A common encounter in ER
Case presentation:
A 75-year old lady came with c/o shortness of breath NYHA grade IV sudden onset since 12hrs, associated with reduced urine output since 1 day.
C/o generalized fatigue and tiredness since 3 days
No H/o fever, vomiting, loose stools, nausea, abdominal pain, cough, chest pain, palpitation, sweating, and altered sensorium
Past medical history:
The patient is known to have diabetes, hypertension, CAD with normal LV function with chronic AF, hypothyroid and dyslipidemia, severe PAH and OSA – on intermittent domiciliary CPAP.
On examination:
The patient was conscious, oriented, afebrile, dehydrated ++
HR – 150 / min
BP – 130/90 mmHg
RR – 30 / min
Temp – 98.4 F
GCS – 15/15
CBG – HIGH
SPO2- 91 % RA
Bilateral pitting pedal edema ++
JVP – mildly elevated
Systemic examination:
CVS : S1S2 + No murmur
JVP – elevated
RS : B/L AE + B/L basal crepts
P/A – Soft, BS + non tenderness , no organomegaly
CNS – Slightly drowsy but easily arousable (GCS – E3-4, V5, M6) NFND, moving all 4 limbs
Bedside investigations done:
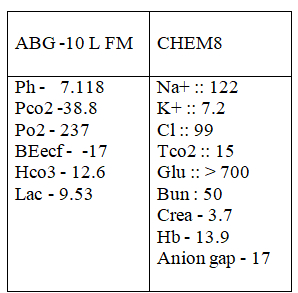
ECG:
Initial ECG:
Is this ventricular tachy arrhtyhmia or SVT with aberrancy?
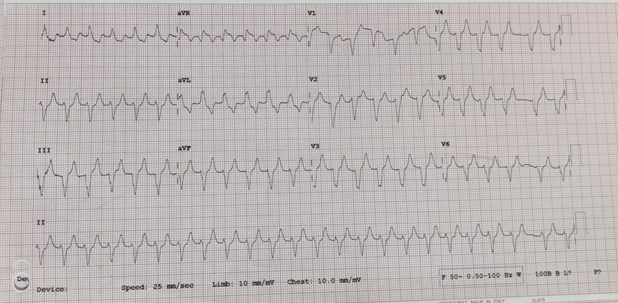
But subsequent ECG within 2 mins:
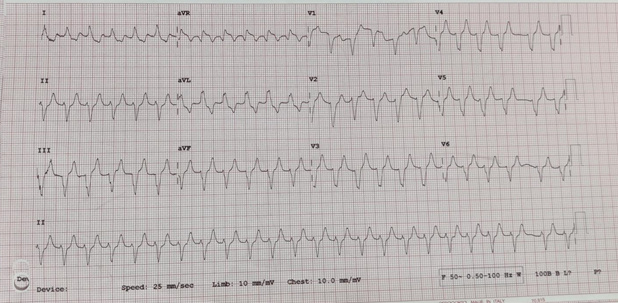
Showed:
• Non sinus rhythm – irregular rhythm
• Left axis deviation
• Rate – 150 bpm
• Wide qrs complex
• Tall t wave noted
• St depression lead 1 , avl
• Sine wave pattern – in 2nd ecg
Probably features of severe hyperkalemia in background of chronic atrial fibrllation with fast ventricular rate
Provisional diagnosis:
• Hyperglycemic state – Diabetic keto acidosis vs hhs
• Severe hyperkalemia – seocndary to aki
• Chronic atrial fibrillation with fast ventricular rate – Sepsis-induced
• Severe sepsis – focus – Urosepsis
• Acute kidney injury – Pre renal – secondary to dehydration
• Dyselectrolytemia
Further investigations revealed the following:
• CBC – Leucocytosis with neurtrophilic predominance (TC – 23100, N84.5%, L6%),
• Mild anemia (Hb : 9.3),
• Platelets – 2.21lakhs
• CRP – elevated (305.13)
• Urea: 114.9
• Creatinine: 3.19
Urine routine:
• Protein ++
• Blood +++
• Glucose ++
• Pus cells – plenty
• Epithelial cells : 8to 10
• RBCs- plenty
• Urine ketone : negative
• Nitrite – negative
Echo done:
• Normal lv function, ef – 60%
• Dilated ra/rv
• Severe pah
• ? Features of cor pulmonale
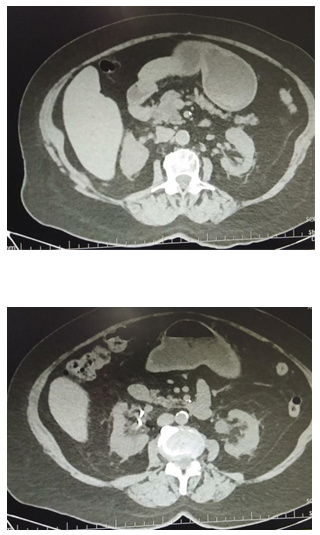
CT chest and abdomen:
• Features of cardiomegaly with CORADS 3
• Features of left-side perinephric fat stranding – probable left pyelonephritis
CT abdomen images showing left-sided perinephric fat stranding – left pyelonephritis
Discussion:
Treatment challenges we faced in ER – diagnostic dilemmas encountered worth discussion:
1) What to treat first? – hyperkalemia? hyperglycemia? AF with fast ventricular rate
2) Do we give fluid boluses to this patient considering patient was in fluid overload status?
3) Concomitant sepsis treatment
A) As patient had severe hyperkalemia of 7.2 meq with sine wave pattern, which is precursor for ventricular arrhythmias like vf/vt, which can be life-threatening, we chose to treat the hyperkalemia first.
Treatment given:
1) Injected calcium gluconate 30 ml iv stat –> repeat dose of 20 ml calcium gluconate after 20 min
2) Injected insulin 12 units iv stat, dextrose deferred as cbg more than 700 mg/dl
3) Asthalin nebulizer 10 mg stat given
ECG changes seen in hyperkalemia include:
• Peaked T waves
• P wave widening / flattening
• PR prolongation
• QRS widening with bizarre QRS morphology
• Conduction blocks (bundle branch block,fascicular blocks)
• Bradyarrhythmias :: sinus bradycardia, high grade AV block with slow junctional and ventricular escape rhythms , slow AF
B) Secondly, we started treatment for hyperglycemia:
Insulin infusion @ 8 units/hour as per dka protocol, with hourly cbg monitoring
Diagnostic criteria for DKA
• Sr. glucose – >250
• Arterial PH – < 7.3
• HCO3 – <15
• Urine ketone – ++
• Sr.ketones – +++
• Anion gap – > 10
• Develops over hours to days
• Most common in type 1 diabetes mellitus
• Mental status – Alert / drowsy / stupor / coma
• Sr.osmolarity – variable
Diagnostic criteria for HHS
• Sr. glucose – > 600
• Arterial PH – >7.30
• HCO3 – >15mmol /l
• Urine ketone – negative
• Sr.ketones – Negative
• Anion gap – <12mmol/l
• Develops over hours to weeks
• Most common in type 2 Diabetes mellitus
• Mental status – Alert / drowsy / stupor / coma
• Sr.osmolarity – > 320mmol/kg
In our patient:
• Urine ketone was negative, thereby ruling out dka
• Considering she had altered mentation with sugars more than 700, serum osmolality was calculated, which was found to be 285 mmol/l , thereby ruling out hhs
• Hence, we continue treatment for hyperglycemia as per sliding scale for insulin infusion
C) After initial hyperkalemia correction -hr settled from 160 to 140 bpm. Now a diagnosis of atrial fibrillation with fast ventricular rate was more obvious as it was unmasked by the decerase in heart rate. As patient was constantly still slightly drowsy and had borderline bp of 90/60 mmhg, chemical cardioversion with inj amiadarone 300 mg inufusion over 1 hour was given slow iv. Heart rate after initial iv bolus of amiadarone was reduced further to 110-120 bpm. Hence, the patient was continued on inj amiadarone infusion @ 900 mg over 24hrs.
ECG features of atrial fibrillation:
• Irregularly irregular rhythm
• No p waves
• Absence of an isoelectric baseline
• Variable ventricular rate
• Qrs complexes usually < 120ms unless pre-existing bundle branch block , accessory pathway , or rate-related aberrant conduction
• Fibrillation waves may be present and can be either fine (amplitude < 0.5mm) or coarse (amplitude > 0.5mm)
• Fibrillatory waves may mimic p waves leading to misdiagnosis
D) Finally the patient was dehydrated, but fluid overload, iv fluids as per dka protocoal was initiated, and ivf – ns 500 ml iv boolus was given. Considering ivc was collapsing and the patient had normal lv function with ef of 60%, but also keeping in mind the underlying cardiac abnormality, deranged kidney functions, and fluid overload status, guarded ivf ns 250 ml bolus was given followed by 100 ml/hr.
E) As all of the above was triggered by an underlying sepsis with source being left pyelonephritis – iv antibitoics was initiated with inj magnex forte 3 gm iv stat followed by 1.5 gm iv bd.
Old diagnostic criteria for sepsis : systemic inflammatory response syndrome (sirs):
• Temp – < 36’c or > 38 ‘c
• Rr – > 20/min
• Hr – >90
• Wcc – <4000 or >11000
New diagnostic criteria for sepsis: quick sequential organ failure assessment score (qsofa):
• Systolic bp < 100mmhg
• Rr – > 22/min
• Altered mental status
• Lactate – >2 mmol
Goal in sepsis:
• Iv antibiotics within first hour
• Fluid resuscitation
• Mean arterial pressure > 65mmhg
• Urine output > 0.5ml/kg/h
• Treatment for the underlying sepsis, hyperkalemia, hyperglycemia, and atrial fibrilaation was initiated simulateneously within 1st hour of presentation, and the patient was treated subsequently under cardiology team and after obtaining diabetologist’s and nephrologist’s opnion. She was discharged with normal hemodynamics after 48 hrs.
• Thereby, I would like to end by saying though this is a very common challenge we face in the emergency department every day, diagnosing a patient along with concomitant initiation of complex treatments is a skill we need to develop as what we do here directly in the emergency department is seen to directly impact the patient’s outcome.
References:
• Tintinalli’s Emergency Medicine – 9th Edition
• RCEM guidelines
 Dr. Noor Akbar
Dr. Noor Akbar
MRCEM Resident – Dept. of Emergency Medicine
Kauvery Hospital, Chennai