Diabetic ketoacidosis (DKA) is defined as clinical syndrome with Ketonaemia > 3.0 mmol/L or significant ketonuria (more than 2+ on standard urine sticks) Blood glucose > 11.0 mmol/L or known diabetes mellitus Serum venous bicarbonate of < 15.0 mmol/L and/or venous pH < 7.3. Oral hypoglycaemic drugs, such as dapagliflozin and empagliflozin, belong to the class of Sodium-Glucose Cotransporter 2 inhibitors (SGLT2i). These drugs function blocking glucose reabsorption at the luminal membrane of the proximal renal tubules. Studies indicate that SGLT2i contribute to reduction in body weight, provide a slight decrease in both systolic and diastolic blood pressure, and may slow disease progression by enhancing β- cell insulin secretion and improving insulin sensitivity in peripheral tissues. These effects are linked to reduction in plasma glucose levels. While the most common side effects are typically mild, including genital mycotic infections and lower urinary tract infections. However, cases of DKA have been reported in patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) using SGLT2 inhibitors, occasionally occurring even without other predisposing factors. We report the case of a female patient who developed DKA associated with acute coronary syndrome after being switched to an SGLT2i several weeks before hospitalization.
CASE REPORT:
A 71-year-old female patient presented with a history of T2DM, came to the emergency department with C/O of difficulty in breathing NYHA class II TO III associated with nausea and vomiting, 1 episode non bilious and non blood stained which had begun 12 hrs back. C/O decreased physical activity associated with generalised tiredness for past 2 days .patient had a recent admission 2 weeks back to our hospital with H/O slip and fall sustaining injury to left elbow and left hip. Diagnosed with distal humerus fracture communited left elbow / undisplaced greater trochanteric fracture – left hip S/P Distal humerus bicolumnar plating left elbow, tension band wiring left elbow, DR boot application – left lower limb, patient is bed bound since then. During discharge Patient was started on dapagliflozin due to poor glycemic control.
Her vital signs were as follows are heart rate of 132 bpm, respiratory rate of 34 rpm, blood pressure of 80/60 mmHg and temperature of 98.6 F. On physical examination, conscious, oriented, tachypnic Kussmaul breathing pattern. On systemic examination, CVS: S1 S2 heard no murmur. RS: B/L AE +/B/L basal crepts ++, CNS: NFND, PA soft non tender, ABG revealed high anion gap metabolic acidosis with type I respiratory failure. The electrocardiogram (ECG) revealed a sinus rhythm with normal axis, and nonspecific repolarization abnormalities TROP I : 1.56 ng/dl ( positive ), POC creatinine : 0.7 mg/dl , sodium 130 mmol/L (135–145), potassium 4.6 mmol/L (3.5–5.5), chloride 101 mmol/L , glucose of 204 mg/dl, HB : 9.2 mg/dl , lac 1.8, HC03 : 12.6, serum ketones : 5.6 .ECHO : global hypokinesia of left ventricle with more of anterior wall hypokinesia with severe LV EF : 30%
Treatment with crystalloids and a continuous intravenous insulin infusion was initiated in the emergency room (ER). The patient was then admitted to the CCU, where more intensive rehydration with crystalloids was administrated, while maintain the initial therapeutic plan unchanged.
Two days later, the patient was shifted to ward from CCU. Due to her elevated troponin levels on admission and coronary risk factors, a coronary angiography was recommended. However, her family declined further evaluation. She was discharged 3 days later with regimen of subcutaneous insulin, aspirin, clopidogrel, atorvastatin and furosemide. The oral antidiabetic treatment with dapagliflozin was not resumed.
DISCUSSION
SGLT 2 INHIBITORS: Dapagliflozin and empagliflozin, A new class of OHA
MOA: SGLT2 inhibitors lower glucose reabsorption in the proximal tubule, causing 50–60% of filtered glucose to be excreted in the urine. Their action is glucose-dependent and ceases when blood glucose levels fall below 90 mg/dL.

Increase in blood ketone bodies – tubular reabsorption – SGLT2i mediated sodium (Na+) reabsorption increases the tubular Na+ concentration, that facilitate the reabsorption of negatively charged ketone bodies by creating an electronegative gradient.
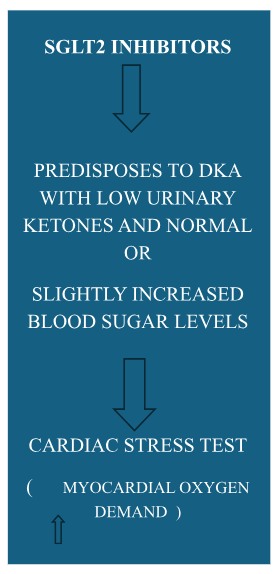
DKA occurs in diabetic patients due to an elevated level of blood ketone bodies, resulting from both increased hepatic production and decreased urinary clearance of ketones. This severe acute complication is associated with a 30% raise in mortality, and SGLT2 inhibitors appear to predispose patients to this rare adverse event, occurring in up to 1 in 1,000 individuals. Both dapagliflozin and empagliflozin have been reported to raise glucagon levels, thereby promoting hepatic ketogenesis.
Ketoacidosis produced by SGLT2 inhibitors have special features
- Blood glucose levelsare normal or slightly increased.
- Ketone body concentrations are low.
This patient presented with vomiting, generalized fatigue, difficulty breathing, and an elevated serum troponin level indicative of a non-ST-elevation myocardial infarction (NSTEMI). While dapagliflozin use has been associated with DKA in the presence of recognized precipitating factors, this case lacked typical symptoms of an acute coronary syndrome, such as chest pain, with absence of clear electrocardiographic signs of ischemia and only a minor elevation of serum troponin, this does not support that an acute coronary syndrome was responsible for such a severe metabolic disturbance. Furthermore, the patient’s tachycardia and tachypnea resolved within hours of correcting the DKA, with normalization of troponin levels and no need for antianginal medications.
These findings suggest that DKA may have acted as a “cardiac stress test,” activating the acute coronary syndrome by increasing oxygen demand. However, we acknowledge the alternative possibility that an acute coronary syndrome initiated the DKA in this patient, who was previously at increased risk due to dapagliflozin therapy, cannot be entirely excluded.
Recommendations for the safer use of SGLT2i contain maintaining a high suspicion for diabetic ketoacidosis (DKA) in patients taking these medications who present with symptoms, even if their blood glucose levels are normal or only slightly elevated.
In such cases, the SGLT2 inhibitor should be discontinued and not restarted until a definitive cause has been identified or the ketoacidosis has resolved. While the benefits of SGLT2 inhibitors continue to outweigh the risks in the treatment of type 2 diabetes mellitus (T2DM), we wish to highlight the potential for SGLT2 inhibitors to cause DKA even when urine ketone levels are undetectable or low and blood glucose is only slightly elevated. Therefore, measuring blood ketones can be particularly useful in these situations.
REFERANCE
-
- Novikov A, Vallon V. Sodium glucose cotransporter 2 inhibition in the diabetic kidney: an update. Current opinion in nephrology and hypertension. 2016 Jan 1;25(1):50-8.
- Fioretto P, Giaccari A, Sesti G. Efficacy and safety of dapagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, in diabetes mellitus. Cardiovascular diabetology. 2015 Dec;14:1-3.
- Storgaard H, Bagger JI, Knop FK, Vilsbøll T, Rungby J. Diabetic ketoacidosis in a patient with type 2 diabetes after initiation of sodium–glucose cotransporter 2 inhibitor treatment. Basic & clinical pharmacology & toxicology. 2016 Feb;118(2):168-70.
- EMA confirms recommendations to minimize ketoacidosis risk with SGLT2 inhibitors for diabetes.
Available at: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/re-ferrals/SGLT2_inhibitors/human_referral _prac_000052.jsp&mid=WC0b01ac05805c516f (accessed April 10 2016).
-
-
- Taylor SI, Blau JE, Rother KI. SGLT2 inhibitors may predispose to ketoacidosis. The Journal of Clinical Endocrinology & Metabolism. 2015 Aug 1;100(8):2849-52.
-
 Dr. Avinash. S
Dr. Avinash. S
Emergency Medicine Resident, Department of Emergency Medicine,
Kauvery Hospital, Alwarpet
 Dr. Ashok Nandagopal
Dr. Ashok Nandagopal
Clinical Lead & Consultant, Department of Emergency Medicine
Kauvery Hospital, Alwarpet