Periprosthetic Fracture
Fracture associated with an orthopaedic implant (fixation/replacement).
These fractures are increasing due to increased life span, multiple fracture fixation, joint replacement done at earlier ages, trivial trauma, osteolysis, osteoporosis[1], and stress shielding. Patient-specific risk factors are rheumatoid arthritis, osteolysis, osteopenic bone, use of steroid medications, and frequent falls in elderly population. Technique-specific risk factors are femoral cortical notching.
Octogenarian (80 years old) fracture management is never easy and ever-challenging due to multiple comorbidities and age. With periprosthetic fractures, it is a challenging task. A multi-disciplinary approach involving various specialties, patients, patients’ attenders involving in giving care to the patient is needed.
Patient-centric approach and shorter duration of treatment with earliest ambulation is the key in long-term survival.
Presenting a Challenging Case:
An 80-year-old female complains of pain over left knee for one month, following a fall. She was not able to ambulate. Patient was ambulating without aid before fall. Patient was bedridden for the past one month after the fall. She developed multiple bed sores.
Co-morbids- diabetes mellitus, systemic hypertension, seizure disorder, regular medications.
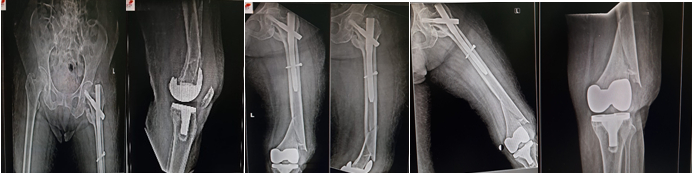
There is history of left intertrochanteric fracture last year, and the patient underwent proximal femoral nailing. Bilateral total knee replacement was done before 10 years.
Positive findings-on examination:
- Patient conscious and oriented.
- Multiple bed sores were present.
- General condition of the patient is poor, dehydrated, Vitals: BP – 100/60 mmHg, Pulse – 92/mins, Afebrile.
Left Knee:
Limb in external rotation, deformed, shortening (1.5 inches), tenderness, diffuse contusion around the knee present. No open wound in the knee, previous scar seen (TKR).
Investigation:
Thorough blood investigations, complete surgical work-up was done.
X-ray – knee, hip. ESR and CRP-infective markers. Dexa-osteoporosis was scheduled later.
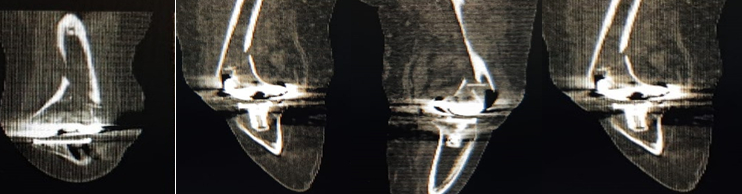
CT Scan-Images:
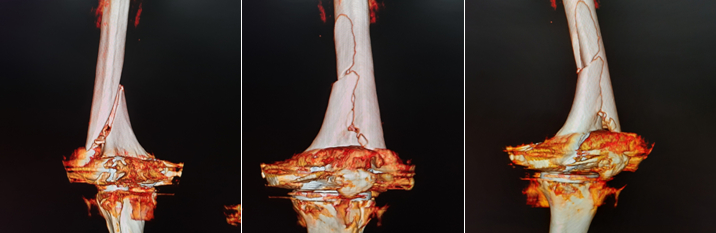
3D Reconstruction CT Images:
CLASSIFICATIONS:

SU CLASSIFICATION – according to fracture location relative to proximal border of femoralcomponent.
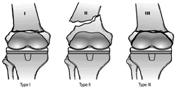
LEWIS AND RORABECK CLASSIFICATION – according to fracture and implant stability

This belongs to type 2 SU’s classification. CT Image shows no obvious evidence of loosening of the implant.
Treatment Options:
Non operative treatment -skeletal traction, splints, cast, braces
Operative treatment – Intramedullary nailing, open reduction internal fixation with LCP or revision arthroplasty.
In view of the fracture pattern and comorbidities, reconstruction of distal femur with LCP was decided. After thorough evaluation from all concerned specialties with high risk, patient was called for surgery.
Challenges involved in this patient were old age, multiple surgeries, and osteoporotic bone (so chances of refracture, implant loosening also expected in view of that) Revision arthroplasty was kept as back up. There was high risk of infection due to grade 3 multiple bed sores and diabetes mellitus. Chance of implant failure and nonunion were expected due to seizures. d.v.t and pulmonary embolism were expected.
Intra Operative Fluoroscopy Pictures:
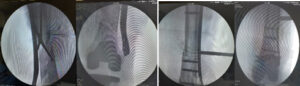
Initially, we started on antibiotics because of high chance of infection after surgery. We got fitness from a geriatrician, cardiologist, plastic surgeon, and anaesthetist. We planned for LCP fixation after discussion since intramedullary nailing and revision arthroplasty were not suitable in this type of fracture.
Under regional anaesthesia, with patient in supine position, we proceeded with the surgery through the lateral approach.
Immediate Post Operative X-ray And Wound Images:

Post- bed side physiotherapy, hip knee mobilization started. Given the severely osteoporotic bone and poor general condition, ambulation was delayed.
One Month Follow Up X-ray And Wound Images:

Wound healed well. Patient was mobilized in wheel chair, bedside mobilization was done, and bed sores were healing.
Discussion:
Periprosthetic fractures are more common with revision joint replacement, less than 5% of primary joint replacement. Elderly patients with decreased bone stock have high probability of these fractures. Management of these fractures are challenging in multiple ways as described earlier. Patient-centric holistic multi-disciplinary approach is needed with combination of mechanical fracture stability and systemic treatments for underlying systemic causes in these elderly patients. Regaining early physical activity is key to the success of the treatment; hence preoperative workup and dedicated postoperative management are necessary.

Dr. Mukunth Krishnamoorthy
Consultant Orthopedic Surgeon
Kauvery Hospital