Pediatric hip replacement, once considered a rare and challenging procedure, has witnessed significant advancements in recent years, offering hope and improved quality of life for young patients facing hip-related issues. While this type of surgery remains relatively uncommon in comparison to adult hip replacements, it has become a viable option for certain pediatric cases, providing a unique set of challenges and considerations for both patients and healthcare professionals. Pediatric hip replacement is typically recommended for children with severe hip joint disorders, congenital abnormalities, or developmental dysplasia of the hip (DDH) that cannot be effectively managed through non-surgical means. These conditions can lead to pain, limited mobility, and long-term joint damage, necessitating intervention to ensure proper growth and development.
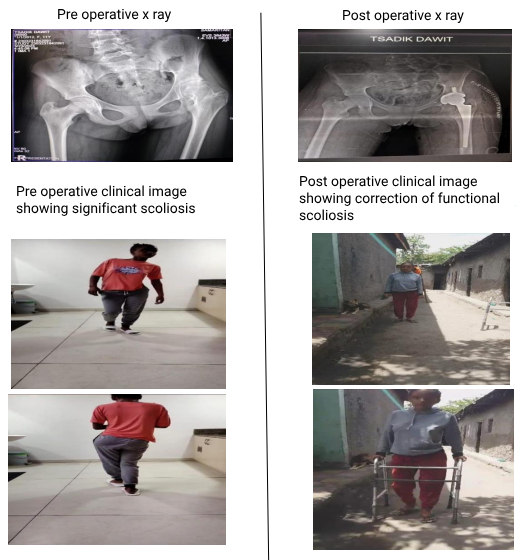
A 13 year old girl from Ethiopia, the cradle of humanity, developed stiffness and pain in her left hip. She had history of contact with tuberculosis and empirical ATT (Anti Tubercular Therapy) was given even though a biopsy proved negative. Her mobility gradually decreased and she presented with complaints of stiffness in her left hip for 3 years. She was evaluated further for any current infection and inflammatory disorders. She had functional scoliosis and possibility of monoarticular Juveline Idiopathic Arthritis was considered and total hip replacement was done. The images depict the amount of scoliosis preoperatively and its correction postoperatively
Surgeons must carefully consider factors such as the child’s age, size, and the potential impact on future growth plates. This requires a highly specialized and individualized approach to address the unique needs of each young patient. Modern pediatric hip replacement procedures benefit from advancements in surgical techniques, materials, and imaging technology. Minimally invasive approaches are increasingly employed, reducing trauma to surrounding tissues and accelerating recovery times. Additionally, improved prosthetic materials, such as high-density polyethylene and ceramic components, enhance the durability and longevity of the implants.
One of the critical challenges in pediatric hip replacement is accounting for the patient’s ongoing growth. Surgeons employ innovative strategies, such as adjustable implants and modular components, allowing for alterations as the child grows. This adaptability is crucial to ensuring that the replaced hip remains functional and accommodates the natural development of the skeletal system. Rehabilitation plays a pivotal role in the success of pediatric hip replacement. Physical therapy and ongoing monitoring are essential to ensure optimal recovery and prevent complications. The involvement of a multidisciplinary team, including pediatric orthopedic surgeons, physical therapists, and pediatricians, is crucial in managing postoperative care and addressing any emerging issues. While long-term data on pediatric hip replacement outcomes are still evolving, early indications suggest positive results in terms of pain relief, improved function, and enhanced quality of life for young patients. Regular follow-up appointments and ongoing monitoring help assess the longevity of the prosthetic joint and address any potential issues that may arise as the child continues to grow.
Conclusion:
The field of pediatric hip replacement has made remarkable strides, offering a ray of hope for children facing complex hip joint issues. As surgical techniques continue to advance and our understanding of pediatric musculoskeletal development improves, the future holds promise for even better outcomes and enhanced quality of life for young patients undergoing hip replacement surgery.


 Dr A. Aravind
Dr A. Aravind Dr. A. William Abraham
Dr. A. William Abraham Dr. Vikraman
Dr. Vikraman