Introduction:
The term intraperitoneal focal fat infarction (IFFI) refers to a variety of self –limiting clinical conditions causing localized necrosis of fatty tissue. Most IFFI cases are associated with torsion or infarction of the greater omentum or epiploic appendages. Although less frequently, torsion of peri gastric ligaments can also lead to fat infarction. Clinically, IFFI can mimic other conditions such as acute appendicitis or diverticulitis, which complicates accurate diagnosis. Imaging modalities like ultrasound (US) and computed tomography (CT) demonstrate high sensitivity and specificity for diagnosing IFFI while excluding other conditions. In most cases, the clinical progression is favorable without the need for intervention, thus reducing unnecessary surgical procedures. This article imaging spectrum of IFFI cases seeks to identify specific patterns of involvement.
Clinical presentation:
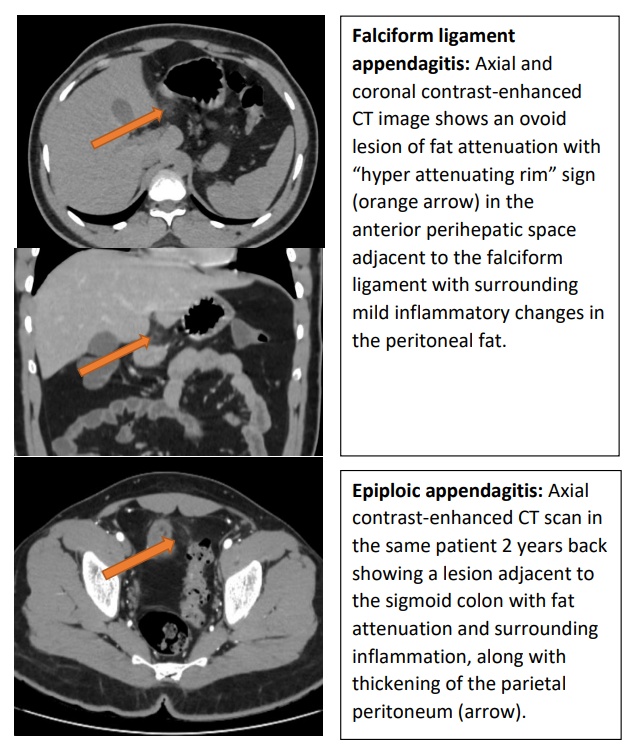
Case 1: A 21 year old male came to emergency department with complaints of abdominal pain for past 1 week associated with loose stools and vomiting. He had a previous history of epiploic appendagitis 2 years back.
Case 2: A 17 year old male came to emergency department with history of upper abdominal pain on and off for past 2 weeks. History of laparoscopic appendectomy 1 year back.
Case 3: A 27 year old female came to emergency department with complaints of abdominal pain with fever chills for past 3 days.
Discussion:
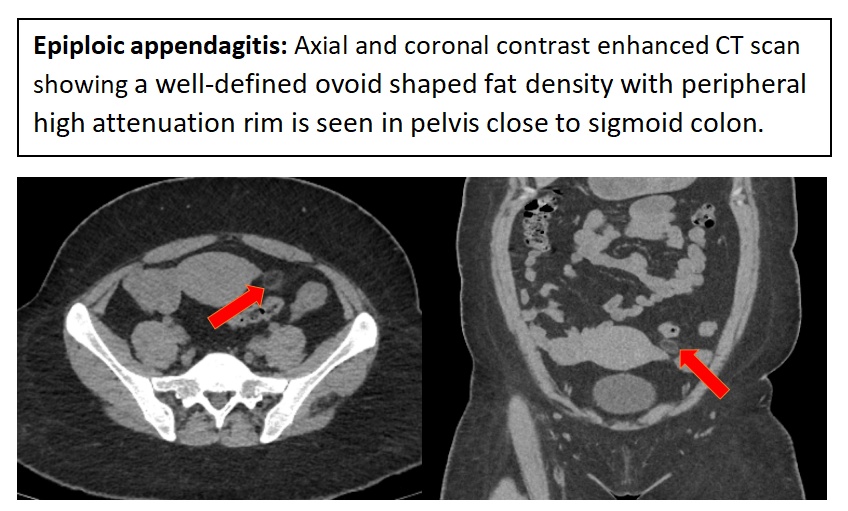
Epiploic appendagitis:
Epiploic appendages are small, fatty protrusions composed of adipose tissue and blood vessels, found along the surface of the large intestine, particularly between the cecum and the recto sigmoid junction. Patients with epiploic appendagitis typically report pain in either the right or left lower quadrant of the abdomen. The most frequent sites for epiploic appendagitis, in descending order, are near the sigmoid colon, descending colon, right hemi colon, and very infrequently, the transverse colon.
In emergency situations, imaging techniques such as computed tomography (CT) and ultrasound (US) are highly effective for assessing suspected cases of epiploic appendagitis. Magnetic resonance imaging (MRI) is often preferred for pediatric patients and during pregnancy. Typical ultrasound findings include a rounded, non-compressible area of echogenic fat with a subtle hypoechoic border, located anteriorly or anterolaterally to the colon at the point of maximum tenderness. The “hyper attenuating ring sign” is a key imaging feature associated with primary epiploic appendagitis. Additionally, thickening of the parietal peritoneum is commonly observed, often accompanied by minimal, focal thickening of the adjacent colonic wall. A central hyper dense dot may indicate a thrombosed vein within the inflamed epiploic appendage (known as the central dot sign), but its absence does not exclude the diagnosis. Post-contrast imaging typically shows no enhancement greater than 10 Hounsfield units.
CT findings usually resolve within approximately six months from symptom onset. Follow-up scans may demonstrate various changes, including a reduction in size to residual soft tissue attenuation and eventual resolution. Over time, infarcted epiploic appendages may undergo aseptic fat necrosis, transforming into fibrotic or calcified masses that may exhibit popcorn or eggshell-type calcification.
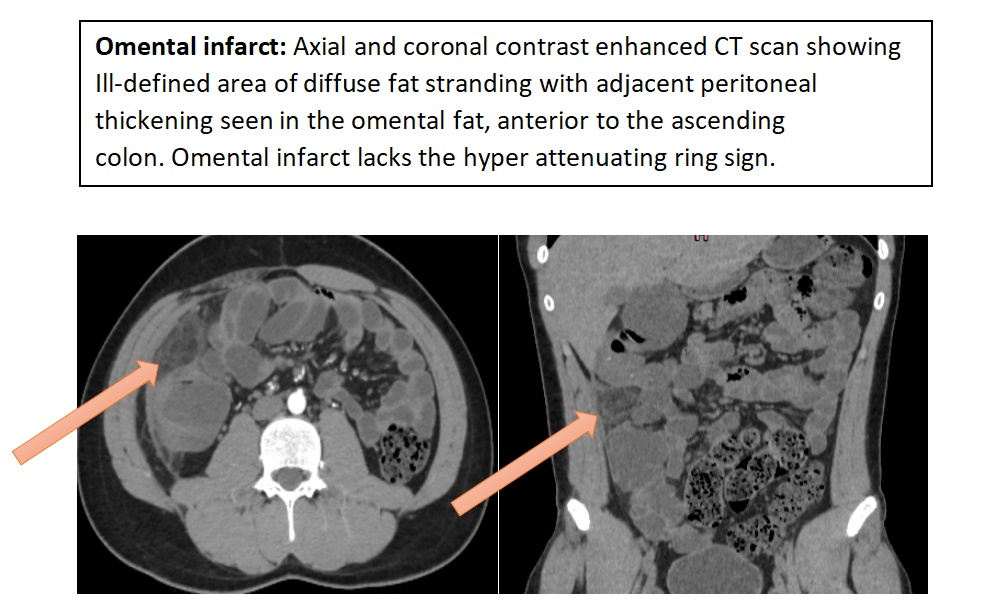
Omental infarct:
The greater omentum is a significant fold of peritoneum that originates from the greater curvature of the stomach and the initial part of the duodenum. It extends downward, covering the lower abdominal organs, before folding back up to attach to the front of the transverse colon. This structure consists of connective tissue, adipose tissue, and lymphatic vessels. Omental infarction (OI) can be categorized into primary and secondary types; however, torsion of the greater omentum is a rare occurrence.
Primary OI occurs spontaneously due to vascular compromise and is typically located in the right inferior region of the omentum, an area known for its more delicate blood supply. The length and mobility of the omentum in this region are thought to increase the risk of torsion. Secondary OI is associated with factors such as abdominal surgery, trauma, tumors, inflammation, and hernia sacs. The clinical presentation of omental infarction typically involves a sudden onset of abdominal pain and tenderness, primarily located in the right iliac fossa. Patients may exhibit mild leukocytosis, and a small percentage may experience a low-grade fever. Nausea and vomiting are generally absent.
Ultrasound can aid in diagnosing omental infarction by revealing a hyperechoic, non-compressible mass in the area of maximum tenderness. However, computed tomography (CT) is regarded as the gold standard for diagnosis. Typically, omental infarction appears on CT as a cake-like fat area larger than 5 cm with surrounding inflammatory changes, lacking the hyper attenuating ring characteristic of epiploic appendagitis. In cases of torsion, a swirling pattern of the omental vessels may be observed on CT, known as the “whirl sign.” Both CT and MRI yield similar imaging results. Early or mild infarction may present as slight haziness in the fat anterior to the colon, while adjacent colonic wall thickening may occur if inflammation spreads.
For hemodynamically stable patients, conservative treatment includes anti-inflammatory medications, oral analgesics, and prophylactic antibiotics.
Falciform ligament appendagitis:
Intraperitoneal focal fat infarction can infrequently affect the perigastric ligaments, which encompass the gastro hepatic, gastro splenic, spleno renal, hepatoduodenal, gastro colic, and falciform ligaments. These ligaments extend from the stomach and envelop vital structures such as blood vessels, lymphatics, lymph nodes, nerves, and surrounding adipose tissue, establishing anatomical connections between the liver, pancreas, spleen, stomach, and transverse colon. Notably, the lower section of the falciform ligament is created by the regression of the umbilical vein and contains both the falciform artery and Para umbilical veins. The fatty protrusions associated with these ligaments can undergo spontaneous torsion, leading to compromised blood flow and subsequent inflammation or ischemia.
Patients often present with sudden epigastric pain that may be accompanied by a mild fever, while other gastrointestinal symptoms are usually absent. Ultrasound imaging may reveal torsion of the fatty appendage in the perigastric and falciform ligaments as a hyperechoic, non-compressible heterogeneous mass at the site of pain. On CT scans, this torsion appears as an oval, well-defined area with fat density and is often associated with inflammatory changes in nearby fat planes. Post-contrast CT does not provide additional diagnostic value. Due to its potential to mimic more serious conditions, many patients undergo laparoscopy for diagnosis. However, when identified prior to surgery, conservative management has proven effective.
Conclusion:
Epiploic appendagitis, omental infarct and falciform ligament appendagitis are classified under IFFI, are conditions characterized by self-limiting occurrences where torsion or vascular blockage results in necrotic adipose tissue. These conditions can present acutely and may resemble various other medical issues. It is important for the radiologist to provide a correct diagnosis and ensuring correct patient management to avoid unnecessary surgery.
References
- Ghahremani GG, White EM, Hoff FL (1992) Appendices epiploic of the colon: radiologic and pathologic features. Radiographics.
- Sand M, Gelos M, Bechara FG et al (2007) Epiploic appendagitis– clinical characteristics of an uncommon surgical diagnosis. BMC Surg.
- Lloyd T (2006) Primary torsion of the falciform ligament: computed tomography and ultrasound findings. Australas.
- Kamaya A, Federle MP, Desser TS (2011) Imaging manifestations of abdominal fat necrosis and its mimics. Radiographics.
 Dr. Sathya Narayanan R
Dr. Sathya Narayanan R
Consultant Diagnostic and Interventional Radiology
Kauvery Hospital Chennai
 Dr Kanagasabai Kamalasekar
Dr Kanagasabai Kamalasekar
Consultant Radiology
Kauvery Hospital Chennai
 Dr Kirthi Chandra
Dr Kirthi Chandra
Junior Consultant
Kauvery Hospital Chennai
 Dr.M.Shirazi
Dr.M.Shirazi
Consultant Physician
Kauvery Hospital Chennai

Dr. Deepan
Consultant
Kauvery Hospital Chennai