CASE REPORT:
A 4 years 6 months old boy with no known comorbidities came to the emergency department with C/O neck pain for the past 3 days unable to extend the neck associated with headache since that morning. Had an episode of vomiting, watery, non bilious and non blood stained . Parents also observed him to be irritable with decreased oral intake after the onset of headache. The child was admitted 4 days back for AGE with dehydration and discharged after a day. After that he had twice presented to ER , once with neck pain with painful neck movements, treated as musculoskeletal pain and again with neck and throat pain with no other associated symptoms was treated supportively for URI.
His vital signs were as follows: heart rate of 100 bpm, respiratory rate of 24 rpm, blood pressure of 90/60 mmHg and temperature of 98.4F. On physical examination, drowsy, arousable to verbal commands, irritable, CRT 2 secs, wt: 14.6kg. On systemic examination, CVS: S1 S2 heard, no murmur, RS: B/L AE +, CNS: moving all 4 limbs, PA: soft, non tender. On local examination, on inspection- flexed position of neck noted, mild neck tenderness +, no lymph node palpable. Throat and ear could not be assessed as the patient was not cooperative. VBG and x-ray neck done were normal. Patient was advised for basic blood workup, and the flu panel was negative.
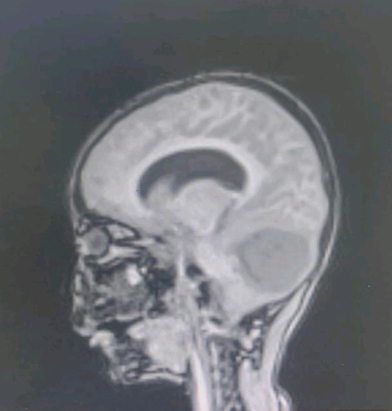
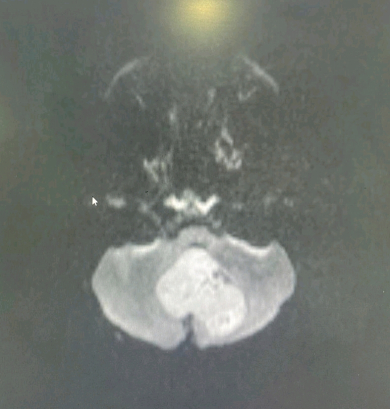
Treatment with crystalloids, analgesics, antacids and antiemetics were started and admitted in ward with stable vitals. MRI brain with neck was done the next day as there wasn’t improvement in the presentation. It showed posterior fossa tumour with obstructive hydrocephalus. Patient was immediately shifted to ICU for ICP management. Patient was shifted to vadapalani kauvery the next day, total tumour excision done. Post op patient was extubated, neurologically intact. On day 3 patient was mobilised. HPE reports suggestive of medulloblastoma. Suture removal done and is planned for radiation therapy within 3weeks.
CASE DISCUSSION:
In a child presenting with such not so alarming but uncommon symptoms, close follow up would help to prevent us from missing such a serious diagnosis.
Medulloblastoma is the most common malignant brain tumor in children constituting nearly 20% of all pediatric brain tumors. It is categorized as an embryonal neuroepithelial tumor of the cerebellum. This is a high-grade tumor that has a tendency to spread via the cerebrospinal fluid.
Within the first few years of diagnosis, mortality approximates 15%; however, cure rates can reach as high as 60% with current therapeutic modalities. Surgical resection preceded and/or followed by radiation and chemotherapy is the mainstay of therapy, with five-year survival rates of between 50% to 90%. This wide range is multifactorial, owing in part to age at diagnosis, the presence of metastases at diagnosis, and histologic variants of medulloblastoma.
Children age 4 to 9 years old has the highest incidence at 44%, followed by adolescents (10 to 16 years old) at 23%, and only a 12% incidence in infants/toddlers (0 to 3 years old). Medulloblastoma affected males 1.5 times more than females.
The diagnosis and management of medulloblastoma are best done by an multidisciplinary team that consisting of pediatrician, neurologist, neurosurgeon, oncologist, radiation therapist, and specialty trained nurses. The majority of children first present with cerebellar symptoms. Mental health professionals involvement is vital as many patients develop depression and anxiety.
REFERENCES:
- Rossi A, Caracciolo V, Russo G, Reiss K, Giordano A. Medulloblastoma: from molecular pathology to therapy. Clin Cancer Res. 2008 Feb 15;14(4):971-6.
- Pfister S, Remke M, Benner A, Mendrzyk F, Toedt G, Felsberg J, Wittmann A, Devens F, Gerber NU, Joos S, Kulozik A, Reifenberger G, Rutkowski S, Wiestler OD, Radlwimmer B, Scheurlen W, Lichter P, Korshunov A. Outcome prediction in pediatric medulloblastoma based on DNA copy-number aberrations of chromosomes 6q and 17q and the MYC and MYCN loci. J Clin Oncol. 2009 Apr 01;27(10):1627-36.
- Wu X, Northcott PA, Croul S, Taylor MD. Mouse models of medulloblastoma. Chin J Cancer. 2011 Jul;30(7):442-9.
- Huse JT, Holland EC. Genetically engineered mouse models of brain cancer and the promise of preclinical testing. Brain Pathol. 2009 Jan;19(1):132-43.
- Smoll NR, Drummond KJ. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci. 2012 Nov;19(11):1541-4.
- Taylor MD, Northcott PA, Korshunov A, Remke M, Cho YJ, Clifford SC, Eberhart CG, Parsons DW, Rutkowski S, Gajjar A, Ellison DW, Lichter P, Gilbertson RJ, Pomeroy SL, Kool M, Pfister SM. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol.
 Dr. Vaishnavi
Dr. Vaishnavi
Emergency Medicine Resident,
Department of Emergency Medicine,
Kauvery Hospital- Alwarpet
 Dr. Ashok Nandagopal
Dr. Ashok Nandagopal
Clinical Lead & Consultant,
Department of Emergency Medicine,
Kauvery Hospital- Alwarpet