INTRODUCTION
- Laparoscopy has gained popularity nowadays as it has advantage of lesser post-operative pain, shorter duration of hospital stay and early ambulation
- However, the pneumoperitoneum created during the laparoscopy alters patients physiological and hemodynamic profile. Pneumoperitoneum is commonly created by CO2 which can also alters cardiac stability
- Pneumoperitoneum created during laparoscopy results in increase in mean arterial pressure (MAP), systemic vascular resistance, mean pulmonary artery pressure and decrease in cardiac output (CO)
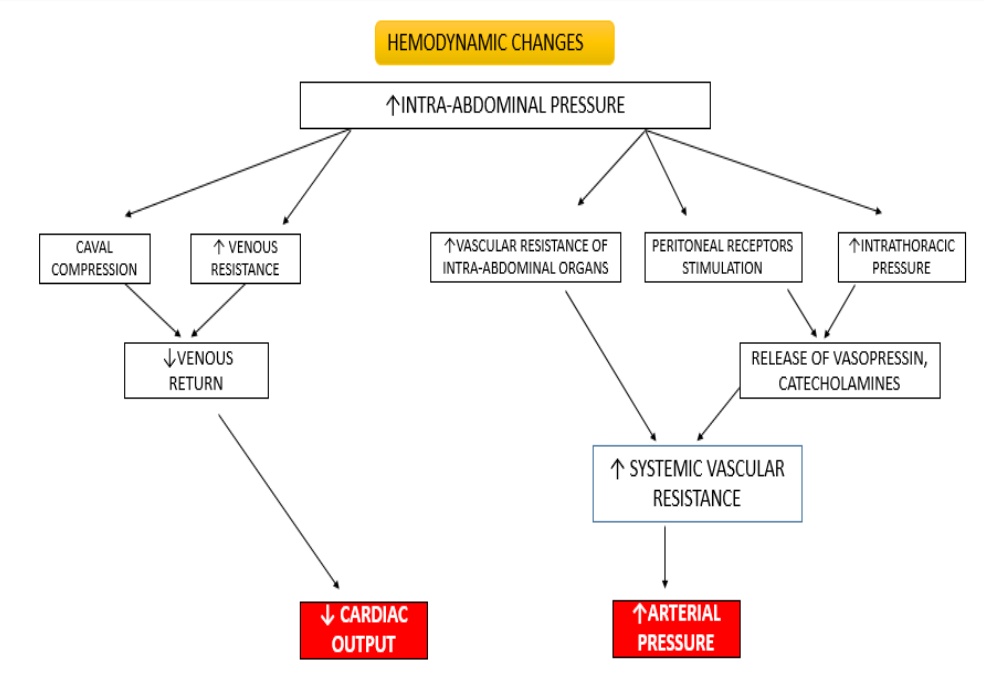
- Cardiac output is further decreased with reverse Trendelenburg position which is commonly used in laparoscopic procedures
- These changes well tolerated in young patients but it could be detrimental in cardiac compromised patients
MAGNESIUM is the second abundant cation of the intracellular fluids.
- It regulates several enzymatic functions in the body
- It plays important role with regards to neurochemical transmission and muscular excitability
- Magnesium shown to have block the catecholamine release from the nerve endings and the adrenal medulla
- It also directly acts on vascular smooth muscles causing vasodilation by inhibiting Ca2+ influx through dihydropyridine sensitive, voltage-dependent channels
- Magnesium also a potent antagonist of N-Methyl-D-aspartate (NMDA)receptor complex resulting in post operative analgesic effect
AIM AND OBJECTIVE
PRIMARY OBJECTIVE
- To assess the efficacy of magnesium sulphate on the attenuation of hemodynamic response to pneumoperitoneum during laparoscopy
SECONDARY OBJECTIVE
- To determine analgesic effect of magnesium sulphate
REVIEW OF LITERATURE
1. British Journal of Anaesthesia 103 (4): 484–9 (2009)
Jee, D. Lee, S. Yun and C. Lee.
“Magnesium sulphate attenuates arterial pressure increase during laparoscopic cholecystectomy”.
This study showed systolic and diastolic blood pressures were higher in the control group than the study group at 10, 20, 30 minutes post pneumoperitoneum. The vasopressin and catecholamine levels were also significantly higher in the control group than the magnesium group. There was no significant difference in the rennin and cortisol levels between the two groups.
2. Journal of Research in Medical Sciences 2005; 10(2): 82-86
Montazeri MD, M. Fallah MD.
“A Dose – Response Study of Magnesium Sulfate in Suppressing Cardiovascular Responses to Laryngoscopy & Endotracheal Intubation”. This study was aimed at finding optimal dose of magnesium sulphate in attenuation of cardiovascular response in laryngoscopy and endotracheal intubation
6 groups were divided and each group received 10,20,30,40,50 mg/kg of intravenous magnesium sulphate and last group received 1.5mg/kg of lidocaine
Conclusion – There was no significant difference in the monitored parameters among magnesium groups but cardiovascular suppression effects was more in magnesium than lignocaine
3. Anesthesia Essays and Researches
Jan-Mar 2017 – Volume 11 – Issue 12.
Kamble, Shruthi P.; Bevinaguddaiah, Yatish; Nagaraja, Dinesh Chillkunda; Pujar, Vinayak S.; Anandaswamy, Tejesh C.
“Effect of Magnesium Sulfate and Clonidine in Attenuating Hemodynamic Response to Pneumoperitoneum in Laparoscopic Cholecystectomy”- 90 ASA Classes I and II patients posted for elective laparoscopic cholecystectomy were randomized into three groups of thirty patients each. Group 1 received injection clonidine 1 μg/kg diluted in 10 mL normal saline over 10 min, prior to pneumoperitoneum. Group 2 received injection magnesium sulfate 50 mg/kg diluted in 10 mL normal saline over 10 min, prior to pneumoperitoneum. Group 3 received 10 mL normal saline intravenously over 10 min, prior to pneumoperitoneum. All the monitored parameters were noted prior and after the pneumoperitoneum
Conclusion – Both magnesium and clonidine attenuated the hemodynamic response to pneumoperitoneum. However, magnesium 50 mg/kg, attenuated hemodynamic response better than clonidine 1 μg/kg
4. Anesthesia Essays and Researches
Anesth Essays Res. 2013 May-Aug; 7(2): 228–231.
doi: 10.4103/0259-1162.118970: 10.4103/0259-1162.118970
Suhrita Paul, Pabitra Biswas, Dhurjoti Prosad Bhattacharjee, and Janmejoy Sengupta
“Effects of magnesium sulfate on hemodynamic response to carbon dioxide pneumoperitoneum in patients undergoing laparoscopic cholecystectomy” – Sixty patients, of either sex (18-65 years of age), undergoing elective laparoscopic cholecystectomy were randomly allocated in one of the two groups containing 30 patients each. One group received magnesium sulfate 30 mg/kg intravenously as a bolus before PP. Another group received same volume of 0.9% saline.
Conclusion – Magnesium sulfate administered before PP attenuates adverse hemodynamic response and provides hemodynamic stability during PP created for laparoscopic surgery.
5. ANAESTHESIA ANALGESIA 1989;68:772-6.
Michael F. M. James, FFARCS, R. Eryk Beer, FFA(SA), and Jan D. Esser, MMED.
“Intravenous Magnesium Sulfate Inhibits Catecholamine Release Associated with Tracheal Intubation” – 2 groups of 15 patients each divided. One group received 60 mg/kg of 50% magnesium sulphate intravenously over 1 minute, while another group received normal saline
Conclusion – The heart rate was unchanged and the rise in systolic blood pressure was insignificant in MgS04 group. This study concludes that magnesium sulphate attenuates the arterial pressure increase and catecholamine response to laryngoscopy and intubation
REFERENCES
- Hodgson C, McClelland RM, Newton JR. Some effects of the peritoneal insufflation of carbon dioxide at laparoscopy. Anaesthesia. 1970 Jul;25(3):382-90.
- Koing H, Wallner T, Marhofer P, Andel H, Horauf K,Mayer N. Magnesium sulfate reduces intra- and postoperative analgesic requirements Anesth Analg 1998; 87: 206-10.
- McLaughlin JG, Scheeres D, Dean R, Bonnell BW. The adverse haemodynamic effects of laparoscopic cholecystectomy. Surg Endosc. 1995;9:121–4
- Joris JL, Hamoir EE, Hartstein GM, Meurisse MR, Hubert BM, Charlier CJ, et al. Haemodynamic changes and catecholamine release during laparoscopic adrenalectomy for pheochromocytoma. Anesth Analg. 1999;88:16–21.
- Koivusalo AM, Scheinin M, Tikkanen I, Yli-Suomu T, Ristkari S, Laakso J, et al. Effects of esmolol on haemodynamic response to CO pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand. 1998;42:510–7.
- Telci L, Esen F, Ackora D, Erden T, Canbolat T, Akpir K. Evaluation of effects of magnesium sulfate in reducing intraoperative anesthetic requirements. Br J Anaesth. 2002;89:594–8.
- O’Leary E, Hubbard K, Tormey W, Cunningham AJ. Laparoscopic cholecystectomy: haemodynamic and neuroendocrine responses after pneumoperitoneum and changes in position. Br J Anaesth 1996; 76: 640–4
- Myre K, Rostrup M, Buanes T, et al. Plasma catecholamines and haemodynamic changes during pneumoperitoneum. Acta Anaesthesiol Scand 1998;42:343–7


 Dr Nirmalraj
Dr Nirmalraj Dr. Karthick Raja Velayutham
Dr. Karthick Raja Velayutham