The novel coronavirus (COVID-19) infection caused by SARS -COV-2, which originated from the Wuhan city, China ,in December 2019, soon spread across to the other continents, and World Health Organization (WHO) declared it a pandemic on 11 March 2020
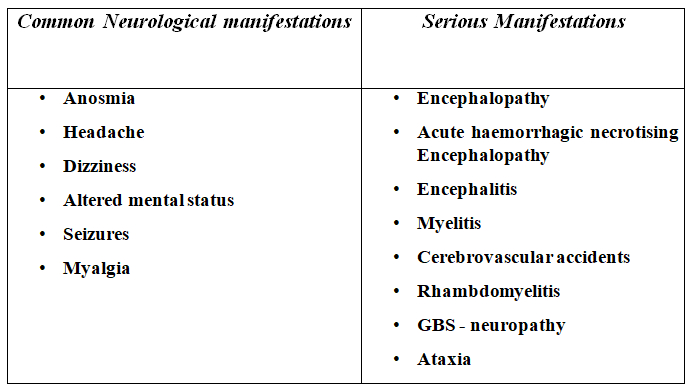
This virus causes primarily a respiratory illness, and there is emerging data on the pathogenesis and treatment protocols. However, there is also increasing evidence for various neurological complications associated with this infection. Common neurological problems include anosmia, which seems to be the heralding feature in many patients with COVID- 19 infection, headaches, dizziness, seizures, and altered mental status.
Strokes, both thrombotic and haemorrhagic, are being recognised in many patients with active COVID infection. Similarly, immune-mediated late response with necrotising encephalitis, myositis, myelitis, and neuropathies can be seen up to 6 weeks’ post- infection,
There are case reports of adult patients presenting with GBS-like phenomenon, 8-12 days’ post active infection.
This COVID-19 virus is not truly neurotropic, but there are several hypothesis regarding the pathophysiology behind CNS manifestations. We now know that this virus has an affinity to angiotensin-converting enzyme-2 receptor (ACE 2), and ACE 2 receptors are also found in glial cells in brain, spinal neurons, and in the nasal epithelium. Hence, direct entry is possible, as shown in many animal models. Secondly, at the time of the viremia phase of illness, disturbance of blood-brain barrier makes the virus to get into the brain directly.
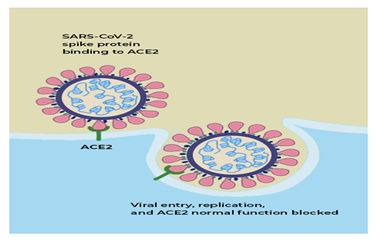
Besides, there is a postulated mechanism which is the retrograde invasion of peripheral nerve terminals done by the virus, which then enters into the CNS by means of the synapses. The elaboration of host and virus interaction is not covered in this article.
Hypoxia and CO2 retention can also be causing some of the non-specific problems such as headaches, dizziness, and altered mental state associated with COVID-19 infection.
In addition to direct infection, immune-mediated response with the endothelial injury through IL-6 and T cells, raised TNF causing coagulation cascade disruption, and extensive complement activation are strongly proposed as some of the causes for increasing CVA, especially thrombotic strokes seen in many patients with infection.
A late immune-mediated neurological manifestation, which can also be seen with many virus infections, including SARs and COVID-19, is not an exception. There are many cases of older patients who reported immune- mediated GBS-like neuropathies post-infection.
Table: COVID-19 and neurology
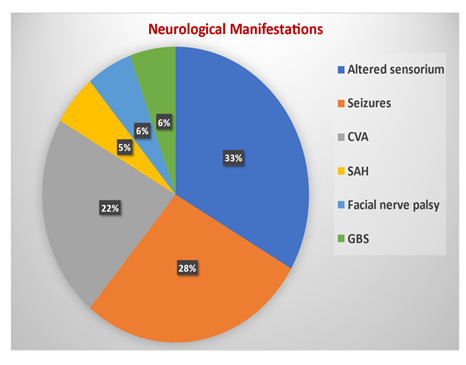
In Kauvery Hospital, Chennai, we encountered many patients treated for COVID with secondary neurological complications. Some of these patients were presented to the hospital with strokes and then found to be COVID-positive. But many of them were already being treated for COVID and later manifested neurological issues.
The strokes that we saw were not just water-shed infarcts but also large vessel thrombosis. A small proportion of patients had intra-parenchymal bleed and subarachnoid bleed. There were also patients with cortico-venous thrombosis (CVT).
In general, the problems could be categorized as:
- Complications related to coagulopathy – CVA , both thrombotic and bleed
- Complications related to encephalopathy, which includes altered sensorium, seizures, etc.
- Complications related to auto-immunity, which was seen presenting late in the post-COVID phase.
Examples of CVA:
Right MCA territory Infarct
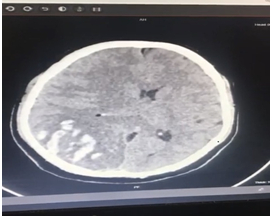
Cerebral bleed

Encephalopathy: A case report
A 72-year older man with past history of psychosis is now in remission. He is positive for COVID-19: CT changes and RT –PCR positive. As the patient was getting better, he developed severe altered sensorium and seizures. CSF was negative for sells but protein raised raised. He was treated symptomatically.
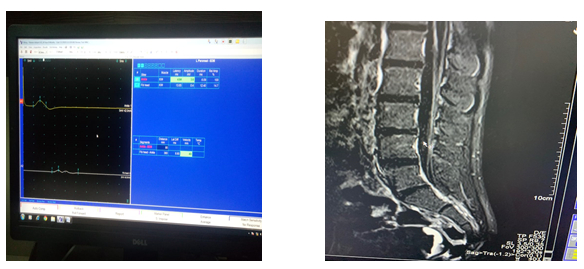
Seizure activity on EEG
GBS: A case report
A 14-year-old male with one day of fever a week ago presented with sudden onset of left lateral rectus palsy and right LMN facial palsy. He had severe ataxia and difficulty in walking. Reflexes were depressed. The condition was clinically diagnosed as Miller Fischer variant of Guillian Barre Syndrome. Nerve conduction studies and MRI spine with contrast supported the diagnosis of GBS. The patient was RT- PCR positive but had no chest symptoms. He was treated with immunoglobulins and made a remarkable recovery.
Patients who have recovered from COVID could also have some long-term issues such as:
• Chronic fatigue syndrome
• Myalgia and athralgia
• Sleep disorders
• Post-traumatic distress syndrome
• Depression
• Cognitive impairment
And these patients thus have to be monitored for long COVID syndrome, which encompasses the above signs and symptoms.
In summary, COVID-19 infection primarily affects the lungs, but neurological complications are seen in a small proportion of patients, and thus there should be a high index of suspicion.
Learning points:
• Neurological manifestations are uncommon, but there should be a high index of suspicion
• Both cytotrophic effect and immune-mediated response
• Long-term effects need to be monitored
 Dr. Bhuvaneshwari Rajendran
Dr. Bhuvaneshwari Rajendran
Senior Consultant Neurology and Neurophysiology
Kauvery Hospital



