History:
Mrs. Kothai 66yrs old female diagnosed as a case of metastatic lung carcinoma. History of bilateral lower limb swelling for past 3 months. History of blackish discolouration of face, hands and feet. She was referred for plain X-ray.
Examination:
A physical examination revealed fluid collection around ankle and knee joint; there was also discomfort at the joints when touched. Clubbing was observed on fingers and toes on both the right and left side. Laboratory evaluation revealed positive BRAF-V600E.Notable negative labs include EGFR, ALK, ROS, MET, KRAS, NTRK.
Imaging Findings:
X-ray of forearm, leg showed smooth solid periosteal thickening of radius, ulna, tibi and fibula without an underlying bone lesion.
Diagnosis:
Pulmonary Hypertrophic Osteoarthropathy secondary to metastatic non small cell lung carcinoma.
Discussion:
Background:
Hypertrophic osteoarthropathy (HOA) is a condition which is distinguished by anomalous multiplication of periosteal tissue and shows three distinct features – digital clubbing, periosteal reaction of long bones and polyarthritis.
Clinical Perspective:
Secondary HOA accounts for 95-97%. Pulmonary causes for HOA include bronchogenic carcinoma, pleural mesothelioma, chronic bronchitis, bronchiectasis, pulmonary fibrosis, and pneumoconiosis.
Secondary HOA due to malignancy is reported only in 12% of children. The malignancy could take the form of nasopharyngeal carcinoma, Hodgkin lymphoma, osteosarcoma and pulmonary squamous cell carcinoma.
The primary form, also termed pachydermo periostosis, is an autosomal dominant condition characterized by coarsening of facial features, mild bone and joint involvement and early onset of disease, usually in the second decade of life.
Extrapulmonary diseases that cause HOA include cyanotic congenital heart disease, bacterial endocarditis, inflammatory bowel disease, acquired immune deficiency syndrome, cystic fibrosis and sarcoidosis. HOA most frequently associated with squamous and adenocarcinoma and least frequently with small cell lung carcinoma.
Pathophysiology:
Increase in PDGF or platelet-derived growth factor and VEGF or vascular endothelial growth factor could be the possible reasons for the clubbing and periosteal reaction. There are some theories which propose hypoxia or inflammation as responsible for the increase of systemic PDGF and VEGF. Yet another theory suggests right to left shunts cause microthrombi to entrench in arterioles of distal extremity which once again causes increase in PDGF and VEGF.
Imaging Perspective:
Radiography shows fluid collection with non-appearance of joint space constriction, periarticular osteopenia, osteophyte development and erosions.
An important radiography characteristic of HOA is proportionate, level, uninterrupted periosteal reaction of diaphysis and metaphysis of tubular bones. The periostitis presents as a single layer of periosteal new bone development. With advancement of the condition, many layered or laminated periostitis can be observed with epiphysis association.
Though there are other processes that may result in periostitis, bilateral smooth periosteal reaction with the absence of underlying lesion does raise doubts for HOA. Therefore, there is a need for immediate and additional assessment involving imaging tests for chest and abdomen.

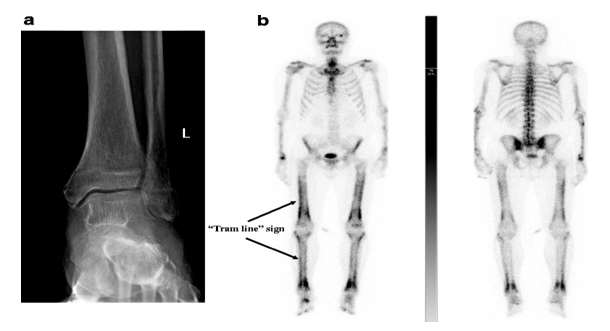
Figure 1 shows smooth solid periosteal reaction of tibia and fibula

Figure 2 shows smooth solid periosteal reaction of radius and ulna
Nuclear Medicine:
Tc-99m MDP bone scan
- Symmetric linear increase in tracer accumulation along diaphyseal and metaphyseal surfaces of long bones
- Tram-track sign
Figure 3 shows symmetric linear increase in tracer accumulation along diaphyseal and metaphyseal surfaces of long bones.
Treatment and Prognosis:
Rapid regression of hypertrophic osteoarthropathy is achieved in cases where the underlying cause is identified and treated; such as a radically treated lung tumor. Results are less successful in the presence of metastatic disease.
In primary hypertrophic osteoarthropathy, symptomatic relief can be obtained by use of NSAIDs, corticosteroids or bisphosphonates.
Differential Diagnosis:
General imaging differential considerations include:
- Chronic venous insufficiency
- Thyroid acropachy
- Hypervitaminosis A
- Voriconazole induced periostitis
On bone scintigraphy, differentials include:
- Normal variant-lateral cortices of the tibiae often appear with a symmetric linear uptake
- Shin splints-can appear similar, but confined to the tibiae
- Chronic venous insufficiency
-
- can cause symmetrical periosteal uptake
- usually confined to the lower extremities below the knees
References:
- Till D. Lerch et al., The Bone & Joint Journal, 2019
- Andegoni M Sandalakis, British Journal of Cardiac Nursing, 2014
- P Kothari et al.,British Journal of Hospital Medicine, 2013
- Nguyen S, Hojjati M. Review of current therapies for secondary hypertrophic pulmonary osteoarthropathy. ClinRheumatol. 2011;30(1):7-13. doi: 10.1007/s10067-010-1563-7