Abstract
Hemophagocytic lymphohistiocytosis (HLH) is an aggressive and life-threatening syndrome of excessive immune activation. It most frequently affects infants from birth to 18 months of age, but the disease is also observed in children and adults of all ages. HLH can be classified into primary and secondary HLH. The highest incidence in those <3 months. The male-to-female ratio is close to 1:1. In adults, there may be a slight male predisposition.
Case report
19 years female, with no comorbids and no known drug allergy, presented to ER from outside hospital with
– H/O fever – low grade, intermittent for initial 3 days following which high grade, intermittent for last 4 days.
– H/O vomiting * 3 days – non bilious. Non projectile, non blood stained.
– H/O shortness of breath * 2 days.
– H/O rashes over both upper limbs * 2 days with bruising over IV cannulation sites.
Menstural history: irregular cycles, LMP= 2 months ago, spotting P/V noted 2 days back.
On initial evaluation at ER
Airway
Patent, self-maintained.
Breathing
RR – 26/ min, Spo2 – 99% RA, B/L air entry equall and absent in basal zones bilaterally, no added breath sounds.
Ciculation
BP – 140/ 70 mmHg. HR – 138/ min,
CVS -Tachycardic, S1S2 normal, no murmur, JVP – Normal,
PA – Soft, non-tender, no organomegally, bowel sounds heard.
Disability
GCS – E4V5M6 [15/ 15]
Moving all 4 limbs
CBG – 121mg/dl
Exposure
Temp: 103o F
Few bruises notes at IV line sites, few petechial rashes over bilateral upper limbs.
VBG
pH – 7.32
PCO2 – 37 mmHg
PO2 – 16 mmHg
BE -7 mmol/ L
HCO3 – 19.3 mmol/ L
LAC – 1.78 mmol/ L
Investigations
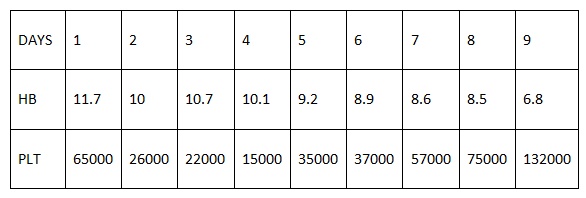
⦁ Complete blood count suggestive of pancytopenia with marked reticulocyte count and deranged liver function.
⦁ Peripheral smear suggestive of normocytic, normochromic anemia with thrombocytopenia (done outside). In our hospital microcytic, hypochromic anemia with thrombocytopenia.
⦁ CRP: 200, LDH: 1688, Ferritin: 15,306, Procalcitonin: 0.90, Trop-I : 0.002, NTproBNP: 531.TGL: 425
⦁ Dengue NS-1: Negative, IgM: negative, IgG: positive, MP-QBC: negative, Scrub typhus IgM: negative.
⦁ Salmonella Typhi O & H positive in 1:320 dilution. Salmonella Para Typhi A&B negative in 1:20 dilution
⦁ ANA/ Anti HAV-IgM/ HEV-IgM/ Anti HBc IgM : non-reactive
⦁ EBv Abs to viral capsid Ag (VCA) IgG/ EBV(NA) IgG antibody: negative
⦁ SARS COV2 IgG antibody: positive
⦁ Echo: normal, Ultrasound abdomen: normal, Coombs test (direct) : negative.
⦁ Blood culture: Proteus species growth present, Urine routine pus cells present.
⦁ Suggested bone marrow biopsy (not done).
Discussion:
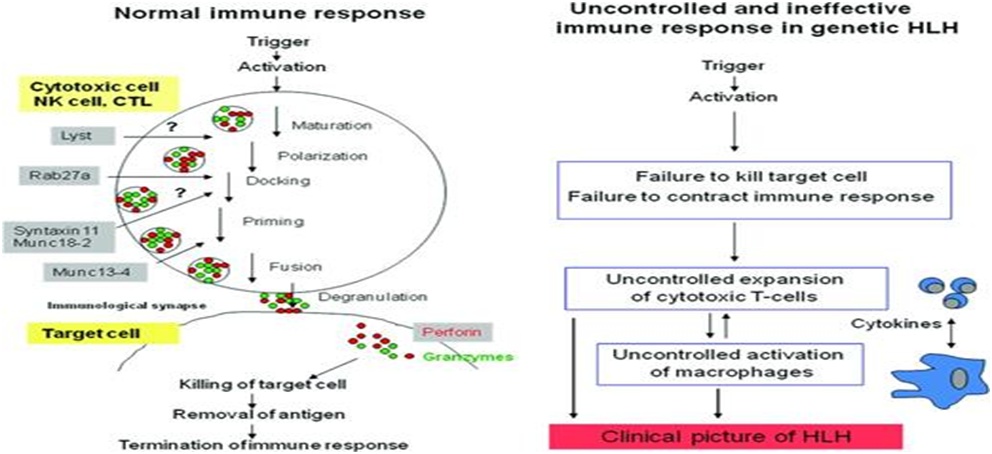
Hemophagocytosis is the engulfment of hematopoietic cells by activated macrophages acting outside of usual immune system regulations. Hemophagocytic lymphohistiocytosis (HLH) covers a wide array of related diseases including HLH, autosomal recessive familial HLH (FHL), familial erythrophagocytic lymphohistiocytosis, viral-associated hemophagocytic syndrome, and autoimmune-associated macrophage activation syndrome (MAS). These disorders feature severe cytopenias due to this uncontrolled hemophagocytosis. Other laboratory signs and clinical symptoms result from disordered immune regulation and cytokine storm. The term primary HLH refers to an underlying genetic abnormality causing the disorder, whereas secondary HLH indicates that the disorder is secondary to underlying conditions such as infection, autoimmune/rheumatologic, malignant, or metabolic conditions. For the purposes of this review, FHL will indicate cases with a primary genetic cause, secondary HLH will refer to cases secondary to infection, malignancy, or metabolic disorders, and MAS will refer to cases associated with autoimmune diseases. Primary HLH consists of monogenic disorders that mainly affect the perforin-mediated cytotoxicity of cytotoxic T lymphocytes and natural killer cells. Secondary HLH occurs as a complication in various settings such as infection, malignancy, autoimmune disease, and post-allogeneic hematopoietic stem cell transplantation. Both primary and secondary HLH are characterized by uncontrolled hypercytokinemia that results in myelosuppression and vascular endothelium damage.
It is estimated that approximately 1 child in 3000 admitted to a tertiary care pediatric hospital will have HLH, which corresponds to several cases per centre per year. Earlier reviews reported much lower rates of incidence, likely reflecting under diagnosis of the condition. As an example, in a series from the 1970s that reported an incidence of 1.2 children per million per year, the diagnosis of HLH was made antemortem in only 11 of 32 patients.
HLH carries a high acute mortality of around 40% for all groups combined. Malignancy associated HLH has a particularly poor prognosis with acute mortality exceeding 80% and 5-year survival of less than 15%. In ICU patients, the published hospital mortality rates range from 52%7 to 68%. The presence of shock or severe thrombocytopenia indicate increased risk. The maximum serum ferritin elevation concentration is directly correlated with an increased mortality risk, while a rapid fall in serum ferritin levels in response to treatment is associated with a more favourable short-term outcome.
There is large overlap between the definitions for HLH and sepsis. Both conditions share similarities in their pathophysiology, cytokine profile and clinical features. It has to be noted that sepsis may demonstrate a variety of immunological phenotypes, from a predominant inflammatory response to suppressed immune function or a combination of both, and this may be subject to evolution over time. Macrophage activation-like syndrome (MALS) was defined by a modified HScore, HPB and DIC or a combination of these, and was associated with a significant rise in early mortality. This further supports the existence of HLH secondary to bacterial infection, although its true prevalence remains imprecise.
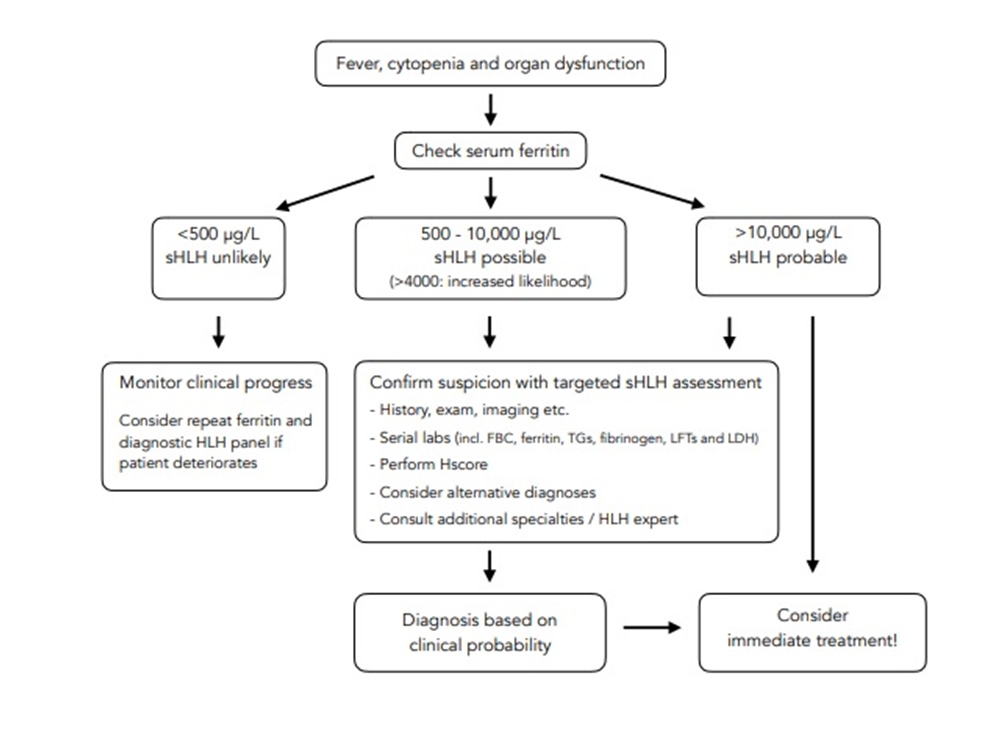
Differentiating HLH from sepsis may be difficult. HLH may be present in the absence of infection but cause an identical clinical presentation to septic shock (sepsis mimic). In addition, HLH can be triggered by infection or predispose to sepsis by virtue of its inherent immune dysfunction. Both conditions can co-exist in the context of an underlying disease such as malignancy or an autoimmune condition. HLH should, be suspected in all critically ill patients with unexplained fever, cytopenias and organ dysfunction, particularly those not responding to aggressive sepsis treatment.
Pathophysiology:
Diagnosis and criteria:
Initial presentation – HLH usually presents as an acute or subacute febrile illness associated with multiple organ involvement. Initial signs and symptoms of HLH can mimic common infections, fever of unknown origin, hepatitis, or encephalitis. With few exceptions, the clinical features are similar regardless of whether an underlying genetic defect has been identified. Some patients have chronic stuttering presentations, with recurrent fevers of unknown origin and manifest only a subset of the classic diagnostic criteria.
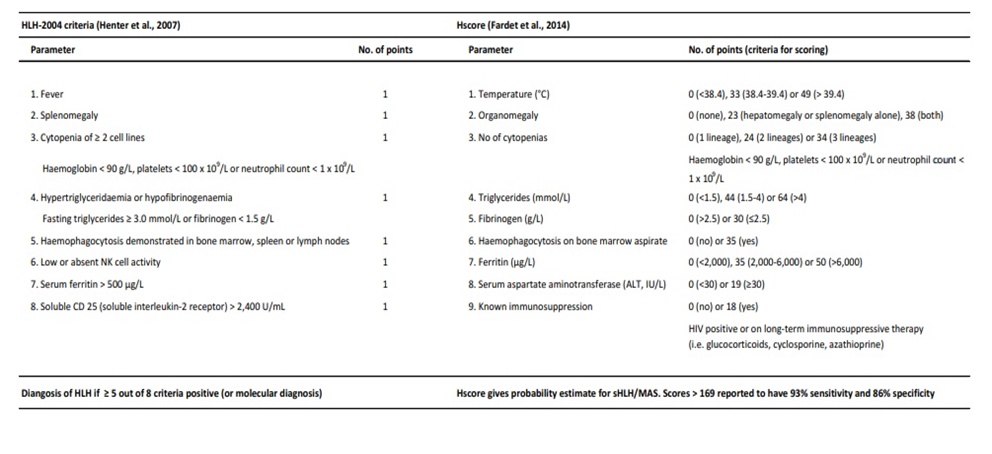
The official diagnosis of HLH, established by the Histiocyte Society, is based on fulfilling one or both of the following criteria:
1. A molecular diagnosis consistent with HLH
2. Five out of the following nine diagnostic criteria for HLH: fever, splenomegaly, cytopenias (affecting two or more of three lineages in the peripheral blood), hypertriglyceridemia, hypofibrinogenemia, elevated ferritin, hemophagocytosis in bone marrow/spleen/lymph nodes, low or absent natural killer (NK)-cell activity, or elevated soluble CD25 (interleukin [IL]-2 receptor).
Approach and Evaluation:
1. History Including travel/drug/sexual/family history etc.
2. Examination Lymphadenopathy, hepato-splenomegaly, rashes, bleeding, signs of organ dysfuction.
3. Initial laboratory tests Full blood count including differential / blood film Routine renal biochemistry and electrolyes Serum ferritin, triglycerides and C-reactive protein.
4. Liver function tests, including AST, ALT, GTT, total bilirubin and LDH.
5. Coagulation screen, including PT, aPTT, fibrinogen, D-dimer ECG, Echocardiogram.
6. Routine imaging CXR Ultrasound scan: abdomen or as clinically indicated CT neck, chest, abdomen, pelvis.
7. Infectious diseases work-up Infectious disease +/- tropical disease consult Cultures from blood, sputum, urine, CSF and other body fluids as clinically indicated.
8. Respiratory virus screen (combined nose/throat swab), HIV screen, hepatitis virology screen EBV, CMV serology and other herpesvirus PCR may be appropriate in paediatric or immunocompromised.
9. Parvovirus B19 serology, Parasitology (blood film for malaria, serology for toxoplasma and leishmaniasis)
10. Fungal screen cultures (BD glucan, PCP from deep respiratory samples).
11. Consider tuberculosis (histopathology, TB cultures +/- TB Gen Xpert of appropriate tissues/fluids as clinically indicated; immunological tests do not have sufficient validity in this setting).
12. Additional tests in immunosuppression Malignancy work-up Haematology consult Bone marrow aspirate / trephine (haemophagocytosis? Leishmania amastigotes?), may need repeat sampling.
13. Auto-immune work-up Rheumatology consult Auto-immune screen.
14. Immunological profiling Other / miscellaneous Cerebrospinal fluid analysis (abnormal in 50%)
15. MRI brain PET scan (infection, malignancy) Tissue sampling (lymphnodes, spleen biopsy etc.)
16. Genetic testing (no acute role; as advised by HLH expert)
Laboratory and radiographic abnormalities:
⦁ Cytopenias — Cytopenias, especially anemia and thrombocytopenia, are seen in >80 percent of patients on presentation. Platelet counts range from 3000 to 292,000 and hemoglobin levels of 3.0 to 13.6 are typical.
⦁ Serum ferritin levels — A very high serum ferritin level is common in HLH and, especially in children, has high sensitivity and specificity. In the HLH-94 study, ferritin levels greater than 500, 5000, and 10,000 ng/mL were seen in 93, 42, and 25 percent, respectively. Serum ferritin in this range is seen in very few other inflammatory disorders in children, and when it does occur in other syndromes, it is often in the setting of iron overload syndromes (eg, in multiply transfused patients). In adults and neonates, other potential causes of extremely high ferritin levels should also be evaluated. As an example, ferritin levels over 10,000 ng/mL can be seen in neonatal hemochromatosis or fulminant liver failure. While a very high ferritin level is helpful in suggesting the possibility of HLH, a low ferritin (eg, ferritin <500 ng/mL) does not exclude the possibility of HLH. A relatively normal ferritin can occasionally be seen in HLH genetic syndromes. Macrophages are a primary source of ferritin, which may account for the association between HLH and very high ferritin levels.
⦁ Liver function and coagulation abnormalities — Nearly all patients with HLH will have hepatitis, manifested by elevated liver function tests (LFTs), including liver enzymes (AST, ALT, GGT), lactate dehydrogenase (LDH), and bilirubin. Increased triglycerides and abnormal coagulation parameters (especially elevated D-dimer) caused by hepatic dysfunction and disseminated intravascular coagulopathy are also frequently seen. The degree of abnormality ranges from mild to hepatic failure. Liver enzyme levels greater than three times the upper limit have been reported in 50 to 90 percent of patients with HLH , LDH is elevated in 85 percent. Bilirubin levels between 3 and 25 mg/dL are seen in greater than 80 percent. The GGT level is an especially sensitive number to follow because of biliary tract infiltration by lymphocytes and macrophages.
⦁ Hypertriglyceridemia can be due to severe liver involvement, but may not be elevated until the liver has been affected for some time. In a review of patients with HLH associated with a variety of triggers, 68 percent had elevated triglycerides at diagnosis or during the course of the disease]. Coagulation abnormalities due to impaired hepatic synthetic function and/or disseminated intravascular coagulation are common.
⦁ Neurologic findings — Neurologic abnormalities have been observed in one-third of patients with HLH, are highly variable, and may include seizures, mental status changes (including severe changes consistent with encephalitis), and ataxia. Patients with HLH are at risk of developing posterior reversible encephalopathy syndrome (PRES), which presents with headache, altered consciousness, visual disturbances, and/or seizures. On examination, patients may have retinal hemorrhages and optic nerve edema. PRES is associated with characteristic findings on brain magnetic resonance imaging (MRI), including vasogenic cerebral edema predominantly in the posterior cerebral hemispheres.
⦁ MRI of the brain in patients with HLH also may show hypodense or necrotic areas. Approximately 50 percent of patients have abnormalities of the cerebrospinal fluid, which may carry an increased risk for mortality and neurologic sequelae.
Treatment:
For primary HLH, the first step in treatment is generally to suppress the overactive immune system. This is often done using a combination of steroids and chemotherapy, with the goal of putting the disease into remission. After initial treatment, patient will usually undergo an allogeneic stem cell transplant, which replaces their defective immune system with a healthy one from a donor. Donor cells may come from a sibling, a parent or an unrelated donor. A stem cell transplant offers patients the best chance for a cure.
For secondary HLH, the aim is to identify and treat the underlying cause of HLH (such as an infection or cancer). In many cases, by treating the underlying cause, HLH will go into remission. In some cases, however, it will be necessary to use steroids and/or chemotherapy to treat the condition – similar to treatment for primary HLH. Treatment for secondary HLH is determined more by the severity of the disorder and its symptoms, rather than its classification.
The biggest hurdle in HLH treatment is identifying alternatives for children who don’t respond to currently available combinations of chemotherapy, steroids and stem cell transplantation.
Conclusion:
HLH is a diverse condition with many causes and is likely under-recognized, which contributes to its high morbidity and mortality. HLH is not a disease in itself but rather a clinical syndrome of extreme hyperinflammation, which is triggered by infection, auto-immunity or malignancy, amongst others. Early recognition is crucial for any reasonable attempt at curative therapy to be made. A number of recent studies have contributed to the understanding of HLH pathophysiology, leading to alternate treatment options; however, much work remains to raise awareness and improve the effectiveness of treatment regimens. It should be suspected and actively investigated in any unwell patient with unexplained fever, cytopenias, progressive organ dysfunction and failure to respond to intensive infection management. Treatment revolves around high-quality supportive care, early anti-inflammatory and immunosuppressive therapy and identification and treatment of any precipitating pathology. In a patient with undifferentiated rapidly progressing organ failure, or if the presumed sepsis diagnosis doesn’t quite “feel” right or respond appropriately – think, could this be HLH?
ACKNOWLEDGEMENT:
For guiding me with the article, I would like to thank, Dr.Aslesha (Clinical lead – Emergency Department)
“The author declares no conflict of interest”
REFERENCES:
- Jordan MB, Allen CE, Greenberg J, et al. Challenges in the diagnosis of hemophagocytic lymphohistiocytosis: Recommendations from the North American Consortium for Histiocytosis (NACHO). Pediatr Blood Cancer 2019; 66:e27929.
- Filipovich A, McClain K, Grom A. Histiocytic disorders: recent insights into pathophysiology and practical guidelines. Biol Blood Marrow Transplant 2010; 16:S82.
- Pachlopnik Schmid J, Côte M, Ménager MM, et al. Inherited defects in lymphocyte cytotoxic activity. Immunol Rev 2010; 235:10.
- Risma K, Jordan MB. Hemophagocytic lymphohistiocytosis: updates and evolving concepts. Curr Opin Pediatr 2012; 24:9.
- Egeler RM, Shapiro R, Loechelt B, Filipovich A. Characteristic immune abnormalities in hemophagocytic lymphohistiocytosis. J Pediatr Hematol Oncol 1996; 18:340.
- Eife R, Janka GE, Belohradsky BH, Holtmann H. Natural killer cell function and interferon production in familial hemophagocytic lymphohistiocytosis. Pediatr Hematol Oncol 1989; 6:265.
- Ishii E, Ueda I, Shirakawa R, et al. Genetic subtypes of familial hemophagocytic lymphohistiocytosis: correlations with clinical features and cytotoxic T lymphocyte/natural killer cell functions. Blood 2005; 105:3442.
- Stepp SE, Dufourcq-Lagelouse R, Le Deist F, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science 1999; 286:1957.
- Dalal BI, Vakil AP, Khare NS, et al. Abnormalities of the lymphocyte subsets and their immunophenotype, and their prognostic significance in adult patients with hemophagocytic lymphohistiocytosis. Ann Hematol 2015; 94:1111.
- Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell 2010; 140:805.
- Behrens EM, Canna SW, Slade K, et al. Repeated TLR9 stimulation results in macrophage activation syndrome-like disease in mice. J Clin Invest 2011; 121:2264.
- Fall N, Barnes M, Thornton S, et al. Gene expression profiling of peripheral blood from patients with untreated new-onset systemic juvenile idiopathic arthritis reveals molecular heterogeneity that may predict macrophage activation syndrome. Arthritis Rheum 2007; 56:3793.
- Henter JI, Elinder G, Söder O, et al. Hypercytokinemia in familial hemophagocytic lymphohistiocytosis. Blood 1991; 78:2918.
- Osugi Y, Hara J, Tagawa S, et al. Cytokine production regulating Th1 and Th2 cytokines in hemophagocytic lymphohistiocytosis. Blood 1997; 89:4100.
- Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol 2014; 14:36.
- Aricò M, Danesino C, Pende D, Moretta L. Pathogenesis of haemophagocytic lymphohistiocytosis. Br J Haematol 2001; 114:761.
- Komp DM, McNamara J, Buckley P. Elevated soluble interleukin-2 receptor in childhood hemophagocytic histiocytic syndromes. Blood 1989; 73:2128.
- Tang Y, Xu X, Song H, et al. Early diagnostic and prognostic significance of a specific Th1/Th2 cytokine pattern in children with haemophagocytic syndrome. Br J Haematol 2008; 143:84.
- Takada H, Ohga S, Mizuno Y, et al. Increased IL-16 levels in hemophagocytic lymphohistiocytosis. J Pediatr Hematol Oncol 2004; 26:567.
- Mazodier K, Marin V, Novick D, et al. Severe imbalance of IL-18/IL-18BP in patients with secondary hemophagocytic syndrome. Blood 2005; 106:3483
- Pagel J, Beutel K, Lehmberg K, et al. Distinct mutations in STXBP2 are associated with variable clinical presentations in patients with familial hemophagocytic lymphohistiocytosis type 5 (FHL5). Blood 2012; 119:6016.
- Lee SM, Sumegi J, Villanueva J, et al. Patients of African ancestry with hemophagocytic lymphohistiocytosis share a common haplotype of PRF1 with a 50delT mutation. J Pediatr 2006; 149:134.
- Feldmann J, Le Deist F, Ouachée-Chardin M, et al. Functional consequences of perforin gene mutations in 22 patients with familial haemophagocytic lymphohistiocytosis. Br J Haematol 2002; 117:965.
- Ueda I, Ishii E, Morimoto A, et al. Correlation between phenotypic heterogeneity and gene mutational characteristics in familial hemophagocytic lymphohistiocytosis (FHL). Pediatr Blood Cancer 2006; 46:482.
- Ramos-Casals M, Brito-Zerón P, López-Guillermo A, et al. Adult haemophagocytic syndrome. Lancet 2014; 383:1503.
- Kris Bauchmuller1 , Jessica J. Manson2 , Rachel Tattersall3 , Michael Brown4 , Christopher McNamara5 , Mervyn Singer6 and Stephen J. Brett7
- Karakike E and Giamarellos-Bourboulis EJ. Macrophage Activation-Like Syndrome: A Distinct Entity Leading to Early Death in Sepsis. Front Immunol. 2019; 10: 55.
- Chellapandian D, Das R, Zelley K, et al. Treatment of Epstein Barr virus-induced haemophagocytic lymphohistiocytosis with rituximab-containing chemo-immunotherapeutic regimens. Br J Haematol. 2013; 162: 376-82.
- Buyse S, Teixeira L, Galicier L, et al. Critical care management of patients with hemophagocytic
- lymphohistiocytosis. Intensive Care Med. 2010; 36: 1695-702.
- Machowicz R, Janka G and Wiktor-Jedrzejczak W. Similar but not the same: Differential diagnosis of HLH and sepsis. Crit Rev Oncol Hematol. 2017; 114: 1-12.
Kenneth L McClain, MD, PhD and Olive Eckstein, MD, et al.
 Dr.Silvera Samson Raj
Dr.Silvera Samson Raj
MRCEM Resident,
Kauvery Hospital, Chennai.