INTRODUCTION
- T-cell mediated rejection(TCMR) occurs in 10%-12% of renal allografts with current immunosuppresants. It can develop at any time as early as a week to as late as years. Some of the risk factors are poor compliance, inadequate immunosuppression, HLA mismatch and no induction.
AIM
- To study the pattern of TCMR in renal allografts To assess the outcomes in these patients.
MATERIALS AND METHODS
- Retrospective analysis of Clinical characteristics, laboratory data, renal biopsy reports, precipitating factors, treatment modalities and follow up data.
- The study period was between March 2015-July 2023
- Inclusion criteria: Biopsy proven TCMR
- Exclusion criteria: Combined ABMR and TCMR
RESULTS
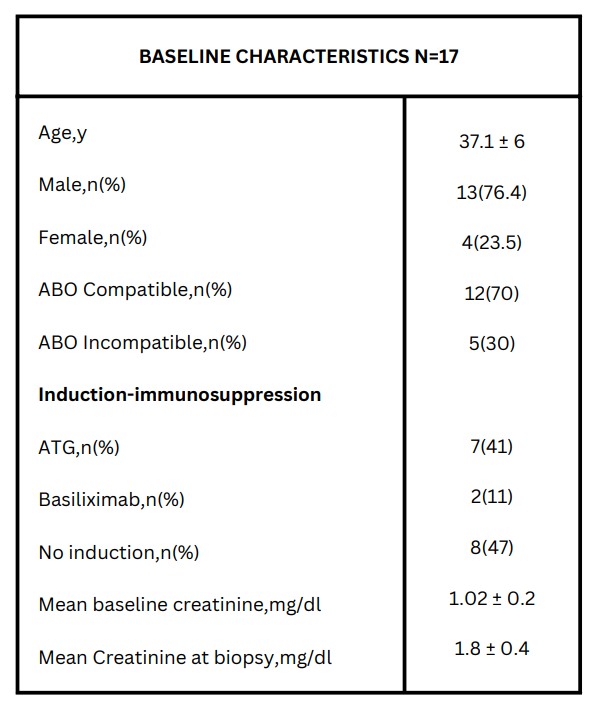
- Data of 110 renal transplantation reports was analyzed It includes 102 live related donors and 8 deceased donors.17 Patients had TCMR
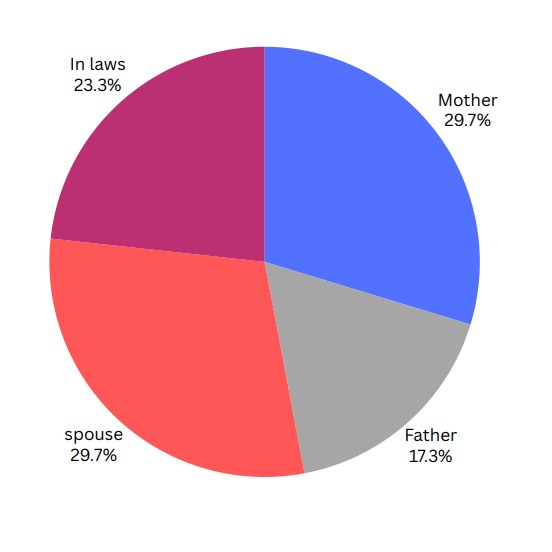
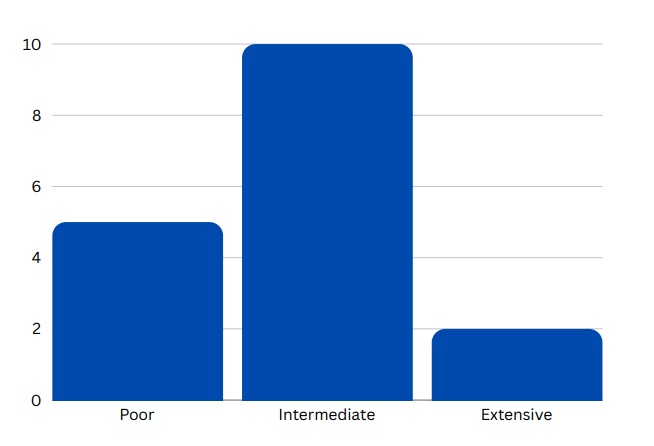
TAC METABOLIZER STATUS
HLA MATCHING
- HAPLO=9(53%)
- MISMATCH=5(29.5%)
- 1/6 MATCH=3(17.5%)
TIME OF REJECTION
- IMMEDIATE : 3(18%)
- 1-6 MONTHS : 9(53%)
- 6MONTHS -1YR : 3(18%)
- > 1YEAR : 2(11%)
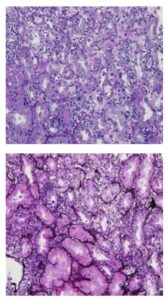
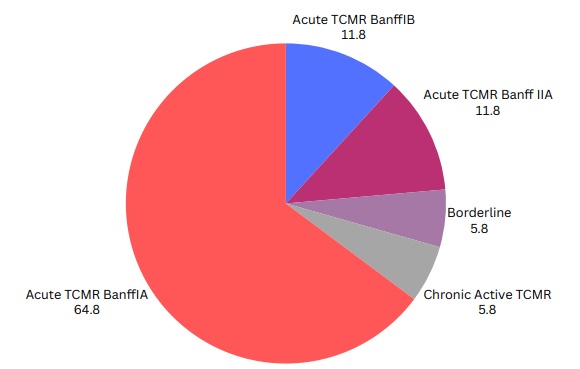
Patterns of TCMR
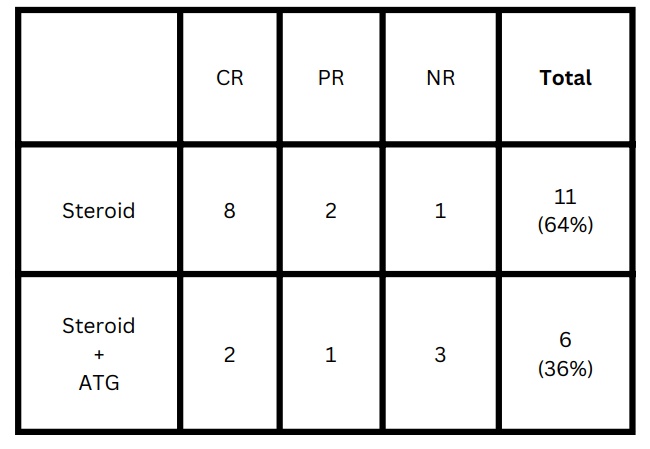
TREATMENT
Intravenous Methylprednisolone at 500mg/day 3 doses followed by oral steroids 1mg/kg and gradually tapered. Patients in whom serum creatinine did not show improvement with pulsing steroids and BANFF 2A were further treated with ATG. We defined Response based on eGFR improvement from nadir(at biopsy) to baseline eGFR before rejection, 1-3 month after treatment. complete(CR) with in 5ml decline from baseline, Partial(PR) >5ml to <25ml,No response >30ml decline.
OUTCOMES: SHORT TERM
LONG TERM
- NORMAL RENAL FUNCTION: 4(23.5%)
- CHRONIC ALLOGRAFT NEPHROPATHY: 4(23.5%)
- GRAFT LOSS: 5(29%)
- DIED WITH FUNCTIONING GRAFT: 4(23.5%)
DISCUSSION
All the 17 cases were live related renal transplantation. Parental donors were the most, as Haploidentical was 53%.Induction agent used in 9(52%).Most common pattern was TCMR 1A(64.8%) .S. Creatinine reached pre-rejection levels in 60% of patients. Low tacrolimus level were seen in 5(30%) pts. Compliance was good in most of the patients. Studies have shown that acute rejection of the kidney allograft is associated with chronic graft dysfunction and has a negative impact on long-term kidney graft outcomes. A higher grade of Banff rejection on the kidney biopsy is associated with inadequate response to the treatment and inferior graft survival. Functional recovery after rejection treatment is an important prognostic factor for long-term outcomes.
CONCLUSION
Most patients with TCMR improved intially upon treament as we see complete response in 10(58%) and Partial response in 3(17%).On long term followup 4(23.5%) had normal renal function and 4(23.5%)chronic allograft nephropathy
Reference:
1.Jalalzadeh M, et al. The impact of acute rejection in kidney transplantation on long-term allograft and patient outcome. Nephrourol Mon. 2015;7:e24439.
2.Brennan DC, Malone A. Treatment of Acute T Cell-Mediated (Cellular) Rejection of the Renal Allograft. Lam AQ, ed. UpToDate; 2020.
3. Fernando ,et al.Clinical outcomes of TCMR in renal allografts www.ijtonline.in




 Dr R Balasubramaniyam,
Dr R Balasubramaniyam,  Dr B Balaji Kirushnan,
Dr B Balaji Kirushnan,