Professor Dr Thameem Ansari, during his earlier days, was working in all the three city medical colleges and Institute of Child Health and Hospital for Children, Madras. He worked abroad for over three decades as the Head of Pediatric Surgery in Penang Malaysia, Head of Surgery and Allied Departments in Penang Adventist Hospital and continued for two decades. He was appointed as the Head of the Medical Education Committee, M and M Committee, Surgical Care Review Committee and Patient Care Review Committee. Dr Ansari has published two books in pediatric surgery and one on neonatal problems – diagnosis and management. The second book with 1000 color palettes titled as “Diagnostic Picture Aid in Pediatric Surgery with Q and A” was published in Malaysia. Dr Ansari is a peer reviewer for Medical Journal of Malaysia and was given “Best Reviewer Life Time Achievement Award” with citation and cash award as token of appreciation. Prof. Dr Ansari was also former Adjunct Prof. of Pediatric Surgery, AIMST University – Malaysia and Prof. of Pediatric Surgery, AUCMS University, Penang, Malaysia. Dr Ansari has done over 40000 surgical procedures in children (minor, major, cold and emergency cases) with excellent results. Dr Ansari has presented and published in lead journals – Journal of Gut and Hepatology, Journal of Asianic Ocean, Journal of Radiology, Hospital Pulau Penang Journal, Journal of Pediatric Surgery, etc. 200 scientific papers in India, Nepal, Korea, Hong Kong, Singapore, Malaysia, Libya, Jordan, Paris, Holland, etc. Dr Ansari had his advanced training in GI motility lab in Sweden, Singapore (esophageal pH metry, EM, electro gastrography, anal manometry, pelvic floor training, bio feedback training to overcome fecal incontinence, colon transit study, manometry aided cine defeco graph, etc.) and laparoscope training in Germany and in USA. Dr Ansari was Director of Digestive Function Center (private) Penang, Malaysia. Dr Ansari did his PillCam endoscope training in Florida, USA and started PillCam endoscopy services in Malaysia from 2005 onwards.
Prolonged Jaundice in Children – Diagnosis and Management
Introduction:
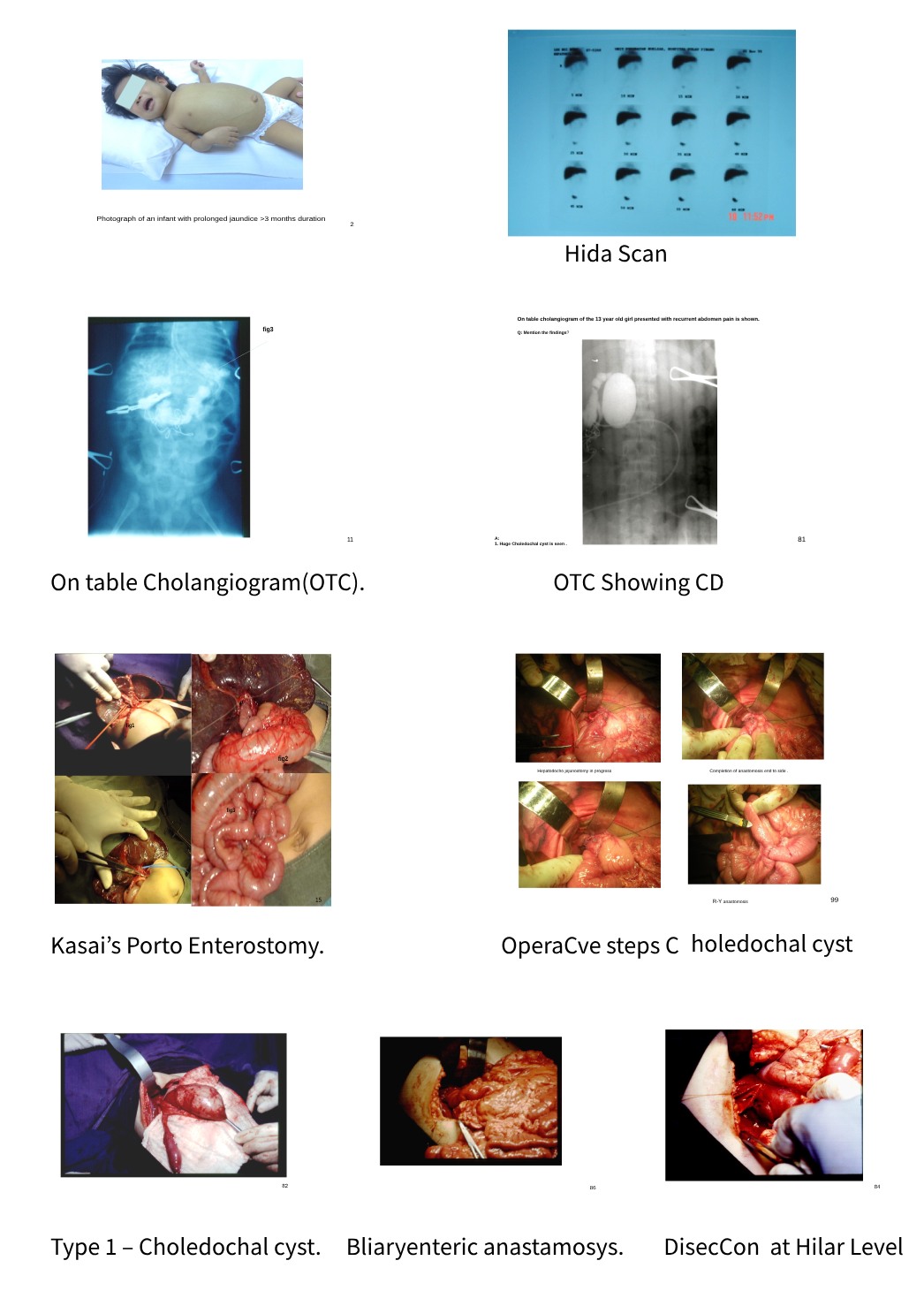
Prolonged jaundice is defined as jaundice lasting for more than 14 days of life in full-term infants. Etiologically, it has to be distinguished between obstructive jaundice and jaundice due to medical causes. Serum bilirubin (SB) > 5mg/dl or 85 Mmol/L in term infants, 14 days after birth and 21 days after birth in preterm babies. Jaundice affects 2 to 15% of all new born (NB) babies and 40% of breast-fed babies (BF). Prolonged jaundice after 28 days of life must be viewed with suspicion of cholestatic jaundice (obstructive jaundice) until proved otherwise. I am presenting my personal experience in management of jaundice due to surgical causes – a. biliary atresia b. biliary hypoplasia c. inspissated bile plug syndrome d. idiopathic perforation of bile duct e. congenital choledochal cyst, primary sclerosing cholangitis, etc. Jaundice in children, some are life-threatening and some are self-limiting. This article aims to provide a concise review of surgical causes in children and discusses the diagnosis and management as well as provides a brief description of jaundice due to medical causes.
Index words: Jaundice/Surgical Causes/Management
The causes for prolonged jaundice could be 1. pre-hepatic 2. hepatic 3. post-hepatic causes. Hemolytic jaundice, breast milk jaundice, G6Pd deficiency Gilbert syndrome, viral hepatitis, hepatotoxic drugs consumed (Chinese herbal medicine)
In my personal series, I have operated more than 300 neonates and older children with various causes for prolonged jaundice in India, Libya and in Malaysia. Biliary atresia (around 150 neonates and infants), congenital choledochal cyst (100 cases of my personal series) the other causative factors such as a. inspissated bile syndrome b. intrahepatic hypoplasia c. Caroli’s disease d. idiopathic perforation of CBD are relatively rare e. Primary sclerosing cholangitis in an African (Chad) child. Surgical disease refers to obstructive and impaired biliary drainage. It is differentiated from medical causes by measurement of the level of SB (split bilirubin direct and indirect level); elevated direct bilirubin level is suggestive of cholestatic jaundice and elevated indirect bilirubin is suggestive of largely medical causes which include infantile hyper trophic pyloric stenosis, the pyloric tumor causes extraneous compression of bile duct.
Management is surgery which varies from minor to ultra-major procedures. Neonates or infants and older children with jaundice present with icterus, yellowish discoloration of skin, pale stool, high-colored urine, lethargy, increased sleepiness, poor feeding, high pitched crying and vomiting, etc. Incidence of BA (biliary atresia) is 1 in 5000 to 1 in 18000 in Caucasians. Associated anomalies do occur in BA and have to be looked for. BA is characterized by inflammatory sclerosing cholangiopathy which starts prenatally due to maternal viral infection, genetic predisposition along with exogenous factors triggering inflammatory events during embryonic or perinatal period. BA is not due to genetic factors alone and few other factors are associated with the disease.
Affected children with BA present with progressive jaundice, skin discoloration, icteric, itching, pale stool and dark high colored urine; liver and spleen will be palpably enlarged (cirrhosis sooner or later will set in).
Investigations:
Full blood picture is done to rule out hematological causes. Serum bilirubin (SB) total value and split value for direct and indirect level. Elevated direct bilirubin indicates cholestatic jaundice and needs further diagnostic evaluation which includes ultrasound and HIDA scan. Ultrasound will reveal contracted gall bladder and no evidence of bile ducts with or without changes in the liver (depend on early referral 28 days of life or delayed beyond a month or two). In early referral, the bile flow will be good since fibrosis of the duct is not complete. HIDA scan will show the dye in intrahepatic radicals as well as in to duodenum if patent, if not seen then per operative cholangiogram is done either laparoscopically or through right subcostal small incision and keep in view for Kasai’sportoenterostomy (prior consent is obtained). Following surgery, effective clearance of jaundice and improved LFT was noted in my series 33% to 40% approximately and another 33% lived with jaundice and supportive therapy; the rest 30% were outright failure.
Post-operatively infants may get recurrent cholangitis, fever, deepening jaundice and may need antibiotics and steroids, may drain good quality of bile seen through the stool chart and SB level will come down. If not, they will progress to hypersplenism, portal hypertension, pancytopenia, bleeding varices, etc. and will need appropriate care. The success of surgery depends on timing of surgery (early cases after 28 days surgical referral and in the meantime work up is done for Kasai’s). Progressive cases may need liver transplantation.
Inspissated Bile Syndrome: Due to prematurity, cystic fibrosis and prolonged TPN or fluconazole drug, is one of the risk factors. The affected child presents feature suggestive of obstructive jaundice, ultrasound will reveal the biliary sludge, dilated bile duct. Mild cases get cleared with hydration and urso deoxycholic acid therapy. Severe cases could lead to cirrhosis liver following liver damage and may need Kasai’s portoenterostomy after routine investigations done as for BA cases.
Choledochal Cyst:
It is defined as cystic dilatation of CBD due to distal obstruction congenital weakness of the wall of bile duct, anomalous pancreaticobiliary junction (APBJ) and reflux of pancreatic juice in to biliary tree causing damage to bile ducts and dilatation occurs are the important causes. Congenital choledochal cyst (CD) occurs in 1 in 10000 live births and seen in Chinese descent in Asian population (my own experience confirmed this in Malaysia). CD could be diagnosed even prenatally and also seen in adults (from NB to adults) and present with recurrent abdominal pain in older children, missed as functional abdominal pain in my series. CD are of five types and type
Type 1. A cyst of extra hepatic bile duct accounting to 90% in my series.
Type 2: Choledochal diverticulum
Type 3: Choledochocele inside wall of duodenum
Type 4: Both intra hepatic and extra hepatic duct dilatation
Type 5: Caroli’s disease (multiple intrahepatic cysts
Investigations and Management:
1. Plain x-ray abdomen ( soft tissue impression will be seen below right hypochondrium)
2. MRCP
3. Per-operative cholangiogram to study the details of anatomical relationship
4. Surgery – Laparoscopically vs. open laparotomy (I did all open laparotomy)
Procedure: Total cystectomy, cholecystectomy, hepatico-docho jejunostomy, Roux en Y anastomosis followed by liver biopsy and appendicectomy (with informed consent)
5. Post-operatively, long-term follow-up advice is given to parents (cholangitis
Conclusion:
Prolonged jaundice is attained a life-threatening disorder. Early referral to paediatric surgeon is mandatory if jaundice persists beyond 28 days of life. Serum bilirubin level (direct & indirect) is important. Medical causes must be ruled out for PJ. HIDA scan to find out the patency of intra & extra hepatic ductal system. If not conclusive, per operative cholangiogram has to be done, followed by liver biopsy to find out the injury to the liver as well as no paucity of bile duct (rules out Alagille syndrome). Careful antenatal history and perinatal history, metabolic screening medications history. Increase of parenchymal enzyme aspartate aminotransferase & alanine aminotransferase suggestive of liver injury due to virus or drug induced or auto immune. In obstructive jaundice, increase level of ductal enzyme alkaline phosphatase, gamma glutamyl transpeptidase is seen. Ultrasound of abdomen (hepatobiliary tree & liver).Liver transplantation has given a new ray of hope to these unfortunate infants.

Prof. Dr Thameem Ansari
MBBS, MS (Gen), M.Ch (Pediatric Surgery), FICS (Ped.Surgery)
Senior Consultant Pediatric and Neonatal surgeon,
Kauvery Hospital, Chennai. Professor of Faculty of Medicine
Lincoln University College, Malaysia
Adjunct Professor of Pediatric Surgery, MGMCH – Pondicherry
Visiting Consultant Pediatric Surgeon, Penang, Malaysia



