Case presentation
A 65-year-old lady was brought with sudden onset of drowsiness associated with breathing difficulty and increased frequency of urination since the morning of 3\6\2021. The attendant saw her normal at 11:30pm on 2\6\2021
- No H/o fever, cough, vomiting, loose stools, trauma, head injury, chest pain, palpitation, sweating, seizure,
- H/o covishield vaccination 2nd dose completed on May 2021
- Past medical history : The patient is a known hypertension and dyslipidemia case
On examination:
- The patient was drowsy, arousable, febrile, dehydrated ++. Tachypneic
- A – Threatened, noisy breathing,
- B – B/L AE + B/L basal crepts + , conducted sounds +, RR – 32, Spo2 – 88% RA
- C – B/L PPWF + , CVS – S1S2 + ,HR – 92, BP – 100/60,
- D – E3V2M4 ,B/L pupils pin point (1mm), moving all 4 limbs
- E – Temp – 100.6’F
Bedside investigation done

- Sinus rhythm
- Rate – 100 bts/min
- Normal axis
- No acute st-t changes
Echo
- Sclerotic aortic valve
- Mild AR/ trivial MR
- Mild TR /PAH (PASH – 48mmhg)
- Normal RV function
- No RWMA
- Good LV systolic function (EF – 60%)
- Reduced diastolic compliance

Regular medication
- – Zolfresh 10mg HS
- – Cilacar 10mg BD
- – Metosartan 50mg OD
- – Nexito plus OD
- – Rozavel 10mg HS
Provisional diagnosis
- Probably sespsis with septic shock -> lung source? Pneumonia vs seizure disorder
- AKI
Further investigations revealed the following:
- CBC – Leucocytosis with neutrophilia and lymphophenia (TC – 11800, N79.5, L120)
- Low normal platelets at 1.68 lakhs
- Normal RFT and LFT
- Mildly elevated CRP – 6.02
- Elevated D-Dimer – 1800
- Normal procalcitonin – 0.78
- Urine routine – WNL
- Urine toxicology screen +ve (positive) for Benzodiazepine
- RT PCR Covid swab test – Negative
CT brain
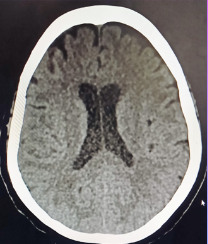
- Chronic lacunar infarct in the right thalamus
- Small vessel ischemic changes
CT abdomen

- Fatty liver
- B/L small-sized kidneys with cortical scars
- Right adnexal cyst
CT chest

- Mild cardimegaly with pericardial thickening and bilateral mild pleural effusion
- Subtle subpleural ground glass attenuation with interlobular septal thickening in left upper lobe anterior segment
- Areas of consolidation with air bronchogram in the right upper and middle lobe
- Consolidation with branchogram and surrounding ground glass opacities in the right lower lobe superior and medical segment in the central perihilar location – R/O neoplastic ethology
Suspicion
In suspicion of exact reason for drowsiness, hypotension, desaturation, which was unexplained by lab investigations and clinical finding, attenders were probed again deeply in regard to drug history.

- We had a suspicion of drug overdose -> advised attendants to go back and see tablet box
- Patient apparently was on tab. – ZOLFRESH 10MG OD
- The attendants later went through the patient’s medicine box to see all tablets are missing from the 2 strips of Zolfresh 10 mg, each containing 12 tabs which were brought just 2 days ago
Management
- Inj – Paracetamol 1gm iv stat -> in v/o fever
- Inj – Pan 40mg iv stat
- Inj – Emeset 4mg iv stat
- Ivf – ns 500ml bonus -> in v/o bp 100/60 (in v/o hypotension) repeat bp 110/60
- Inj – magnex forte 3gm iv stat
- Ryle’s tube insertion -> with continuous aspiration
- Foley’s 16 size catheterization done -> clear urine drained 150ml
- All supportive measures were taken, and the patient was admitted to ICU for further neuro-observation of vitals.
- This patient recovered with supportive measures and symptomatic treatment and was discharged after 5 days of hospital stay and obtaining psychiatric counseling
Discussion
Clinical features of benzodiazepines overdosage
- Rapid with most developing symptoms within 4 hours
- Patient initially present with mild-to-moderate impairment of CNS function.
- Severe overdose can lead to prolonged deep coma, apnea, respiratory depression, hypothermia, Brady cardia, cardiac arrest, pulmonary aspiration,
- Drowsiness
- Dizziness
- Ataxia
- Dysarthria
- Confusion
- Hypotension
Toxicity
- Benzodiazepines have a wide therapeutic index and taken alone in overdose rarely cause severe complications or fatalities
- Taken in overdose in combinations with alcohol, opioids, tricycles antidepressants are particularly dangerous
- Elderly and those chronic illness are much more vulnerable to lethal overdose with benzodiazepines
Benzodiazepines antogonist –> flumazenil
Indications
- Reversal of benzodiazepines sedation
- Benzodiazepines toxicity
Contraindications
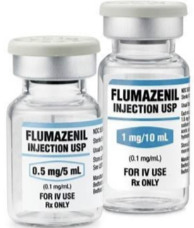
- Known seizure disorder
- Overdose of unknown agents
- Suspected or known physical dependence on benzodiazepines
- Suspected cyclic antidepressants overdose
- Suspected increased intracranial pressure
- Co – ingestion of seizure inducing agents
- Flumazenil is a benzodiazepines receptor antagonist that can be used as an antidote for benzodiazepines overdose
- Specific antagonist for benzodiapines -> flumazenil at 0.2mg / min maximum dose of 3g/h, but it may precipitate seizures and intracranial pressure.
- Flumazenil should be avoided if the patient is dependent on benzodiazepines or takes tricyclic antidepressants as it can precipitate withdrawal syndrome and cardiac arrest
- Oral bioavailability is very less ->not used orally
- I/V injection action starts within seconds and lasts for 1-2hrs
- It also has no role in the management of unknown overdose
- In addition, if full airway protection has been achieved, a good outcome is expected and therefore flumazenil is unlikely to be required (GCS)
- It is very effective at reversing the CNS depression associated with benzodiazepines but less effective in respiratory depression
- It has short half life, and duration of action of flumazenil is less than 1 hour
Take-home points
- An incomplete history which does not corroborate all the clinical signs and symptoms should push us to go back and retake the history.
- If clinical situations like mentioned above should arise, we should suspect drug overdose.
 Dr. Noor Akbar
Dr. Noor Akbar
MRCEM Resident – Dept. of Emergency Medicine
Kauvery Hospital, Chennai