Case presentation
A 66-year-old lady presented to our emergency department with the following complaints:
- Decreased sensorium and drowsiness for 2 days
- Decreased oral intake for 2 days
Presenting illness
- Patient presented with the complaints of altered sensorium and drowsiness for the past 2 days (since 14/5/21), sudden in onset and gradually progressive to the current state.
- H/O decreased food intake for 2 days.
- No H/O head injury, vomiting, trauma, headache, neck stiffness, blurring of vision, limb weakness, bowel & bladder incontinence, fever, cough, cold, and loss of weight.
Recent past medical and surgical history
- k/c/o acute pyelonephritis for which she underwent cystoscopy with B/L. DJ stenting was done on 12/3/2021 (outside hospital).
- Recent Covid pneumonia as on 16/4/2021. Home isolation is managed with steroids. CT severity score is 10/25 (done outside hospital)
- Urinary tract infection was there as on 1st week of May, and urine culture done showed E-coli was left untreated.
The patient is a known case of having diabetes, hypertension, coronary artery disease, and chronic kidney disease on medical management with a baseline keratinize of 2.1 mg/dl. She has also hypothyroid.
Initially at ER
General examination
– Patient conscious, drowsy, arousable
– Pallor present
– No icterus/clubbing/cynosis/lymphadenopathy/edema.
– Vitals: HR: 116/min, BP: 110/60mmg, SPO2: 100%RA, RR:30/min
Local examination:
– Facial puffiness + lip edema
– Oral cavity : teeth stained, crusting + , foul smelling(halitosis)+
Systemic examination
I. Respiratory system: B/L air entry decreased, B/L crepts +
II. Cardiovascular system: S1, S2 +, no murmer, JVP normal
III. Abdomen: soft, non-tender, no organomegaly, BS +
IV. Central nervous system: GCS- E2V2M5, no deficit
Initial investigations and workup
ECG: sinus tachycardia
ABG: showed high anion gap metabolic acidosis with compensation

Serology: NEGATIVE
Urine routine: Turbid, pus cells: 10-12, u.protein: +, u.blood: ++, ketone : negative, crystal and cast : nil
Blood culture: no growth
Urine culture: GNB: E-coli
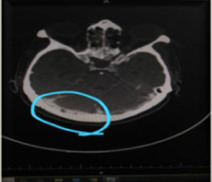
CT brain: age-related atrophy
CT chest: patchy GGO in b/l peripheral subpleural location s/o atypical infection CORADS- 5 – severity score: 14/25
CT – KUB: no significant abnormality
ECHO : conc LVH, normal RV &LV EF-60%, no RWMA, mild PAH—EEG: no epileptic features
Primarily, the case was treated based on the initial investigation as urosepsis with acute kidney on chronic kidney injury and was started on IV antibiotics, PPI. Hemodialysis was done at the ICU stay. Initial CT brain and KUB were normal. Subsequently, on day 3 of hospitalization, sepsis improved, and kidney injury was also resolving with hemodialysis, but there was no improvement in her GCS, which was still deteriorating. Hence, the patient was put on NIV as she was tachypneic and tachycardiac. She was continued with broad-spectrum IV antibiotics. In view of unexplained drop in GCS despite treatment, the patient underwent an MRI brain with MRA.
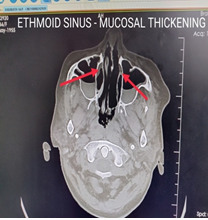
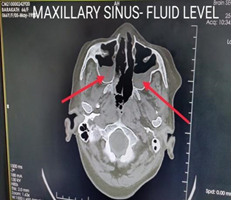
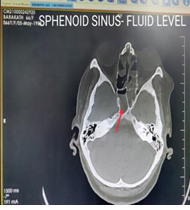
– MRI brain with MRA: Acute infarcts were found in the right medial thalamus, mammilary body, and parietal region. There was an ill-defined soft tissue in the right temporal region adjacent to the sphenoid sinus assoc with narrowing of the distal cavernous and supraclinoid segment of right ICA . Pansinusitis. Suggested contrast to r/o cerebral abscess.
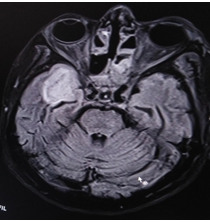
MRI BRAIN – FLAIR- INFARCT INVOLVING TEMPORAL LOBE
MRI BRAIN WITH MRA- DWI- ACUTE INFARCT
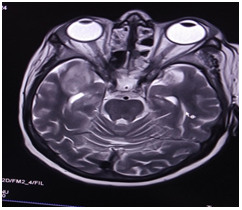
MRI BRAIN – T2WI
And now, turning our case towards “infarcts”, giving a spark would be because of paroyxsmal atrial fibrillation, creating an embolic infarct! So started on anticoagulants and antiplatelet after consulting with neuro team and waiting for a change to happen.
As the case required further work, CT BRAIN with contrast was taken after getting clearance from the Nephro team. CT brain with contrast showed the following:
CT brain with contrast: Acute infarct in the right gangliocapsular region. cavernous sinus thrombosis. pansinusitis. Right temporal lobe abscess with extension into right orbit.
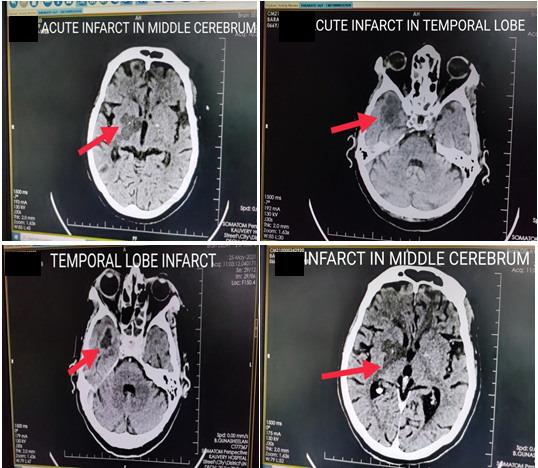
CAVERNOUS SINUS THROMBOSISPANSINUSITIS :
In order to probe into the definitive cause, the case was discussed with ENT team and planned for endoscopy. It was planned for surgical debridement also.
Diagnostic nasal endoscopy and biopsy: Black necrotic material++ (thick eschar) was noted involving the inferior and middle turbinate. Extensive disease was noted involving the bilateral ethmoids. Multiple tissues were taken and sent for fungal culture and biopsy.
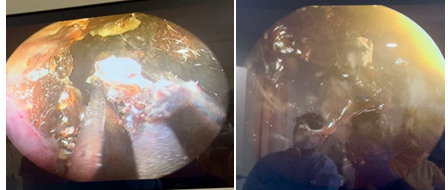
Black necrotic thick eschar, biopsy is taken
Extensive disease involving inferior and middle turbinate
- Now taking us to the second year of MBBS after having a look at that grow in the culture.
Culture growth of mucormycosis in sabouraud dextrose agar
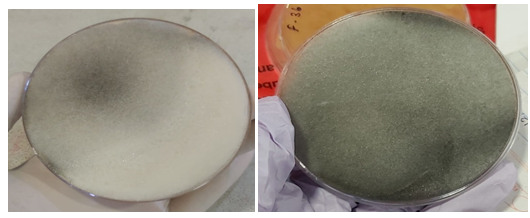
Day 1 24 hours growth
40-hours growth with 48 hours AT 25 Degree Celsius
Microscopic view
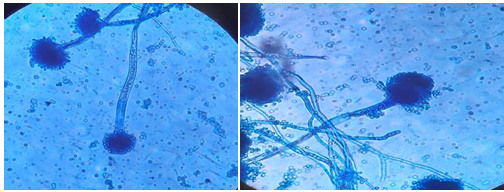
Microscopic view of rhizopus oryzae–showing hyphae with spores in 40xfocus
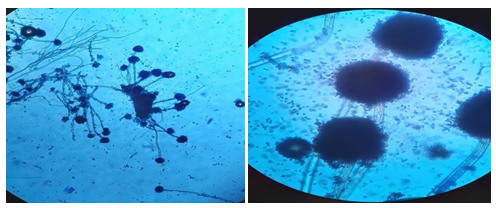
View in 100x focus Rhizopus species
The patient was finally diagnosed with rhinocerebral mucormycosis, first case in our hospital. The patient continued to deteriorate and was eventually on inotropic support. Despite all aggressive measures, she succumbed to the disease.
Discussion
A complex interaction of factors comprising preexisting diseases, such as diabetes, hypertension, use of immunosuppressive therapy, and systemic immune alterations of COVID-19 infection itself, may lead to the secondary infections, which are prominently being recognized in view of their impact on morbidity and mortality.
Mucormycosis is generally a group of uncommon infection caused by a fungus, but now it is becoming a common diagnosis in post-covid patients. Mucormycosis is an invasive fungal infection once called as zygomycosis, but the organisms that causes the infection, specific types of molds, have been scientifically reclassified, and the term mucormycosis came later. These infections are broken down into 5 presentations: rhinocerebellar, pulmonary, cutaneous, gastrointestinal, and disseminated.
The most common presentation is a sinus infection. In this case, the infection spreads outside the sinuses, causing necrosis of the roof of the mouth, involving the septum and turbinates, and spreads to brain. This can cause altered consciousness, lethargy, seizures, partial paralysis, neuropathies, brain abscess, and coma.
When the infection spreads to the eyes, there can be swelling, proptosis, vision loss, and potential blindness. In some individuals, there could be ophthalmoplegia, making it difficult or painful to open the eyes.
This was a challenging diagnosis because symptoms were common to many other conditions.
When to suspect and warning signs and symptoms:
- Sinusitis- nasal stuffiness/erythematous nasal mucosa, nasal discharge (bloody/blackish), local pain on cheek bone, epistaxis, loss of smell.
- One-sided facial pain, numbness/paresthesia, or swelling,
- Halitosis, tooth ache, loosening of teeth, jaw involvement, palatal ulceration.
- Eyelid edema, orbital pain, eyelid ptosis, protruding eyes, ocular mobility restrictions, double vision, and sudden vision loss
- Fever, headache, cough, shortness of breath, altered mental state, thrombosis, and necrosis (eschar formation).
- Chest pain , pleural effusion, haemoptysis
Conclusion:
This is a case of unusual presentation of rapidly developing a fungal infection in a patient with pre-existing co-morbidities in the background of COVID-19.
Increase in mucormycosis in the Indian context appears to be an intersection of diabetes (high prevelance), rampant use of corticosteroids (increases the blood sugar level and opportunistic fungal infections), COVID-19 (lymphopenia, endothelial damage, cytokine storm), and contaminated oxygen equipment.
Learning points
- An effective teamwork is an essential tool for constructing a more effective and patient-centered health care delivery system (emergency physicians, internal medicine specialist, intensivist, ENT specialist, neurologist, ophthalmologist, microbiologist, dentist, and surgeon).
- Statistical analysis has proven that steroids drugs are useful in reducing mortality in COVID-19 patients with low oxygen saturation levels. Steroids reduce inflammation; however, they can negatively affect your ability to fight infection. “An important thing is using it wisely and timely”.
- Early diagnosis and treatment of mucormycosis that consist of antifungal therapy and surgical debridement are important to reduce mortality and prevent the end-organ damage.
- Use clean, sterile water for humidifiers during oxygen therapy
- Do not consider all the cases as bacterial sinusitis, particularly in the context of immunosupression and/or COVID-19 patients on immunomodulators
- Do not hesitate to seek investigations as appropriate, such as KOH staining and microscopy and cultures for detecting fungal etiology.
- The vaccine for COVID-19 will not give you COVID-19- Get vaccinated.
 Dr. Niveda R
Dr. Niveda R
Resident 1st Year – Dept. of Emergency Medicine
Kauvery Hospital Chennai



