pulmonary embolism during spinal instrumentation surgery. A prospective study using transoesophageal echocardiography. J Bone Joint Surg Br 2003; 85:9
- Kao SJ, Yeh DY, Chen HI. Clinical and pathological features of fat embolism with acute respiratory distress syndrome. Clin Sci (Lond) 2007; 113:279
- K. A. Powers and L. A. Talbot, “Fat embolism syndrome after femur fracture with intramedullary nailing: case report,” American Journal of Critical Care, vol. 20, no. 3, pp. 4–6, 2011.
- E. M. Bulger, D. G. Smith, R. V. Maier, and G. J. Jurkovich, “Fat embolism syndrome. A 10 year review,” Archives of Surgery, vol. 132, no. 4, pp. 435–439, 1997
- Kubota T, Ebina T, Tonosaki M, et al. Rapid improvement of respiratory symptoms associated with fat embolism by high-dose methylpredonisolone: a case report. J Anesth 2003; 17:186
- Sethi D, Kajal S, Saxena A. Neuroimaging findings in a case of cerebral fat embolism syndrome with delayed recovery. Indian J Crit Care Med 2015; 19:674.
- Fulde GW, Harrison P. Fat embolism–a review. Arch Emerg Med 1991; 8:233.
- Bederman SS, Bhandari M, McKee MD, Schemitsch EH. Do corticosteroids reduce the risk of fat embolism syndrome in patients with long-bone fractures? A meta-analysis. Can J Surg 2009; 52:386


 Dr Dinesh Raj
Dr Dinesh Raj