Brain metastases are the most frequently seen intracranial tumors in terms of patient incidence. Studies indicate that approximately 15% to even 30% of individuals diagnosed with malignancies ultimately develop metastatic lesions within the brain over the course of their illness. The most common primary tumours causing intracranial spread are lung, breast, melanoma, renal and colon cancers – in the order of frequency. Notably, around 70% of patients presenting with symptomatic brain metastases exhibit multiple lesions upon MRI examination. Fortunately, with the increasing accessibility of advanced imaging technologies in recent years, early detection has become more achievable.
Typically, metastatic lesions tend to localize within the brain parenchyma, particularly near the grey matter – white matter interface. The cerebral hemispheres are the most commonly affected regions, followed by the cerebellum.
The treatment methods available in managing brain metastasis are surgery, whole brain radiotherapy and stereotactic radio surgery. When considering a patient for surgery, multiple factors need to be taken into account. The most important one is the status of the primary and systemic disease and atleast 4 to 6 months of expected survival due to the same. Large lesions with mass effect need to be surgically excised in order to prevent rapid worsening of the clinical status of the patient.
Previously only solitary metastatic lesions were preferred for surgical excision. But due to the advancement in surgical techniques and decrease in the overall operative morbidity, even upto four intracranial lesions in accessible locations can now be removed safely.
Here we present a case of bilateral cerebral metastases which was successfully managed with complex team work involving radiation oncology, medical oncology and neurosurgery.
A 50 year old lady was diagnosed with carcinoma ovary, for which she underwent total abdominal hysterectomy, bilateral salpingo – oophorectomy and omentectomy in 2020. She received 8 cycles of post operative chemotherapy and treated with Olaparib for 1 year. While on regular follow up, PET CT showed multiple brain metastasis in cerebellum, right temporal and left high frontoparietal cortex. She received whole brain radiotherapy (27 Gy in 9 #) along with SRT boost (15 Gy in 3 #) in December 2021. Repeat PET CT in October 2022 showed significant regression of the disease and the cerebellar lesions were not visualised. Contrast MRI imaging in November 2023 showed enhancing lesions in the left high frontoparietal cortex and right temporal lobe with mass effect and midline shift to the left.
PET CT showed no active disease elsewhere in the body.
The patient was well preserved with no gross neurological deficits.
Considering the above scenario, the decision to remove both the lesions, one on each cerebral hemisphere was made.
During the surgery, the patient’s preoperative contrast MRI was loaded in the neuronavigation system and the surgical incisions were planned accordingly. Small tailored craniotomies were made on each side with just enough dimensions to expose the tumour.
The left sided high frontal lesion was immediately adjacent to the motor cortex. Large veins were seen draining from the eloquent motor strip traversing close to the lesion. Post operative weakness is very common in such lesions. To prevent neurological deficits, different modalities were used during the surgery. Tumour fluorescence is one useful adjunct tool especially in high grade brain tumours. Sodium fluorescein was injected intravenously into the patient and special filters were used in the operating microscope to delineate the tumour tissue from the surrounding eloquent cortex. Indocyanine green intraoperative angiography was used to visualise the drainage veins and their relationship with the motor cortex veins which were then meticulously dissected off from the tumour.
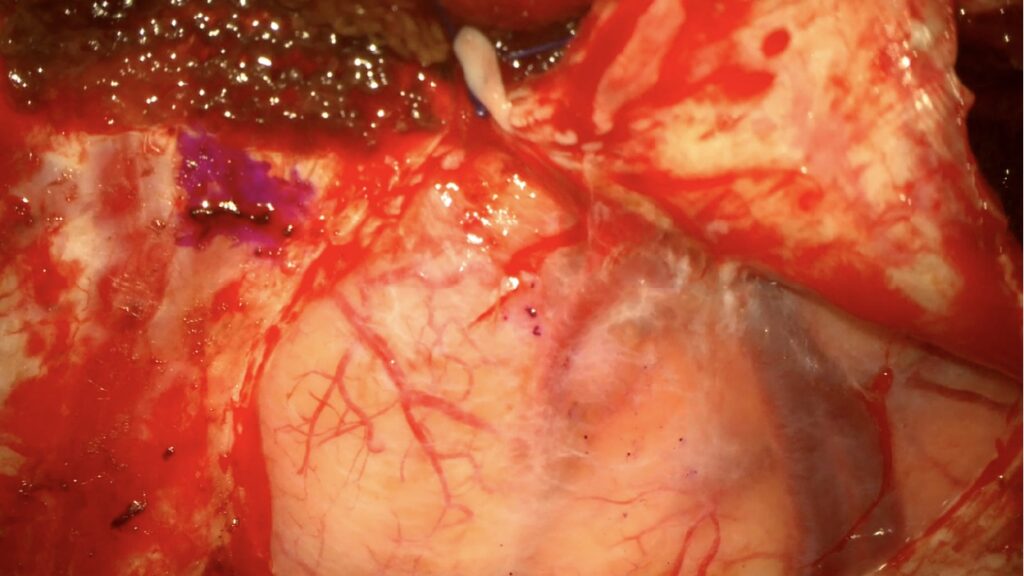
Intraoperative picture of the left high frontal tumour lying just anterior to the motor cortex and its draining veins.
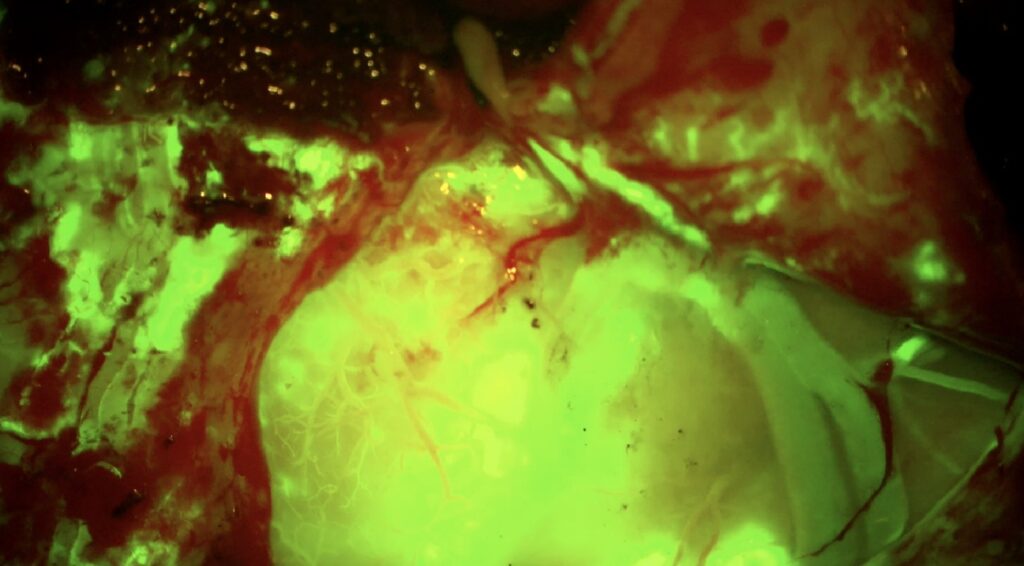
Intraoperative tumour fluorescence after administering sodium fluorescein
The right sided temporal lesion was also removed in a similar manner.
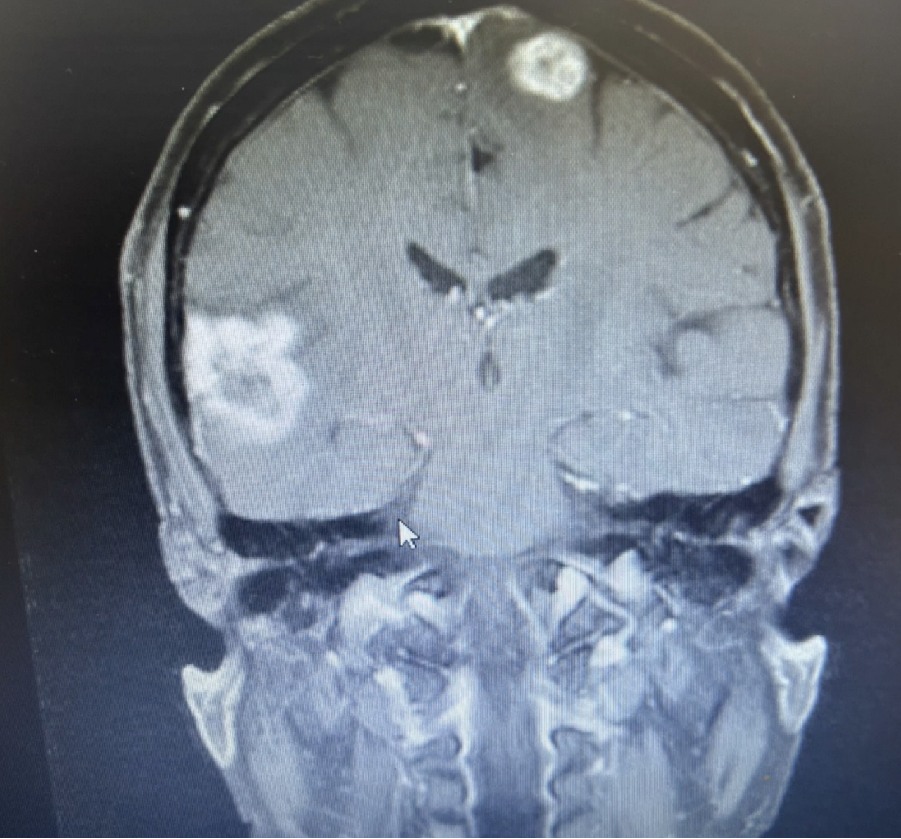
Preoperative MRI showing contrast enhancing lesions in the left high frontal region and right temporal region.
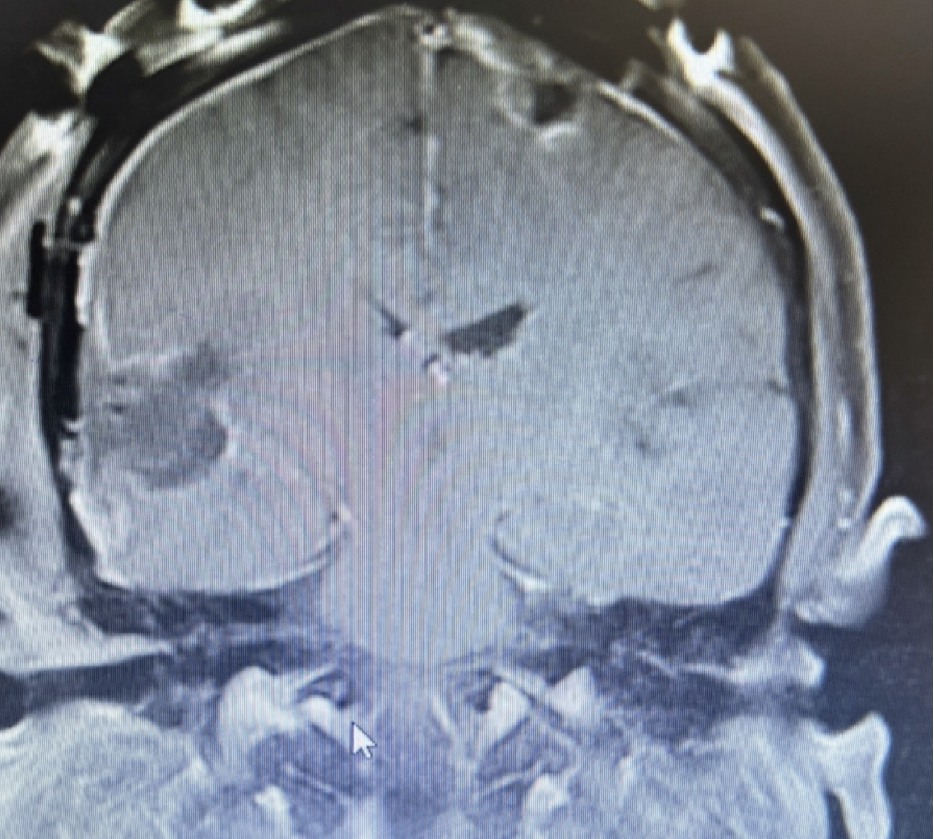
Post operative MRI showing gross total excision of both the metastatic lesions
Post operative MRI showed gross total excision of both the lesions. The patient recovered well without any neurological deficits and was discharged.
After surgical wound healing, she received SRT boost of 18 Gy.
CONCLUSION:
Management of multiple brain metastasis has to be customised according to each patient taking into consideration the general condition of the patient, objectively assessed using the Karnofsky performance scale, the status of the primary and the systemic disease. Tumours in deep location especially in the brainstem, thalamus and basal ganglia are not amenable to surgery. Large lesions more than 3 cms with surrounding mass effect and midline shift need to be surgically removed in order to provide immediate clinical improvement in the patient.
With the advent of neuronavigation which is essentially a computer assisted – stereotactic image guided surgery and advances in operative microneurosurgical techniques, it is possible to remove multiple brain metastasis without surgical morbidity and post operative neurological deficits. Surgical tumour removal followed by post operative radiotherapy provides better survival in indicated patients.


 Dr. J. Balaji
Dr. J. Balaji Dr. A. N. Vaidhyswaran
Dr. A. N. Vaidhyswaran Dr. A. N. Aswin
Dr. A. N. Aswin
