INTRODUCTION:
Rapidly progressive glomerulonephritis (RPGN) is a clinical syndrome manifested by features of glomerular disease in the urinalysis and by progressive loss of kidney function over a comparatively short period of time (days, weeks or a few months) requiring Dialysis. It is one of the intra renal causes of Acute kidney injury(AKI).
RPGN is usually due to one of the three broad mechanisms of glomerular injury.
- anti-GBM disease
- immune complex mediated injury.
- pauci-immune necrotising (ANCA) and crescentic glomerulonephritis.
Both anti-glomerular basement membrane (GBM) disease and anti-neutrophil cytoplasmic antibodies- myeloperoxidase (ANCA-MPO)-associated vasculitis are small vessel vasculitides that can precipitate the development of RPGN and diffuse alveolar hemorrhage (DAH). These are both rare entities that confer an increased risk of organ functional loss and mortality from respiratory or renal failure.
CASE REPORT:
76 year old obese female who is a diabetic ,hypertensive and OSA on overnight BIPAP presented with complaints breathlessness on mild exertion for past 2 days. On physical examination at admission, blood pressure was 174/86 mmHg, heart rate was 78 bpm with a rhythmic pulse, respiratory rate was 18/min, and the oxygen saturation was 94%,crackles present in the bilateral lung fields, clinical symptoms suggestive of pulmonary edema.
Routine blood investigations revealed severe renal failure with Urea-167 mg/dl, creatinine-11mg/dl. Urine routine showed plenty of RBC and protein-3+.USG revealed normal sized kidneys with corticomedullary differentiation maintained.
Probable diagnosis of RPGN was made and initiated on Hemodialysis (HD) and further investigations revealed Anti-GBM IgG-125.42RU/ml(strong positive),MPO(PANCA)-21.64 Units(weak positive) other markers PR3(CANCA),ANA were negative and complement levels C3 and C4 were within normal limits.
DISCUSSION:
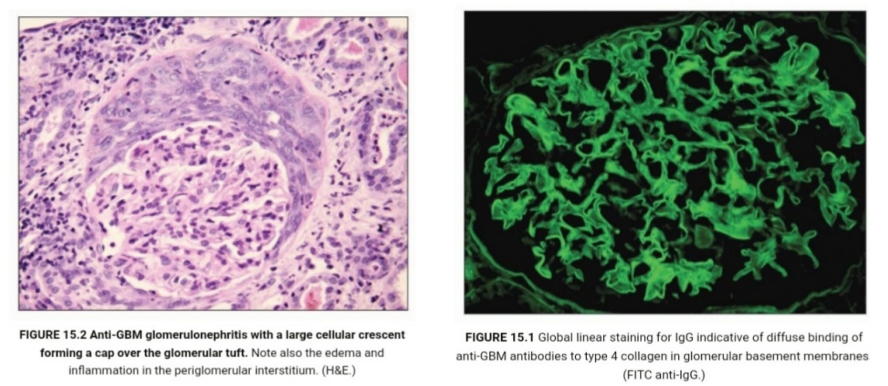
Anti-glomerular basement membrane (anti-GBM) disease is a vasculitis affecting glomerular capillaries, pulmonary capillaries or both. Goodpasture disease is caused autoimmunity to the carboy terminal ,non collagenous(NC1) domain of type IV collagen chain alpha3(IV)NC1,also known as Goodpasture antigen. Type IV collagen is an essential constituent of all basement membranes. Both environmental and genetic factors are important etiologies. There are strong association between Human leukocyte antigen (HLA) class II alleles including DRB1*1501 and DR4 alleles.
Between 50% and 75% of patients with acute symptoms of lung hemorrhage and severe renal failure. In a third to half of patients, renal involvement occurs in the absence of lung hemorrhage. In this group since systemic symptoms are generally not prominent presentation is often late with kidney failure. Whatever be the stage of presentation, once significant kidney impairment has occurred, further deterioration in kidney function is usually rapid and often irretrievably lost
According to one of the largest documented series patients with double-positive anti-GBM and ANCA disease tend to present more evidence of chronic injury (sclerotic glomeruli/fibrosis) on renal biopsy compared to single anti-GBM disease. On the other hand, and quite surprisingly in the face of the previous information, double-positive patients tended to recover more often from dialysis-dependent renal injury after treatment, but no overall survival differences were described. Disease relapse is far more common in ANCA-associated vasculitis and double-positive disease than in single anti-GBM disease.
TREATMENT:
Generally once the diagnosis of Anti-GBM disease was made , treatment (immunosuppression)should be initiated promptly with plasma exchange ,glucocorticoids (pulsing) and cyclophosphamide, but conservative approach for recommended by KDIGO for patients without alveolar hemorrhage but who are oliguric and/or having advanced kidney failure requiring dialysis, especially if they have a very high proportion of crescents(85%-100%) on kidney biopsy .Hence in the above described patient, renal biopsy is deferred since patients cannot lie down in prone position because of her morbid obesity and OSA. Since the patient presented late with severe renal failure requiring dialysis, the chances of renal recovery with immunosuppression(plasma exchange and cyclophosphamide) in anti-GBM disease is very less and infection rate will be more, we have decided to manage conservatively with dialysis. But as she is also MPO(PANCA) positive she was treated with pulsing steroids (500mg) OD for 3 days followed by low dose oral steroids and currently she is on maintenance hemodialysis.
REFERENCES:
- McAdoo SP, Tanna A, Hrušková Z, et al.: Patients double-seropositive for ANCA and anti-GBM antibodies have varied renal survival, frequency of relapse, and outcomes compared to single-seropositive patients. Kidney Int. 2017, 92:693-702. 10.1016/j.kint.2017.03.014
- KDIGO 2024 CLINICAL PRACTICE GUIDELINE FOR THE MANAGEMENT OF ANTINEUTROPHIL CYTOPLASMIC ANTIBODY (ANCA)–ASSOCIATED VASCULITIS
 Dr Vishnu Shankar
Dr Vishnu Shankar
2nd Year Nephrology Resident,
Kauvery Hospital, Chennai