Patient summary
A 30 year old female came to our OPD with complaints of difficulty in swallowing since age 10,which was gradually progressive in nature. Initially she had difficulty in swallowing solids for several years, followed by semi-solids for past 2 years. Since last 3 weeks, there is difficulty in swallowing liquids accompanied by pain during swallowing and loss of weight.
Her mother gave a history of extensive peeling of skin in both her lower limbs at the time of child delivery followed by falling of finger and toe nails 10 days after birth. She had extensive blistering, skin peeling and scarring at points of pressure. She was diagnosed as a case of EpidermolysisBullosa. Long term prognosis was explained and was started on oral steroids till 2 years of age. Later her parents discontinued steroids and lost follow up. None otherfamily member had similar illness/complaints.
On general examination she was poorly built and undernourished, pallor, angular stomatitis and chelitis, absent finger & toe nails,multiplehypo-pigmented and hyperpigmented scars over trunk,face and limbs. Basic blood work up revealed severe microcytic hypochromic anaemia [Hb – 8gm%, MCV-69.1 Fl, MCH-17.5 pg and MCHC – 25.4gm%].Renal and liver function tests were normal.
OGD scopy- She had severe luminal narrowing at the level of crico-pharynx at 15cms. The lumen was negotiated with a 0.035” GW & 10mm CRE balloon followed by dilatation. Scope negotiated beyond, which showed another stricture at 20 cms and CRE balloon dilatation done. Two more strictures were encountered at 26 cms and 35 cms. Balloon dilatation of all strictures were done. Scope passed into stomach. Futher CRE dilatation of strictures were done with 12mm & 13.5mm balloon. Submucosal triamcinolone was injected in 0.5ml aliquots in 4-quadrants at stricture remnant sites. A 20Fr NG tube was placed after nasal re-routing of GW. Patient developed severe left sided headache & returned back to OPD. On examination she has left maxillary sinus region tenderness. So the NG tube was removed & relook endoscopy was done. Scope was easily passed through the stricture remnants into the stomach. Dominant stricture was identified at crico-pharynx(15cms). A 16Fr-NG tube was placed via right nostril. Patient was reviewed after 2-weeks. NG tube was removed & relook endoscopy done. Stricture remnants at 15cms & 20cms were seen with partial healing of mucosa. Scope was passed easily into stomach. She was taught self-dilatation with a 14Fr Foleys catheter with 3cc air. She was able totake solid food after two decades.
Based on the blistering disorder since birth along with esophageal mucosal involvement in the form of esophageal strictures , we made a diagnosis of genodermatoses namely EpidermolyisBullosa with Multiple esophageal stricturing-requiring CRE balloon dilatation followed by self-dilatation of strictures for long term nutritional management.
Discussion
Epidermolysisbullosa (EB) is a genodermatoses characterized by blistering of the skin and mucous membranes induced by minor trauma. Prevalence worldwide is 8-10/ million births.Besides the skin, the gastrointestinal (GI) tract is the most common affected site. Esophagus and oropharynx are the most common affected areas in the GI tract. Esophageal bullae formation is caused by the trauma of solid, hot or poorly masticated foods. Blister formation in the oropharynx and/or esophagus causes symptoms of dysphagia. Also after blister formation and chronical ulcer inflammation, esophageal strictures subsequently give way to mechanical obstruction. The strictures and dysphagia together cause severe malnutrition. Reduced protein intake eventually deteriorates the wound healing process bringing about a vicious circle. The pain that patients suffer while taking food orally is one of the major reasons why they stop eating willingly. The aim should be interfering before the strictures occur; however, this is almost never possible to achieve.
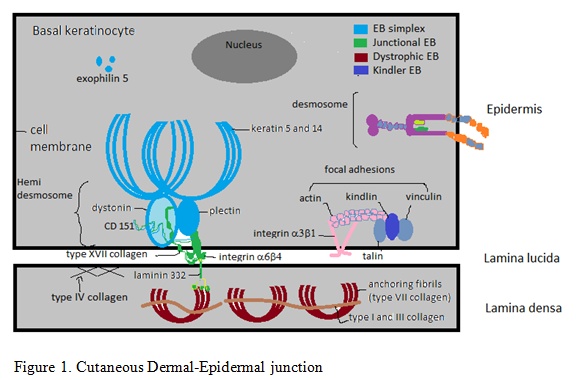
There are four major types: EB simplex (EBS), Junctional EB (JEB), Dystrophic EB (DEB), and Kindler syndrome, based on the level of blister cleavage, genetic inheritance pattern, lesion morphology and genetic mutation. Intraepidermal blistering occurs in EBS. In JEB, tissue separation occurs at lamina lucida in dermo-epidermal junction, whereas in DEB, cleavage occurs in the sub basal lamina. Kindler syndrome can mimic clinically any of the above three types and has multiple cleavage planes.
Dystrophic epidermolysisbullosa (DEB) results from mutations in the gene encoding type VII collagen (see fig.1) which is an essential component of anchoring fibrils. Due to deeper level of cleavage at upper dermis, mucocutaneous scarring, milia and fibrosis is commonly seen in DEB. DEB in inherited in autosomal dominant or recessive pattern. Patients with recessive inheritance are more severely affected. Presence of pseudosyndactyly, contractures and scarring with milia formation are characteristically seen in DEB. Involvement of GIT in the form of esophageal stenosis can occur. Severe protein energy malnutrition and iron deficiency anemia can occur from swallowing problems and malabsorption
Kindler syndrome (KS) is inherited in autosomal recessive pattern. Characteristic features of kindler syndrome are poikiloderma and photosensitivity. There have been case reports of esophageal stenosis and colitis in KS. Patients are at an increased risk of squamous cell carcinoma at acral and mucosal sites.
Treatment
There is no curative treatment for epidermolysisbullosa. Treatment is mainly symptomatic in the form of wound care, and management of systemic complications.EBD seems to be a safe and feasible method for EB patients with esophageal stenosis. After the procedures, the patients admitted that they have reduced dysphagia and there are developments in swallowing. Skin condition also have started to get better as they started to gain weight. Because once they start to eat, their quality of life increases dramatically.
Almost 70% of the patients suffer from esophageal stenosis in the first 25 years of life. There are other approaches like retrograde esophageal dilatation through an existing gastrostomy, colonic interposition or esophageal resection which have severe morbidity and mortality rates. Although it is claimed that a dilatation program with gastrostomy ensures convenience for the procedure and is more successful for weight gaining. Esophagus balloon dilatation with flexible endoscopy is a safe and efficient method in patients with this condition.
EB patients have high calories and protein requirements for wound healing. Nutrition intake is limited by complications like oral and dental problems, esophageal strictures and squamous cell carcinoma of esophagus. Specific diet plan with assistance is crucial in preventing and treating malnutrition, anemia, hypoalbuminemia which occur commonly in EB patients.
 Dr. S. Vadivel Kumaran
Dr. S. Vadivel Kumaran