Introduction:
Despite the fact that there is a greater demand for organs than there are available for transplant, the responsibility to take care of potential donors increases. The main limiting factor is the availability of suitable donors and organs in organ donation. A multidisciplinary team approach is essential for successful organ donation. Donor organs should be normalized and maintained till the time of organ retrieval. Especially older people and marginal donors are also potential donor candidates, such cases need to be managed carefully, to improve the conversion rate and graft survival after donation. Intensivists play a vital role in the identification, declaration of brain death, and improving rates of graft survival by providing optimal care to potential organ donors.
Multisystem Management of Multi-organ Donor
1) Management of Hemodynamics:
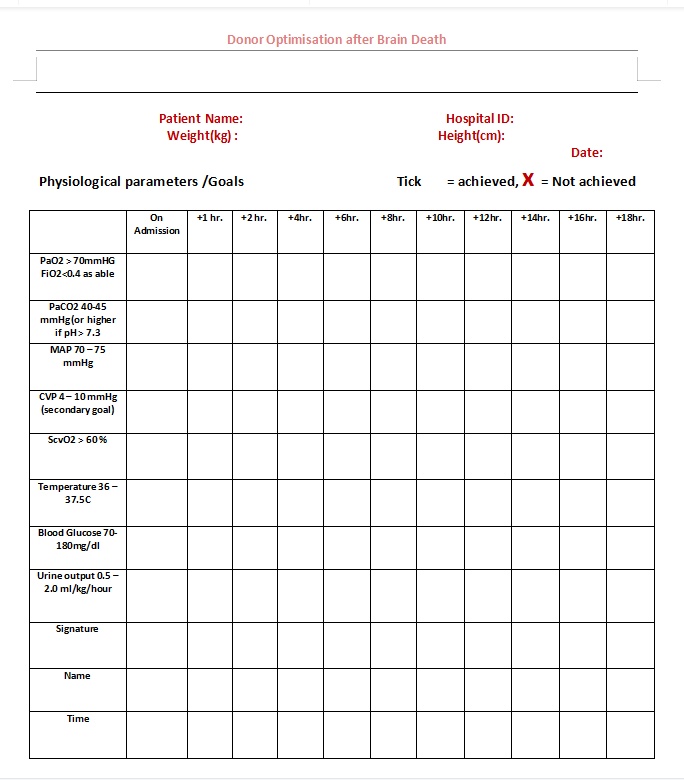
Hemodynamic instability, like large fluctuations in hemodynamics from sympathetic storm to vasoplegic state, is very common in brain-dead donors. The predominant goals of hemodynamic management are to maintain volume status and blood pressure within a normal-range.
To optimize cardiac output to maintain perfusion pressure of all organs, review intravascular fluid status, and correct hypovolemia with fluid boluses. Commence vasopressin (2.4 units/hour) where vasopressor is required, wean, or stop catecholamine pressors as able. Intravenous fluids and inotropes/vasopressors (dopamine, dobutamine, epinephrine, vasopressin, and norepinephrine) should be administered based on hemodynamic variables and also with guidance of bedside point-of-care ultrasonography.
2) Respiratory management:
Basic respiratory support in intensive care like Maintain 30-45 degrees head of bed elevation and ensure cuff of endotracheal tube is appropriately inflated to prevent aspiration. Patient position change (side, back, side) as per unit protocol. Maintain regular chest physiotherapy including suctioning as per unit protocol. Review ventilation, ensure lung protective strategy (Tidal volumes 4 – _8ml/kg ideal body weight and optimum PEEP (5 – _10 cm H2O). Where available, and in the context of lung donation, perform bronchoscopy, bronchial lavage.
3) Management of hormonal and metabolic derangement:
Administer maintenance fluids (or NG water where appropriate) and review fluid administration every 2 hours to avoid positive fluid balance and to maintain Na+ < 150 mmol/L. Maintain urine output between 0.5 –2.0 ml/kg/hour. If > 4 ml/kg/hr, consider Diabetes insipidus and treat promptly with desmopressin nasal spray (1 puff per nostril every 4 hours) or vasopressin (1–4 IU/hour) with frequent monitoring of sodium.
Administer methylprednisolone (dose 15 mg/kg, max 1 g) to moderate the inflammatory response, which is common in brain-dead donors. Increased organ retrieval is associated with methylprednisolone use and should be administered immediately. The other component of hormonal replacement is a thyroid supplement. However, there is no strong evidence for thyroid hormone replacement, and intravenous T3 is generally unavailable in India. So, T4 oral 300–400 mcg/8 hourly is suggested instead of T3. Always maintain normoglycemia. Consider an insulin infusion to keep blood sugar at 70–180 mg/dl.
4) Blood and Coagulation:
To avoid thrombotic complications, low-molecular-weight heparin or sequential compression devices are recommended. On the other hand, in case of active bleeding cause of the bleeding should be identified immediately and correct the coagulation if there is any coagulopathy. Transfusion of blood and blood products should be done only if necessary.
5) Lines, Monitoring, and Investigations (if not already done):
Insert arterial line preferably left radial for continuous blood pressure monitoring. Place Central vein catheter preferably right side (int jugular or subclavian) to administer fluids and vasopressor. Maintain normothermia using active warming where required. Perform basic investigations like a 12-lead ECG, CXR (post intubation, CVC lines procedure where possible). Send Troponin level in all cardiac arrest cases (and follow-up sample where patient in ICU > 24 hours). Where available, perform an Echocardiogram. Review and stop all unnecessary medications. Continue hourly observations as per critical care policy.
Conclusion
Brain stem death is commonly followed by a predictable pattern of multiple organ failure. we can improve the number and quality of donor organs by providing the appropriate support before and after brain death. Brain-dead organ donor support is intensive and time-consuming which Increases the number of marginal donors who are now being accepted as potential donors.

Dr Vetriselvan, MD, DM
Consultant Critical Care
Kauvery Hospital Chennai



