Ms.KK, 34 years with ESRD due to chronic glomerulonephritis was evaluated for live , related renal transplantation. The only available donor was her mother who was otherwise medically fit to donate but for a mismatched blood group. She was O and her mother was B. Measurement of anti B antibody titer revealed that it was positive for 1: 256 for IgM and 1: 512 for IgG antibodies. There was excellent HLA matching between them (5/6 HLA match)
Family agreed for blood group incompatible renal transplantation and the standard pre transplant desensitization that included Rituximab (anti CD 20 monoclonal antibody) along with tacrolimus, mycophenolate and steroid based immune suppression initiation 2 weeks prior to transplantation was initiated.
Plasmapheresis was started towards bringing down the antibody levels. The titers came down as predicted up to 1:16 for IgG but never came down in spite of adequate immune suppression. The desired titer is 1:4 for IgG antibodies.
She underwent Immuno adsorption (IA) treatment that instantaneously brought down the anti B antibody levels and she underwent successful transplantation. The post operative period was uneventful with normal kidney function and without any rebound increase in antibody titer
Discussion
⦁ Why blood group incompatible transplants were considered absolutely contra indicated earlier?
The blood group antigens are expressed not only in the red blood cells but also on the vascular endothelium. The anti-blood group antibodies are present naturally and transplant across blood group will result in destruction of the kidneys because of these antibodies
⦁ What is the normal procedure in performing ABOi transplants?
The treatment protocol consists of removing these antibodies by plasmapheresis or by immunoadsorption and reducing these antibodies by rituximab (anti CD 20 monoclonal antibody) along with traditional triple immune suppression
⦁ What are the antibody titer aimed prior to transplantation?
Before considering the transplantation the baseline titer is checked. The recipient serum is progressively diluted and made to react with the red cells of the donor. The cell lysis at the highest dilution is taken. Higher the dilution, greater is the level of anti-blood group antibodies.
A titer of less than 1: 512 is considered acceptable and prior to transplant a titer of 1:4 is aimed for
⦁ What are immune adsorption columns?
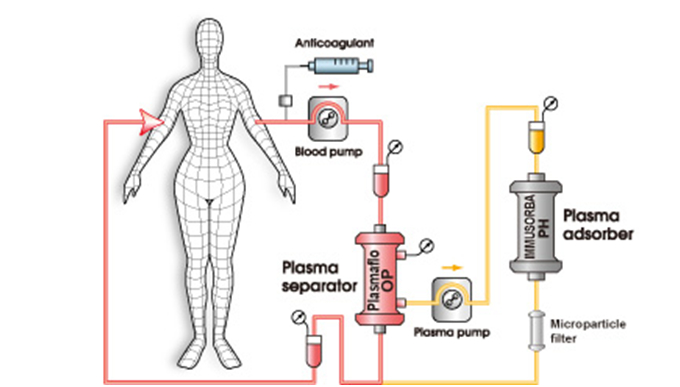
These are special fibers coated with blood group antigens that removes antibodies as the blood passes through. These columns could run for hours and as the blood is recirculated the antiblood group antibodies bind to them and their level comes down.
⦁ What is the procedure to perform IA?
First, patient undergoes plasma pheresis and the removed plasma that contains anti blood group antibodies are passed through these IA column and the plasma is returned to the patient. The anti-blood group antibody titer is assessed every 2 hours and once the titers are brought down to acceptable levels (1:4) the transplant is performed,
⦁ What are the standard protocols available for ABOi transplantation?
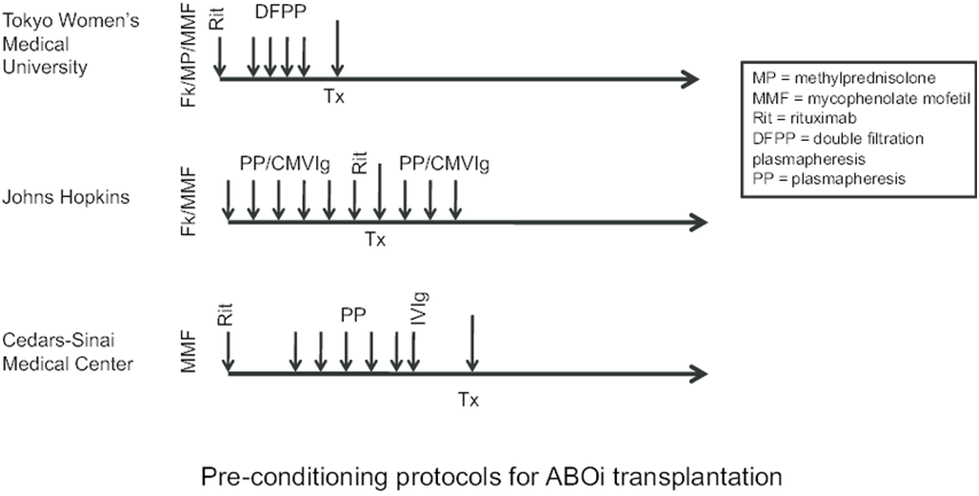
(Ref: Joseph Kahwaji. Rituximab: an emerging therapeutic agent for kidney transplantation. Transplant research and risk management)
⦁ What is the main advantage of ABOi transplant in our patient?
Compared to a blood group compatible donor with no HLA matching, an ABOI transplant with good HLA matching is ideal because the long term graft survival depends on the degree of matching. In our patient the donor is the mother and we generally expect 50 % of the antigen match (3/6) between a parent and their children. Fortunately in this patient the degree of matching was (5/6) and the graft survival is expected to be excellent in the long run.
 Dr.R.Balasubramaniyam. MBBS, DNB( Gen.Med), DNB(Neph)
Dr.R.Balasubramaniyam. MBBS, DNB( Gen.Med), DNB(Neph)
Head, Department Of Nephrology
Kauvery Hospital, Chennai