Necrotizing fasciitis (NF) is an aggressive skin and soft tissue infection (SSTI) that cause necrosis of the muscle fascia and subcutaneous tissues. This infection typically travels along the fascial plane, which has a poor blood supply, leaving the overlying tissues initially unaffected, potentially delaying diagnosis and surgical intervention. Consequently early recognition of symptoms is crucial and patients have to be rushed into surgery immediately where a thorough debridement needs to be performed. Diabetic patients exhibit impaired cutaneous wound healing with increased susceptibility to infection and it is therefore reasonable to speculate that this chronic, debilitating disease contributes to a more serious nature of NF.
Patients frequently first present with systemic signs of infection at the general medicine department and not the surgery department. Hence it is essential that NF is taken into consideration as a potential issue when examining patients with symptoms as mentioned in our case.
Case Report
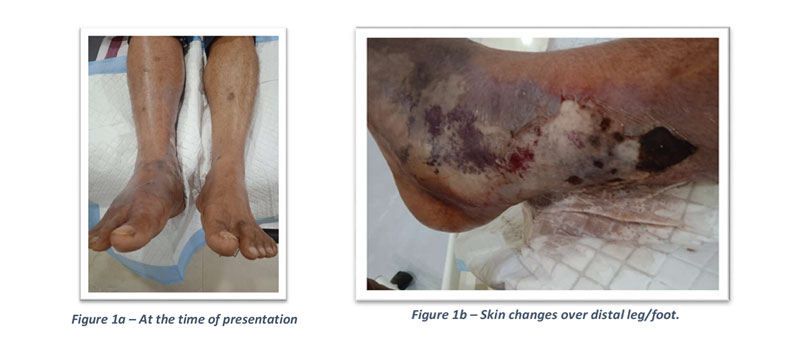
We present a case of a 56 year old male patient who came to the ER with complaints of pain and swelling over the right foot/leg for the past 3 days. We obtained a history of long distance bare foot walking followed by development of blisters over the dorsum of foot/ankle associated with low grade fever which was treated at a local clinic with antipyretic drugs and topical ointment. There was progressive worsening of the condition which was evident by the rupture of blisters along with severe pain and discolouration of the right foot/distal leg. The patient developed high grade fever and was brought to the ER on the 4th day of onset of symptoms on 12-12-2022 for further management.
On examination of the right lower limb we observed skin changes in the medial aspect of the middle/lower third of leg and swelling over the dorsum of the right foot. Distal pulses were not palpable due to the edema (Fig 1a/1b). He was diagnosed as a case of necrotizing fasciitis and was immediately started on IV antibiotics empirically. Basic blood investigations revealed
leucocytosis, increased CRP and HbA1c, indicative of severe infection and poorly controlled diabetes mellitus.
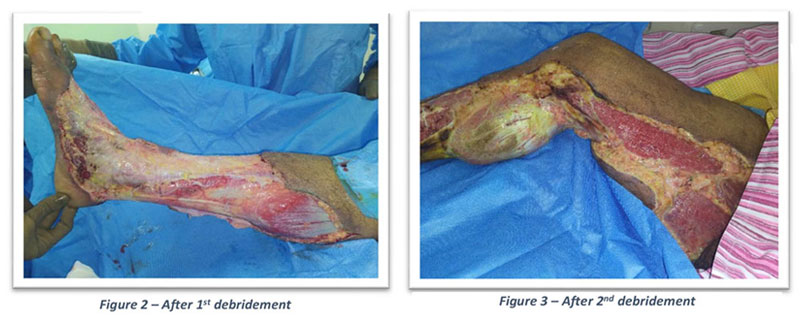
The patient was taken up for emergency exploration and wound debridement of the right lower limb on 13-12-2022 (Fig 2) and tissue sample was sent for culture/sensitivity. C/S reports revealed Beta Haemolytic Streptococci growth and he was started on appropriate antibiotics. We noticed ascending infection and an increase in the WBC count even after the above treatment. In addition the patient also developed necrotic patch with blisters over the right groin region. He was taken up for a second exploration and wound debridement (15-12-2022) which extended up to the medial aspect of upper thigh (Fig 3).
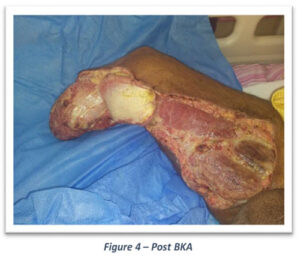
Inspite of the above mentioned interventions, patients’ blood picture showed increasing trend in the WBC count and CRP. Further tissue samples also revealed beta haemolytic streptococci growth and he was initiated on crystalline penicillin. Patient started responding well to the crystalline penicillin but unfortunately the distal leg/ankle/foot were severely compromised due to the aggressiveness of the infection and a below knee amputation was suggested citing a non- salvageable leg/foot. BKA was done and debridement of the thigh and knee tissues were performed on 21-12-2022 (Fig 4).
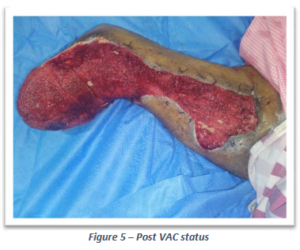
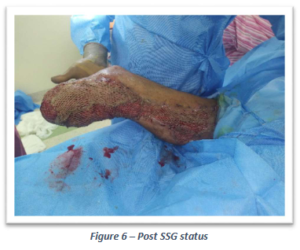
Patient showed immediate improvement and blood picture showed near normal WBC counts and CRP levels. Patient improved symptomatically and was put on vacuum assisted closure system (VAC) on 28-12- 2022 to enable hastened healing of the raw area (Fig 5) which was followed by split skin grafting on 19-01-2023 (Fig 6). The patient is now well on the road to recovery. Our aim is to rehabilitate and get him back to his routine as early as possible with the aid of various prosthetics available in the market.