Abstract:
- Anaphylaxis is a severe, potentially life-threatening allergic reaction. The most common anaphylactic reactions are to foods (peanut, sea foods), insect stings, medications and latex.
- Anaphylactic shock cases are rare but life-threatening, with its incidence rate of 1.5-7.9 per 100,000 people.
- Acute myocardial injury or infarction in the setting of an anaphylaxis can be due the anaphylaxis itself, when it is known as Kounis Syndrome
Case report
28 years aged gentleman, with no comorbids and no known drug allergy, presented to ER with history of consumption of sea food the previous day following which he had noticed small eruptive rashes with itching over his body while bathing the next day. After bathing, he had a episode of giddiness and fall – sustained injury to his face and was brought to us for further management.
On initial evaluation at ED
Airway
Patent, self maintained. C-spine clinically cleared.
Breathing
RR – 22/ min, Spo2 – 99% RA, B/L air entry equal, no added breath sounds.
Circulation
BP – not recordable. HR – 92/ min,
CVS – S1S2 normal, no murmur, JVP – Normal, cold and clammy peripheries, peripheral pulses feebly felt.
PA – Soft, non-tender, no organomegaly, and bowel sounds heard.
Disability
GCS – E4V5M6 [15/ 15]
B/L pupils equally reacting to light 3mm
Moving all 4 limbs
CBG – 199mg/dl
Exposure
- Active rigors noted.
Local examination of face
- 3×5 cm laceration over nasal bridge just below glabella.
- 1x1cm laceration over mucosal aspect of upper lip.
- Active bleed noted.
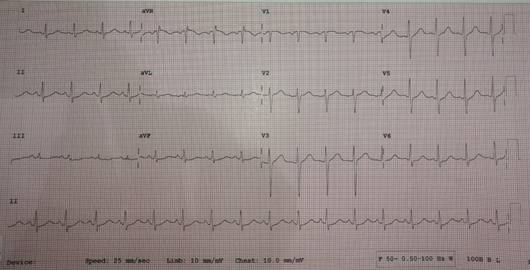
ECG
- Rate 110/ min
- Sinus rhythm
- Normal Axis
- No other specific ST – T Changes
ABG( RA)
pH – 7.32
PCO2 – 41.3 mmHg
PO2 – 91 mmHg
BE – -5 mmol/ L
HCO3 – 21.4 mmol/ L
SO2 – 96%
LAC – 4.11 mmol/ L
CHEM – 8
Na+ – 142 mmol/ L
K+ – 3.0 mmol / L
Cl – – 104 mmol/ L
ica – 1.14 mmol/ L
GLU – 164 mg/ dl
BUN – 20 mg/ dl
CREAT – 1.0 mg/ dl
HCT – 46% PCV
HB – 15.3 g/ dl
TROP-I:
0.10(positive)
ECHO:
Normal sized cardiac chambers
No regional wall motion abnormality
Normal LV systolic function (EF-65%)
MANAGEMENT IN ER:
In view of profound anaphylactic shock, leg end elevation done was done and quickly secured 2 wide bore intravenous cannula.
In view of severe anaphylaxis with shock – Intramuscular adrenaline 0.5ml (1:1000 dilution) given every 5 mins (totally 3 doses given) and IV fluids (NS) about 2 litres given as bolus.
Additionally intravenous hydrocortisone 200mg + chlorpheniramine 10mg + pantoprazole 40mg given.
Lacerated wounds sutured under local anesthesia and hemostasis secured.
For accurate measurement of blood pressure, arterial line secured.
Our initial diagnosis was anaphylaxis with refractory anaphylactic shock.
But with significant elevation in troponin levels, raised a doubt of acute coronary syndrome secondary to anaphylactic shock (? Type-1 Kounis Syndrome).
After stabilization, patient shifted to ICU for further management.
Blood investigations
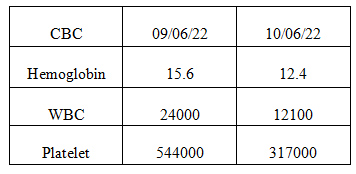
Follow up:
- Cardiologist opinion obtained and serial TROPONIN-I was negative. No recurrence of symptoms noted and patient discharged after 2 days with oral steroids, H2 receptor blocker, anti-histamine and anti-biotics.
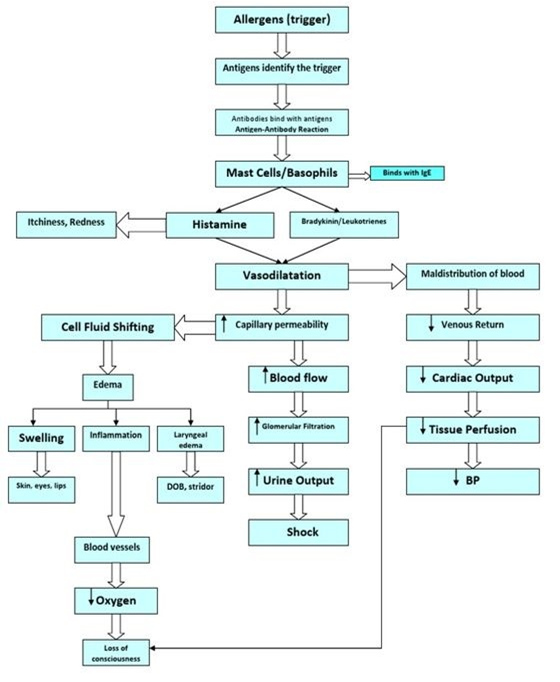
Pathophysiology of Anaphylactic shock:
Discussion:
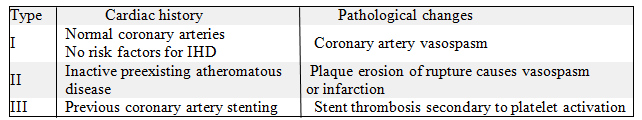
Anaphylaxis is an acute, potentially fatal medical emergency. The acute treatment of anaphylaxis is epinephrine. Myocardial injury or infarction in the setting of an anaphylaxis can be due the anaphylaxis itself, when it is known as Kounis syndrome or it can also be due to the effect of epinephrine treatme Epinephrine may cause coronary vasoconstriction, reduce coronary blood flow, increase myocardial oxygen demand, and worsen myocardial ischemia. Acute coronary syndrome accompanying mast cell activation from allergic, hypersensitivity, or anaphylactoid reactions was first described by Kounis and Zavras in 1991 and has been referred to as “allergic angina” or “allergic myocardial infarction”. Mast cells play a central role in hypersensitivity reactions, and they are necessary for the development of allergic reactions. Mast cells are activated either by IgE-bound antigen cross-linking, anaphylotoxins (C3a and C5a) or a variety of stimuli. Their activation leads to degranulation of preformed inflammatory mediators (e.g. histamine, tryptase, chymase, heparin), increased production of arachidonic acid-derived mediators (e.g. prostaglandin D2, leukotrienes B4 and C4). This leads to coronary artery vasospasm and/or atheromatous plaque erosion or rupture. Overall prevalence of Kounis Syndrome is 1.1% of patient with anaphylaxis and 7% mortality rate of reported cases. Morphine must be avoided in Kounis Syndrome as it may stimulate histamine release and exacerbate mast-cell induced vasospasm. The types of Kounis Syndrome are listed below.
Conclusion:
Kounis Syndrome is not uncommon but can be easily missed. Timely interpretation and prompt action in anaphylaxis with shock is lifesaving. The use of epinephrine for anaphylactic shock is lifesaving but physicians must be aware of this complication even in patients without risk factors or history of coronary artery disease.
ACKNOWLEDGEMENT:
For guiding me with the article, I would like to thank,
Dr.Aslesha (Clinical lead – emergency department)
Dr.Niveanthini (Consultant – emergency department)
“The author declares no conflict of interest”
REFERENCE
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45(2):121–128.
- Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol. 2006;110(1):7–14.
- Kounis NG. Kounis NG. Clin Ther. 2013 May;35(5):563-71. doi: 10.1016/j.clinthera.2013.02.022. Epub 2013 Mar 13. Clin Ther. 2013. PMID: 23490289 Review.
- Kogias JS, Sideris SK, Anifadis SK. Kogias JS, et al. Int J Cardiol. 2007 Jan 8;114(2):252-5. doi: 10.1016/j.ijcard.2005.11.059. Epub 2006 May 2. Int J Cardiol. 2007. PMID: 16647768
- Vigorito C, Poto S, Picotti GB, Triggiani M, Marone G. Effect of activation of the H1 receptor on coronary hemodynamics in man. Circulation. 1986;73(6):1175–1182.
 Dr. Silvera Samson Raj
Dr. Silvera Samson Raj
2nd Year MRCEM Resident
Department of Emergency Medicine
Kauvery Hospital, Chennai