A 45-year-old female with a history of fever, sepsis and acute kidney injury, presented to our radiology department with acute abdominal pain and distension. A MDCT abdominal angiogram with oral Gastrograffin scan was performed, revealing multiple segments of non-enhancing, severely thinned out small bowel walls and foci of intramural gas pockets with intervening normal enhancing segments in the right lower abdomen involving the ileal loops. Of significant concern was the absence of vasa recta adjacent to the ischemic bowel wall, highlighting the ischemic nature of the findings.

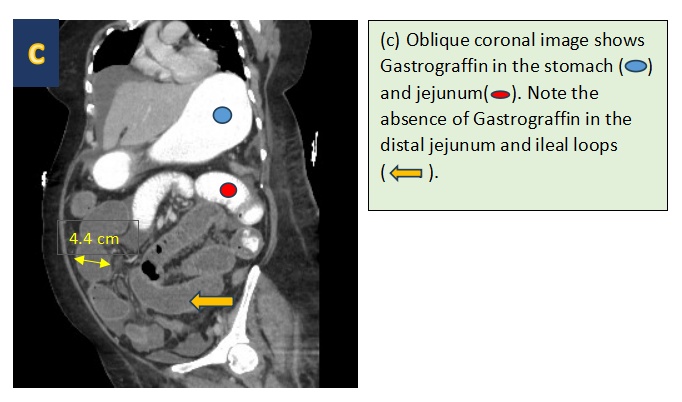
Additionally, dilated and fluid-filled small bowel loops, without a clear transition point, were observed, with the maximum diameter reaching 4.4 cm. Gastrograffin administered during the study did not progress beyond the proximal jejunum, indicating an adynamic ileus. Mild ascites was also noted.
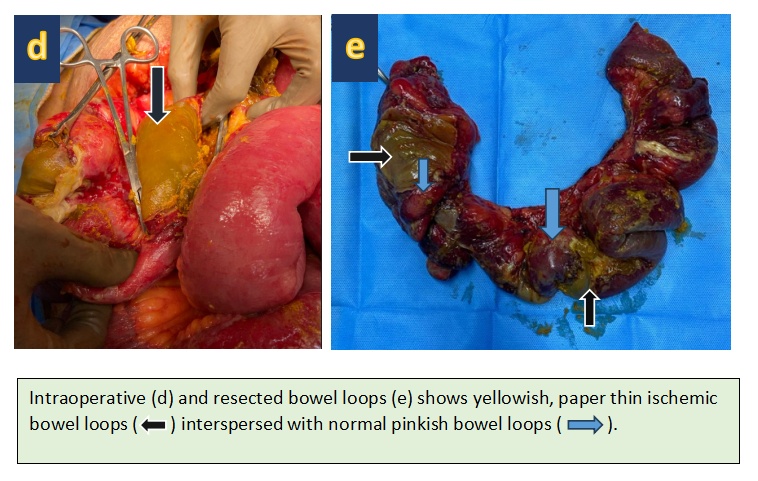
The intraoperative and post-surgical resected small bowel confirmed the diagnosis, showing yellowish, paper-thin ischemic small bowel with interspersed normal bowel loops.
Discussion:
Bowel ischemia is a serious medical condition that occurs when there is insufficient blood flow to the intestines. This can lead to tissue damage and even death if not treated promptly. Radiology plays a critical role in the diagnosis and management of bowel ischemia. In this article, we will discuss the CT findings of bowel ischemia.
The pathophysiology of bowel ischemia is complex and can be caused by various factors, including arterial or venous occlusion, non-occlusive mesenteric ischemia, and bowel obstruction. The clinical presentation of bowel ischemia is often nonspecific, making imaging studies essential for accurate diagnosis.
CT is the primary imaging modality for the evaluation of suspected bowel ischemia. CT findings of bowel ischemia include bowel wall thickening, poor or absent enhancement, luminal dilatation, and pneumatosis intestinalis. These findings can be seen in both small and large bowel ischemia. In addition, CT can also identify alternative causes of acute abdominal pain, such as appendicitis or diverticulitis.
In patients with arterial bowel ischemia, the involved bowel wall may be thin, with a paper-thin appearance attributable to a loss in the volume of the bowel wall. This finding is highly specific for arterial bowel ischemia. Venous bowel ischemia, on the other hand, may present with vascular engorgement and oedema of the bowel wall, leading to extravascular fluid leakage into the bowel wall and mesentery. Mesenteric oedema and extravascular fluid tend to be seen more often in venous than in arterial ischemia.
Bowel ischemia due to bowel obstruction is another common cause of bowel ischemia. In patients with small bowel obstruction, 10% develop bowel ischemia because the segment of the tract proximal to the obstruction site is dilated and filled with fluid. The luminal pressure increases, exceeding first the venous flow and then the arterial flow, resulting in bowel ischemia. CT scanning and reconstruction protocol for bowel ischemia are essential for accurate diagnosis and management.
In conclusion, CT is the primary imaging modality for the evaluation of suspected bowel ischemia. CT findings of bowel ischemia include bowel wall thickening, poor or absent enhancement, luminal dilatation, and pneumatosis intestinalis. Understanding the underlying pathophysiology and CT findings of bowel ischemia is essential for accurate diagnosis and management. Radiologists play a critical role in the diagnosis and management of bowel ischemia, and a high index of suspicion is required for accurate diagnosis.
Special thanks to the ICU and Liver team for clinical follow-up and intraoperative images.
 Dr. Sathya Narayanan R
Dr. Sathya Narayanan R
Consultant Diagnostic and Interventional Radiology
Kauvery Hospital, Chennai
 Dr. Kanagasabai Kamalasekar
Dr. Kanagasabai Kamalasekar
Consultant Radiology
Kauvery Hospital, Chennai
 Dr. Murali
Dr. Murali
Post Graduate Resident – Radiology
Kauvery Hospital, Chennai