Acute kidney injury (AKI) is a common and serious complication of cardiac surgery and is associated with a risk of short and long-term mortality.The incidence of acute kidney injury after cardiac surgery (CSA-AKI) is as high as 30%. Approximately 3% of patients require at least temporary renal replacement therapy (RRT) [1] Patients with severe AKI have a three to eightfold higher perioperative mortality, a prolonged ICU and hospital stay.[2]
Risk factors of CSA-AKI can be categorized into patient pre-, intra- and postoperative factors. Preoperative risk factors are largely non-modifiable and include demographics, such as age and gender; conditions such as hypertension, hyperlipidemia, diabetes mellitus, and vascular disease; and end-organ sequelae such as chronic kidney or liver disease, anemia, and previous stroke [3] . The patient’s preoperative hemodynamics and urgency of the surgical indication (e.g., emergency aortic dissection repairs or coronary artery bypass grafting) also increase risk, especially in conditions such as acute coronary syndrome and cardiogenic shock that require an intra-aortic balloon pump (IABP). Intraoperative factors include ischemia time, cardiopulmonary bypass time. Postoperative factors include use of vasoactive medicine, diuretic, blood transfusion.[4].
This study aims to find the incidence of acute kidney injury in patients who have undergone cardiac surgery, their clinical profile and to follow up and assess for outcomes such as duration of hospital stay, worsening AKI, dialysis requirement and in hospital mortality.
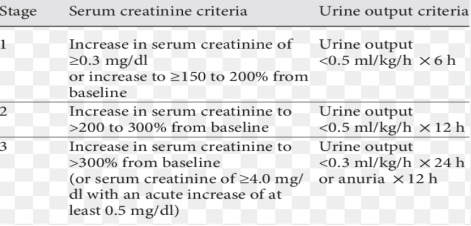
This is a prospective observational study. A total 201 patients who undergo cardiac surgery will be studied. All patients more than 18years of age who have undergone cardiac surgery all included in this study. Exclusion criteria includes patients i) <18 years of age, ii) with chronic kidney disease 5, iii) on dialysis, iv) who have undergone endovascular procedure and v) who decide to withdraw from the study. Patient’s history, preoperative, intraoperative and postoperative data will be collected. Using serum creatinine and urine output AKI stage will be defined using AKIN criteria. Serum creatinine will be measured at hospital admission(preoperative) and daily postoperative. Urine output monitoring will be done during hospital stay. Patients will be followed up for outcomes such as duration of hospital stay, worsening AKI, dialysis requirement and in hospital mortality.
Finding the cause for AKI and taking preventive measures is the mainstay of management. Identification of high-risk patients and categorisation allows earlier intervention and better management. CSA-AKI requires a multimodal approach where both the patient’s pre-operative condition and the effects of the cardiac surgical procedure are considered. Timely intervention requires early recognition of potential actual kidney injury.
References:
- Vandenberghe W, Gevaert S, Kellum JA, Bagshaw SM, Peperstraete H, Herck I, et al. Acute kidney injury in cardiorenal syndrome type 1 patients: a systematic review and meta-analysis. Cardiorenal Med. 2016;6(2):116–28.
- Ortega-Loubon C, Fernandez-Molina M, Carrascal-Hinojal Y, Fulquet-Carreras E. Cardiac surgery-associated acute kidney injury. Ann Card Anaesth. 2016;19(4):687–98
- Huen SC, Parikh CR. Predicting acute kidney injury after cardiac surgery: a systematic review. Ann Thorac Surg. 2012 Jan;93(1):337–47. https://doi.org/10.1016/j.athoracsur.2011.09.010 [PubMed] 0003-4975
- Lagny M.G., Jouret F., Koch J.N., Blaffart F., Donneau A.F., Albert A., Roediger L., Krzesinski J.M., Defraigne J.O. Incidence and outcomes of acute kidney injury after cardiac surgery using either criteria of the RIFLE classification. BMC Nephrol. 2015;16:76. doi: 10.1186/s12882-015-0066-9.
 Dr Yashilha D
Dr Yashilha D Dr R Balasubramaniyam
Dr R Balasubramaniyam Dr B Balaji Kirushnan
Dr B Balaji Kirushnan