We present the case of a 61-year-old female who was brought to our hospital with multiple episodes of flash pulmonary edema. On admission she was in heart failure with uncontrolled hypertension and required NIV. She had undergone angiogram of the Aorta and renal vessels which revealed significant stenosis of proximal segment of the right renal artery with increased PSV. Her left kidney was found to be contracted and measured around 5.8x 6.0cm. Her right kidney was normal in size with maintained corticomedullary differentiation. Renal parameters were deranged – Serum creatinine was 1.8mg/dl. She continued to have hypertension and recurrent episodes of flash pulmonary edema despite continuous lasix infusion and four classes of antihypertensives. Hence, she was dialysed through the right IJV.
After discussion with the nephrologist and cardiologist, we decided to address her ARAS. Review of her angiogram images threw few surprises. Her Aorta was severely diseased with heavy calcification around the right renal artery origin. The upper pole was perfused by a polar branch which originated close to the ostium. We waited for her to stabilize and initially planned to perform the procedure under general anesthesia. The procedure was deemed high risk in view of her having a single functioning kidney, the high probability of distal cholesterol embolization and the possibility of jailing her polar artery.
We approached the right renal artery via a retrograde left femoral approach. The aorta as expected was severely calcified and craggy. The right renal ostium was hidden by a calcified plaque. A LAO- left anterior oblique view revealed a tight (>90%) stenosis of the proximal renal artery and post stenotic dilatation with the polar artery taking off immediately distal to the stenosis. The ostium was engaged with a guiding catheter and the lesion was crossed with a coronary guide wire. Pre dilatation was done with coronary balloons 2X15 and 3X30 and the lesion was stented with a HERCULINKTM 6x18mm balloon expandable stent. Check angiogram showed good perfusion across the stent and a good nephrogram. The polar artery was also preserved.
Her post operative period was uneventful. Her blood pressure and serum creatinine started decreasing from the second postoperative day. She was discharged with stable BP on three antihypertensives and her serum creatinine had dropped to 1.12 mg/dl.
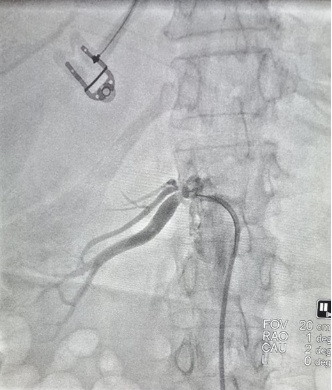
Fig 1: Tight stenosis of the proximal right renal artery and post stenotic dilatation with polar artery taking off immediately distal to the stenosis.

Fig 2: Stenosis stented with a HERCULINKTM 6x18mm stent. Polar artery preserved with good flow postprocedure.
Discussion:
Intervention for Atherosclerotic Renal Artery Stenosis [ARAS] is controversial. The seminal trials STAR, ASTRAL and CORAL advised against intervention. STAR trial had a small cohort and excluded patients with high-risk RAS. ASTRAL had significant recruitment bias. CORAL addressed these concerns to certain extent as it had longer follow up and demonstrated lower systolic BP in the stenting arm.
The 2017 ACC/AHA Hypertension Guidelines provide recommendations on ARAS and its treatment. The authors advise that all patients with ARAS receive medical therapy, based on Level 1A evidence. For patients who do not respond to medical management and continue to exhibit clinical signs of refractory hypertension, deteriorating renal function, or intractable heart failure, revascularization should be considered. However, the ACC/AHA does not fully endorse any specific procedure or confirm outcome benefits.
Post renal artery stenting, hypertension may not be completely corrected. However, there is reduction in the requirement of antihypertensives and prevention of further parenchymal damage to the kidneys.
 Dr. Jan Sujith
Dr. Jan Sujith
Associate Consultant in Vascular Surgery
Kauvery Hospital, Chennai