Spirometry is used widely by physicians and pulmonologists worldwide to aid in the diagnosis of lung diseases as well as in assessing the disease severity. However, it requires the patients to be cooperative and perform forced respiratory maneuvers which might not be possible in all patients. Examples of such scenarios include children, elderly people and patients with dementia or altered mental status. Spirometry might not be abnormal in patients with very early lung disease. Also, spirometry is contraindicated in certain conditions. These include 3rd trimester pregnancy, recent myocardial infarction within 1 month, recent thoracic or abdominal surgery (within previous 6 weeks), recent eye or ear surgery (within previous 6 weeks), active hemoptysis and thoracic, abdominal or cerebral aneurysms.(1)
FOT is Forced oscillation technique which was first described by Dubois et al in 1956. In this technique, sound waves of varying frequencies are passed into the lungs one after the other during tidal breathing. The output from the lungs is measured as Impedance (Zrs) which is a combined output of Resistance (Rrs) and Reactance (Xrs). Reactance has 2 components. Inertance (I) and capacitance(C). A graph is plotted keeping frequencies in the X axis and Resistance and reactance in Y axis. Other parameters that can be inferred from the graph include Ax(Reactance area) and Fres (Resonant frequency). These parameters provide valuable information about the mechanics of airways and lung parenchyma. Resistance is not frequency dependent in adults, however reactance is frequency dependent with capacitance component dominating in lower frequencies and iterance component dominating in higher frequencies. A slight improvisation of this technique is called IOS(Impulse oscillometry system) where multiple sound frequencies are passed at one time.(2)
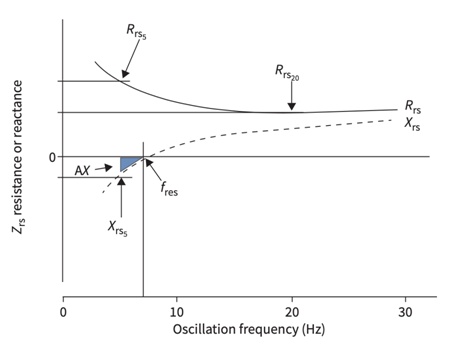
Zrs – Impedance I – Inertance fres – Resonant frequency
Rrs – Resistance C-Capacitance
Xrs – Reactance AX-Reactance area
The above graph shows normal FOT graph
Normal fres value in adults in less than 8-12Hz. Values above 12Hz are abnormal(3, 4)
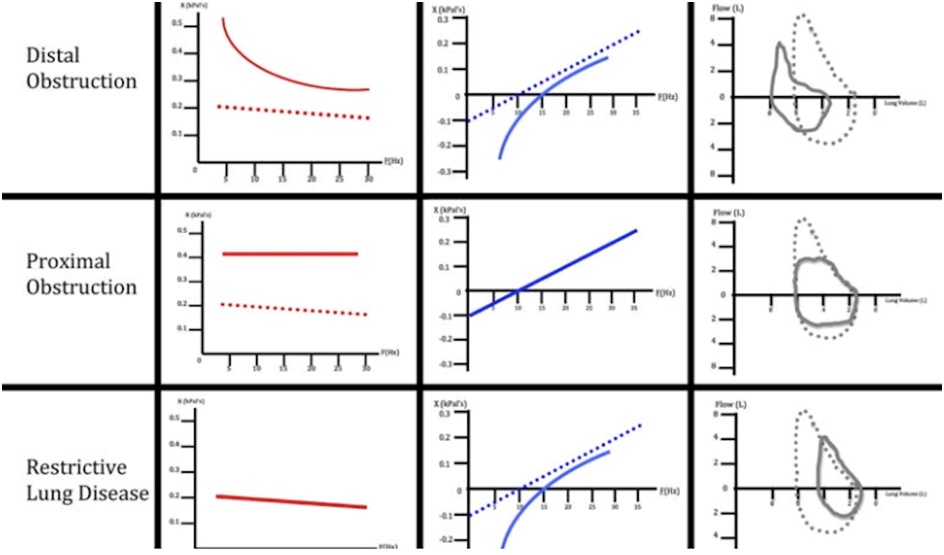
The above graphs show FOT interpretation of obstructive and restrictive lung diseases.(5)
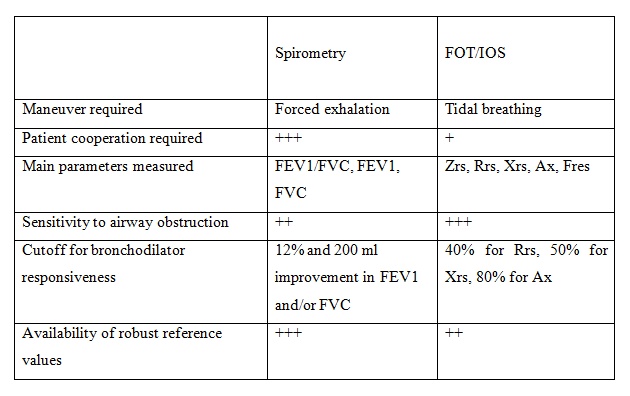
FOT/IOS requires the patient to perform simple tidal breathing maneuvers and hence can be performed in patients who have contraindications for spirometry and in those not suitable for spirometry. Also, FOT is more sensitive than spirometry in diagnosing lung diseases and hence can be performed in those patients who have normal spirometry but high clinical suspicion of lung diseases especially small airway diseases.
Differences between spirometry and FOT/IOS
Let us go through few cases where using FOT has helped us in the management of respiratory symptoms
Case 1
A 25-year-old pregnant female who is in her 3rd trimester of gestation gets admitted in the hospital with persistent dry cough and MMRC grade 1 dyspnea since 1 month. She had no history of fever, expectoration, loss of appetite or weight. She denied any history of atopy however her mother had history of allergy to dust. Her clinical examination of the ENT and respiratory system was normal. Her chest x ray taken with lead shielding was normal. She was initially managed with antitussives and proton pump inhibitors. However, her symptoms persisted. Spirometry was contraindicated and hence she was subjected to FOT which revealed small airway disease with significant improvement on bronchodilator testing as shown in Figures 1A and 1B. She was initiated on inhalers containing formoterol fumarate plus beclomethasone dipropionate. Her symptoms resolved and she was discharged. She later delivered a full term healthy baby by normal vaginal delivery without any complications.
Final diagnosis: Small airway disease phenotype of bronchial asthma
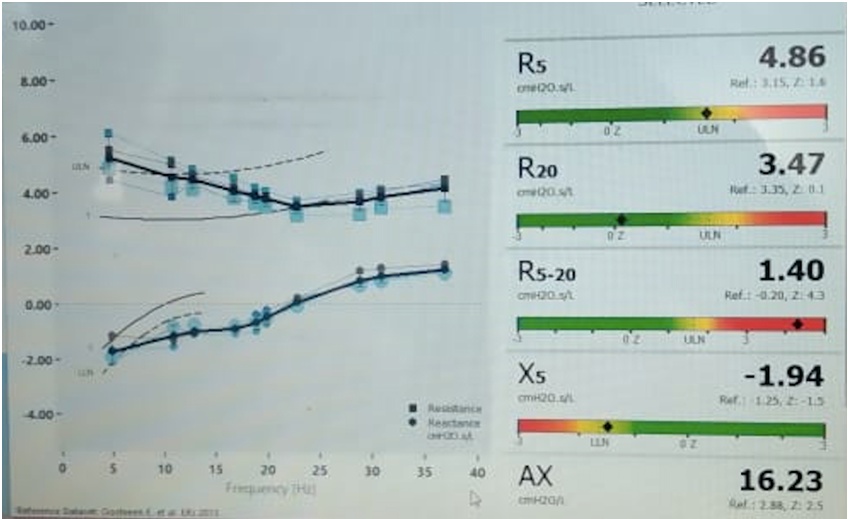
Figure 1A. The above FOT graph typically depicts small airway disease in case 1
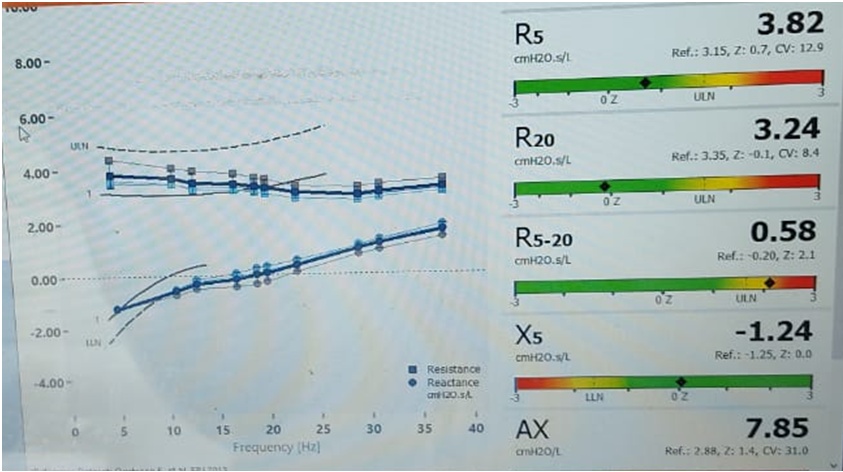
Figure 1B. The above FOT graph of case 1 after bronchodilator usage shows significant improvement in R5, X5 and Ax
Case 2
A 33-year-old female patient presented with complaints of intermittent episodes of dry cough, breathlessness and hyperventilation since 5 years. Her symptoms appeared only while performing household work. She denied any history of allergy and no history of similar complaints in the family. She was evaluated at other centers with chest x ray, ECG, complete blood count, renal function test, liver function test, CT chest, spirometry and 2D Echo. All her investigations were within normal limits. She was managed as a case of anxiety disorder and was put on anti-anxiety medications. However, she continued to have similar episodes. Hence, she came to our center. Her clinical evaluation was normal and her blood investigations revealed no peripheral eosinophilia. Spirometry was repeated at our center with bronchodilator responsiveness testing which was normal. FOT was performed and it revealed small airway disease with significant improvement using bronchodilator as shown in Figure 2. She was put on inhalers containing formoterol fumarate plus beclomethasone dipropionate. Her symptoms resolved and her anti-anxiety medications were stopped.
Final diagnosis: Small airway disease phenotype of bronchial asthma
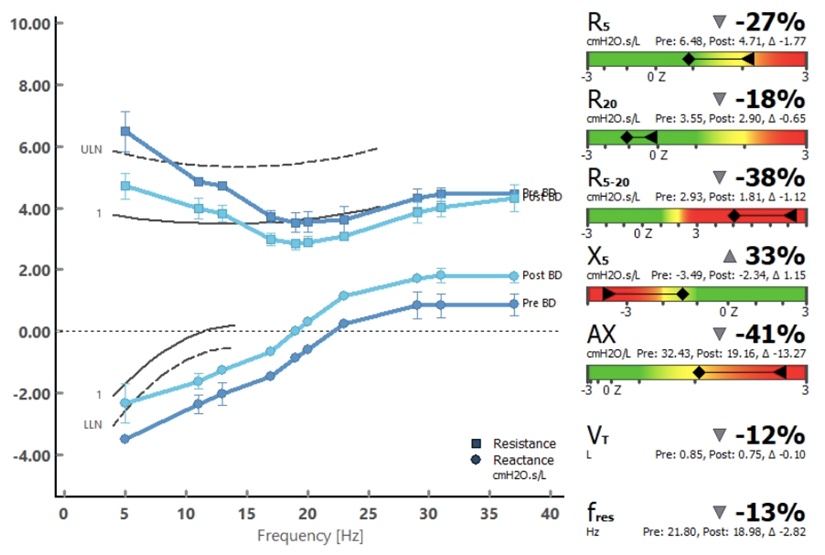
Figure 2 shows FOT graph in case 2 which shows small airway disease with significant improvement using bronchodilator
Case 3
A 65-year-old female patient got admitted in ICU with type 2 respiratory failure. She gave history suggestive of obstructive sleep apnea but was never evaluated or treated. She was obese with a BMI of 32kg/m2. On clinical evaluation she was tachypneic with a respiratory rate of 30 and her chest auscultation was normal. Her NT-proBNP, 2D Echo and D-dimer were normal. Her CT chest showed mosaic attenuation. She was managed with NIV and bronchodilators. Her clinical condition and Type 2 Respiratory failure improved. She was shifted to ward from ICU. She couldn’t perform spirometry however she was able to perform bedside FOT which showed small airway disease with significant improvement on bronchodilator testing as shown in Figure 3. She underwent polysomnography which also revealed severe sleep apnea with AHI 35. She underwent autoCPAP titration and her AHI reduced to 5. She was discharged on advice of nocturnal auto CPAP and bronchodilator.
Final diagnosis: OSA/Obstructive airway disease overlap
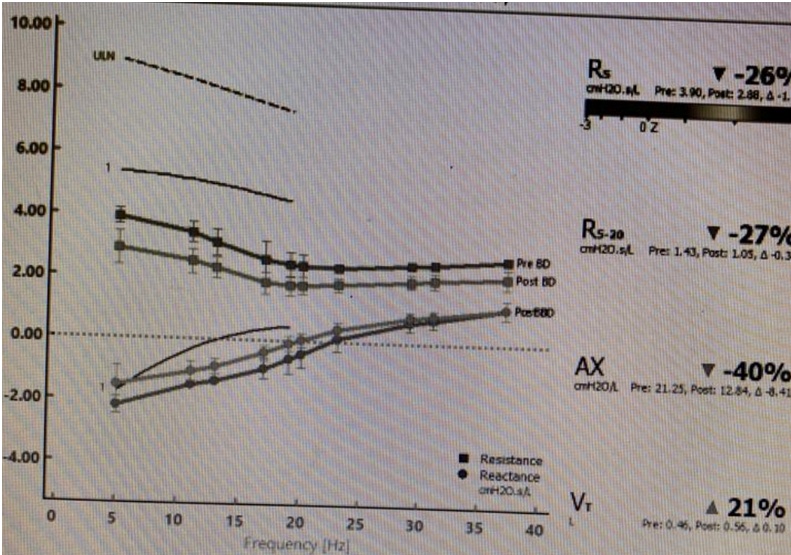
Figure 3 shows FOT graph in case 3 which shows small airway disease with significant improvement using bronchodilator
Other possible applications of FOT include following treatment response in asthma, predicting asthma exacerbations, performing bronchial challenge testing, screening for occupational lung diseases, screening for COPD in smokers, screening for airway obstruction in cystic fibrosis and screening for bronchiolitis obliterans after bone marrow and lung transplants
Summary
FOT/IOS is a new diagnostic technique in the field of pulmonology which has huge implications if used appropriately. However, further research is needed in establishing reference equations among various population groups
Reference
1. Aggarwal AN, Agarwal R, Dhooria S, Prasad KT, Sehgal IS, Muthu V, et al. Joint Indian Chest Society-National College of Chest Physicians (India) guidelines for spirometry. Lung India. 2019;36(Supplement):S1-s35.
2. Brashier B, Salvi S. Measuring lung function using sound waves: role of the forced oscillation technique and impulse oscillometry system. Breathe (Sheff). 2015;11(1):57-65.
3. Kaminsky DA, Simpson SJ, Berger KI, Calverley P, de Melo PL, Dandurand R, et al. Clinical significance and applications of oscillometry. Eur Respir Rev. 2022;31(163).
4. King GG, Bates J, Berger KI, Calverley P, de Melo PL, Dellacà RL, et al. Technical standards for respiratory oscillometry. Eur Respir J. 2020;55(2).
5. Komarow HD, Myles IA, Uzzaman A, Metcalfe DD. Impulse oscillometry in the evaluation of diseases of the airways in children. Ann Allergy Asthma Immunol. 2011;106(3):191-9.
 Dr. R. Nithiyanandan
Dr. R. Nithiyanandan
Associate Consultant Pulmonary and Critical Care
Kauvery Hospital Chennai