A Case Report:
A 63-year-old gentleman with longstanding diabetes and hypertension with a history of papillary carcinoma of thyroid for which thyroidectomy was done 25 years ago, now presented with bilateral lower limb swelling and oliguria for 3 weeks associated with frothy urine. There was also a history of native medicine intake for the past 3 months for some skin lesion over the neck.
On examination there was pedal edema and his BP was 200/80 mmHg. Urine routine showed 3+ proteinuria with granular casts. Urine protein creatinine ratio was 2.2. Serum creatinine was 1 mg/dl, serum albumin was 3.1 mg/dl. Ultrasound KUB showed normal sized kidneys with increased echogenicity and CMD was maintained.
He underwent renal biopsy. On light microscopy, 9 glomeruli were seen. One glomerulus was globally sclerotic. There was mesangial hypercellularity in all glomeruli. Segmental endocapillary hypercellularity was seen in one glomerulus. There were no double contours or spike formation on the glomerular basement membrane. No fibrinoid necrosis or crescent formation seen. No IFTA. No inflammatory infiltrate was present in the interstitium. Blood vessels were unremarkable.
On immunofluorescence, 2 glomeruli are present. IgG (+3) showed granular positivity on the capillary loops in a segmental pattern. IgA (+3) was positive on the mesangium. C3 (+2) was positive on the capillary loops and mesangium. No light chain restriction seen. Rest of the antisera were negative.
As Immunofluorescence showed features of membranous nephropathy, additional tests were asked like PLA2R and NELL1, out of which NELL1 was positive. The final diagnosis was IgA Nephropathy and NELL1 associated Membranous Nephropathy.

Figure 1: Shows PAS staining showing mesangial hypercellularity
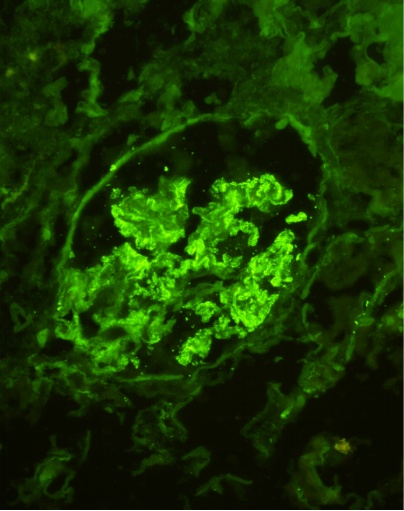
Figure 2: IF shows IgG (+3) granularity on capillary loops
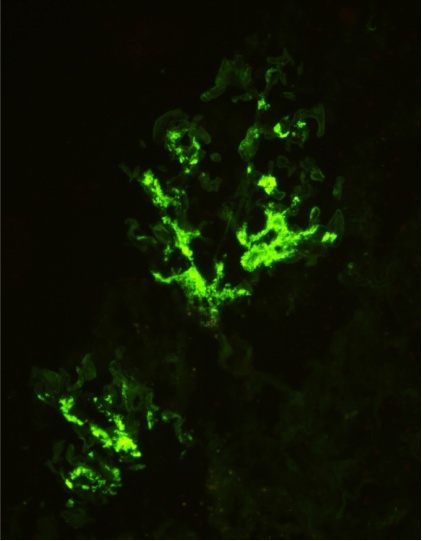
Figure 3: IF shows IgA (+3) on mesangium
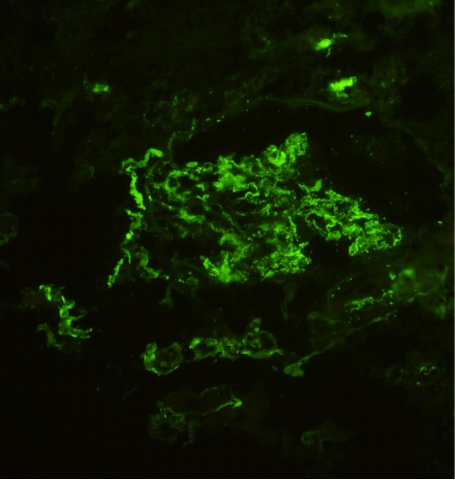
Figure 4: IF shows C3 (+2) on capillary loops and mesangium
Discussion:
IgA nephropathy and Membranous nephropathy are two types of common glomerulonephritis worldwide. The incidence of concurrent IgA nephropathy and membranous nephropathy (cIgAN-MN) is only 0.5-1% in renal biopsies.
In this case report, light microscopy shows features of IgA nephropathy and immunofluorescence shows features of membranous nephropathy. NELL1, Neural epidermal growth factor-like 1 antigen is an autoantigen more likely associated with malignancy and native medicine intake. In 2024, a study conducted by Narayanan et al has concluded that increasing incidence of NELL1 MN linked to the use of fairness creams with high mercury content which is also present in most of the indigenous medicine intake. Cessation of cream usage without immunosuppression has shown favourable clinical outcomes.
Proteinuria reduction to less than 1 g/d is a surrogate marker of improved kidney outcome in IgAN and immunosuppressives should be considered only when proteinuria is >1 g/d despite atleast 90 days of optimized supportive therapy. But in MN, immunosuppressives may not be required when proteinuria is <3.5 g/d and eGFR >60. So when two diseases coexist, the management and treatment decisions seems to be difficult.
There are only a few studies on concurrent membranous nephropathy and IgA nephropathy. But in all these studies, they have described only PLA2R antibody and nothing about NELL1. So this patient with cIgAN-MN with NELL1 positivity is quite rare.
This patient was advised to stop the indigenous medicine intake. His BP was controlled with antihypertensives. Statins and angiotensin receptor blockers were added. T. Budesonide 9 mg OD was given along with a diuretic. On follow up his proteinuria was found to be increasing and in nephrotic range. As nephrotic syndrome with IgA is treated as MCD. So, he was started on oral prednisone and is on follow up now.
 Dr. Prathibha Thangadurai
Dr. Prathibha Thangadurai
DrNB Nephrology Resident,
Kauvery Hospital, Alwarpet
 Dr. Balasubramaniyam
Dr. Balasubramaniyam
Chief Nephrologist,
Kauvery Hospital, Alwarpet