Introduction
Bronchial asthma remains one of the commonly encountered disease in pulmonology practice. It affects almost all age groups regardless of gender, ethnicity and socioeconomic status although most of the asthmatic patients remain controlled with standard inhaled mediations, up to 10% of asthma cases are severe of which approximately 40% remain uncontrolled1. This severe uncontrolled asthma carries a tenfold higher risk of mortality. This severe group of asthmatics require oral corticosteroids (OCS) which in turn can lead to its dependence and have serious irreversible adverse effects including weight gain, osteoporosis, diabetics, etc.. Thus, phenotyping of bronchial asthma carries great importance.
Case Report
We describe an 18-year-old female who was an asthmatic since childhood which was fairly controlled till 17 years of age. she had frequent exacerbations requiring emergency care andfive hospitalizations in a period of 3 months of which two of those with respiratory failure despite being on oral corticosteroids and optimal inhaler therapy after checking the adherence and compliance.
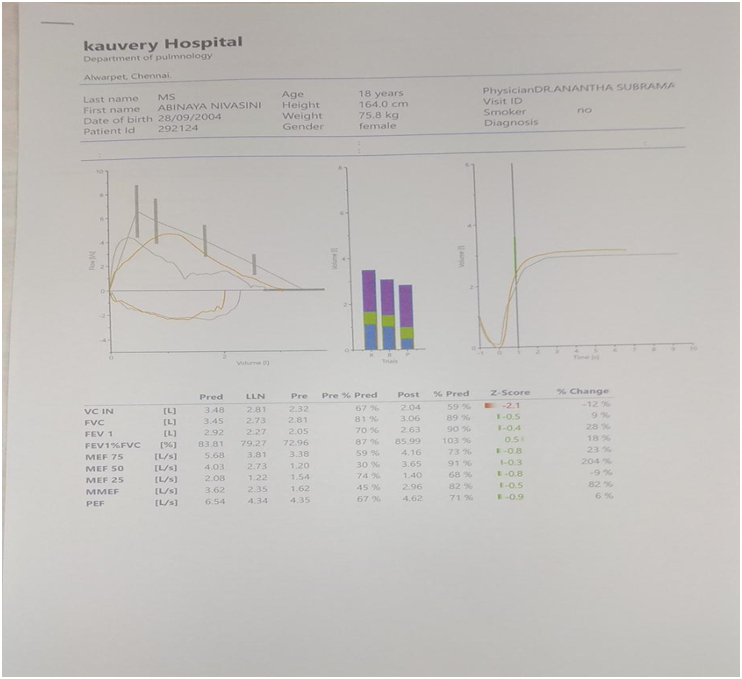
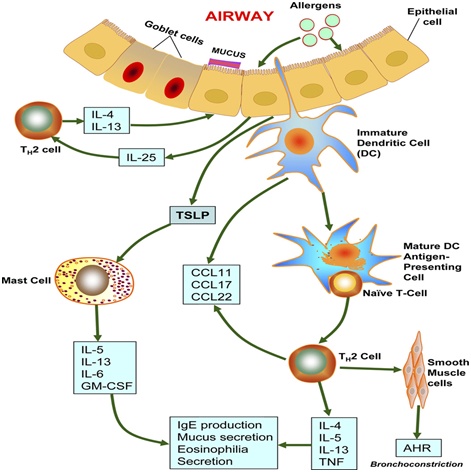
She was on medium dose ICS and LABA inhalation prior to the first exacerbation. Her treatment needed escalation to high dose ICS with LABA, LAMA and reliever medications with salbutamol and ipratropium bromide daily along with oral corticosteroids as she continued to have recurrent exacerbations for3 months. The predicted fev1 value was 70% (2.05lt) fig 1. She was being evaluated for severe uncontrolled asthma during her exacerbation free periods. CAT scan of the chest and para nasal sinuses were normal. Her serum Immunoglobulin E (IgE) was greater than 700 UI/mL and FeNO was 111ppb (cut off <25ppb) fig 2. Her peripheral eosinophil counts were low and not measurable. Connective tissue disease (CTD), vasculitis and allergic bronchopulmonary aspergillosis (ABPA) work up was negative. She was diagnosed with T2 high asthma. She was desensitized to strong positive allergens on SPT (skin prick test) with SLIT (sub lingual immunotherapy).
As her symptoms persisted with exacerbations, the choice of biologics was considered. She was initially treated with Omalizumab (Anti IgE) 300mg twice weekly for 3 months duration. She had no significant improvement and continued to have mild to moderate exacerbations requiring emergency care. Owing to continued exacerbations, omalizumab was discontinued and benralizumab (Anti IL5Rα) was initiated. After completion of 2 doses during her subsequent OPD visits there was significant amelioration of respiratory symptoms. Her AQLI and pulmonary function test improved. Oral corticosteroids were gradually tapered and stopped. She had completed 4 doses of inj Benralizumab 30mg SC and no adverse events have been reported. The dose of ICS also has been reduced gradually over a period of 2 months and stopped. Repeat spirometry predicted fev1 value was 80% and FeNO was 95ppb. She had no asthma exacerbations since starting Benralizumab treatment.
Discussion
This case report highlights the importance of biologics in bronchial asthma management. Biologics are used to treat T2 inflammation related asthma. Thus, phenotyping and Endo typing is needed for asthma patients to initiate optimal medical therapy and to decide on the biological agent suitable for severe uncontrolled asthmatics.
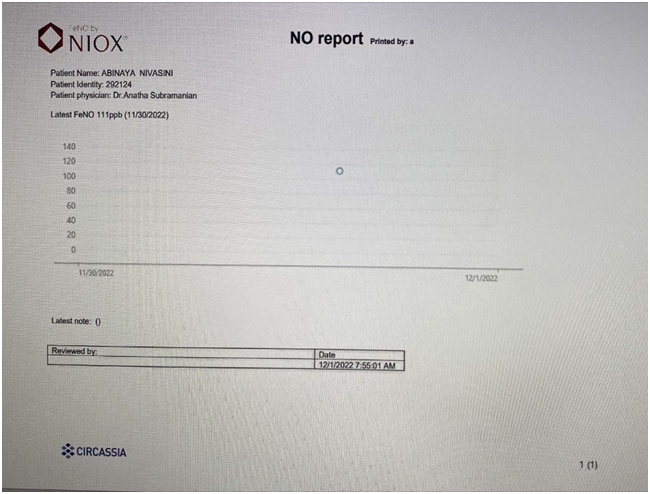
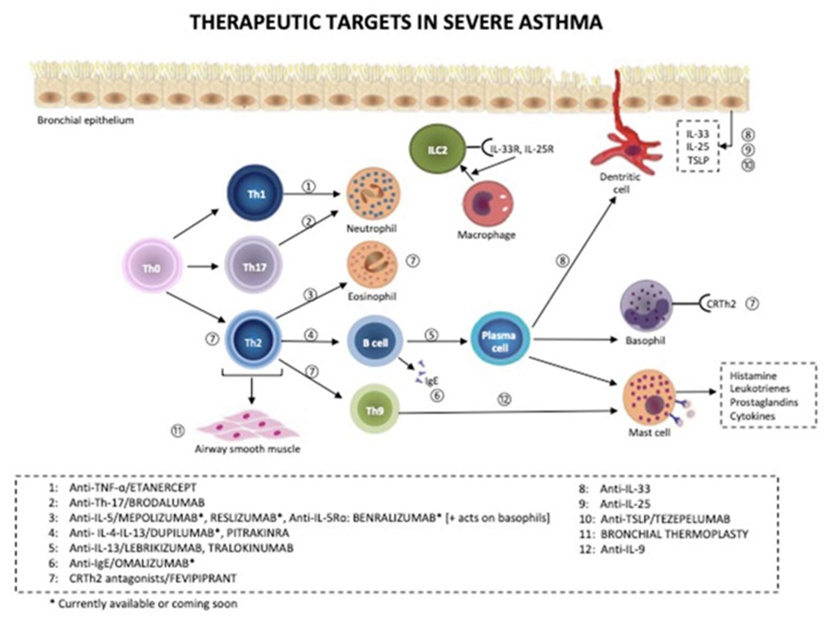
The different etio-pathological mechanisms involving the various phenotypes and endotypes of asthma led to the development of newer therapies. The biologics currently available in India are omalizumab (anti IgE), mepolizumab (anti IL5) and benralizumab (anti IL5R). The other agents commonly used are dupilumab (anti IL 4 and anti-IL 13), reslizumab(anti IL 5) and Tezepelumabwhich targets the thymic stromal lymphopoietin (TSLP)Fig 3. These monoclonal antibodies (mAB) are used according to the specific biomarkers identified. These MABs target the molecules involved in type 2 inflammatory pathway and thereby helps in decreasing the airway inflammation, thus reducing the need for systemic corticosteroid therapy.
This patient had both allergic and eosinophilic predominant uncontrolled asthma which is an overlapping phenotype. Omalizumab acts by lowering the blood IgE levels and peripheral eosinophilia. Since there was a poor response to omalizumab this patient was switched to benralizumab though she had lower peripheral blood eosinophilia which was not measurable due to steroid usage. FENOhas been found to be associated with the pathwaysof IL4, IL13 and can be used as surrogate marker for eosinophilic airway inflammation2,3. The major cytokine responsible for eosinophilic pathophysiology is IL54.the gold standard method for diagnosing eosinophilic asthma requires sputum phenotyping which is done only by limited centres. mABs targeting IL4 and IL13 (Dupilumab) are not available in India. Hence the decision was made to start on benralizumab. This targeted therapyapproved in 2017 directed against IL5Rα induces eosinophil apoptosis via the antibody-dependent cell-mediated cytotoxicity (ADCC) involving natural killer cells, leading to peripheral blood eosinophil depletion5. It is used in step 4/5 Gina treatment guidelines for asthma for adults above 18years of age with peripheral eosinophil counts of >300/µl.
Conclusion
There are novel therapies and convincing evidence to prove the management of asthma beyond inhaled and oral medications especially steroids which is a commonly prescribed for asthma that can have deleterious effects on patients in countries like India where the risk of multi drug resistant infections is alarming and the other morbidities associated with it.
This case report showed the benefits of Benralizumab on severe uncontrolled asthma and its use based on FENO indicating the use of this mABin the absence of peripheral blood eosinophilia. Also, its use in acute exacerbations requiring ICU care is being studied and has shown promising benefits. As more evidence emerges on the pathophysiology of asthma, newer targeted therapies are being studied for precision-based medicine especially for chronic diseases like asthma (fig 4).
References
- Wenzel S. Severe Asthma in Adults. Am J Respir Crit Care Med. 2005; 172; 149–60
- Price DB, Buhl R, Chan A, Freeman D, Gardener E, Godley C, et al. Fractional exhaled nitric oxide as a predictor of response to inhaled corticosteroids in patients with non-specific respiratory symptoms and insignificant bronchodilator reversibility: a randomised controlled trial. Lancet Respir Med. 2018; 6:29–39
- Increasing utility of FeNO as a biomarker of type-2 inflammation in severe asthma Kian Fan Chung Published:June 25, 2021DOI:https://doi.org/10.1016/S2213-2600(21)00170-3
- IL-5 and IL-5 receptor in asthma.Kotsimbos AT, Hamid Q. Mem Inst Oswaldo Cruz. 1997;92 Suppl 2:75-91. doi: 10.1590/s0074-02761997000800012. PMID: 9698919
- FitzGerald JM, Bleecker ER, Nair P, Korn S, Ohta K, Lommatzsch M, et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–41
Figures.
1.
2.
3.
4.
 Dr. Anantha Subramanian
Dr. Anantha Subramanian
Consultant Pulmonologist
Kauvery Hospital Chennai