Background Information:
Osteoporotic vertebral fracture(OVF), a common condition in geriatric population presents with broad spectrum of symptoms from mild discomfort to disabling pain. Likewise the treatment options are also aplenty depending on the clinic-radiological features. Medical management of osteoporosis is mandatory after any kind of surgical management of OVF to prevent further fractures in spine as well as appendiceal skeleton. Even in conservatively managed patient, medical management of osteoporosis is pivotal in improving the outcome.
Medical management includes proper evaluation and quantification of the disease, and pharmacological intervention. Osteoporosis work-up includes Dual Energy X-ray Absorptiometry (DEXA scan) and blood investigations to rule-out etiological conditions and pharmacological compatibility. Considering the need for life-long management of osteoporosis, educating the patient and caregivers about disease and treatment is essential to improve the compliance and adherence.
Conducting an audit in this area is important because although surgical management alleviates the acute pain, the importance of medical management in augmenting the outcome and preventing recurrent fractures cannot be neglected. The data from this audit can be utilised to improvise the treatment protocol, educate the patients and address the lacunae in standardisation of osteoporosis management.
Criteria for the Audit
Methodology
- Patient Identification
A search was performed using the Spine and Neurosurgery Department database, to identify all patients who underwent spine surgery between the years 2015 and 2021. From this cohort, a subset of patients was identified, who underwent vertebroplasty with or without instrumented stabilisation. Further information such as the patient history, pre-operative investigations, operative notes, medications given and post – op notes were obtained from the medical records and IT department. This study was registered as audit with our institutions audit department.
- Laboratory and Radiological Data Analysis
The MRI/CT scan reports were analyzed to confirm the presence of vertebral compression fractures, and the level of fracture was identified. DEXA scan reports were analyzed to identify the subset of patients with osteoporotic VCFs. Laboratory investigations including serum calcium, phosphorus, vitamin D, parathormone (PTH) and renal function test and their temporal data were retrieved from hospital’s electronic medical record.
- Treatment Data
The drug possession rate was indirectly assessed by evaluating the pharmacy billing data and follow-up notes.
4. Treatment protocol
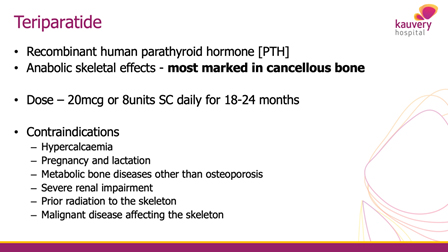
As per NICE guidelines, osteoporosis treatment is dictated by DEXA T-score. Bisphosphonates are recommended in hip fractures whereas teriparatide injection is effective in vertebral fractures. Teriparatide has been proven to be effective in preventing other level fractures in vertebra and hence it was routinely utilised in all our patients with proven osteoporosis and vertebral fracture, along with oral calcium and vitamin D supplements.
Findings of the Audit
A total of fifty patients were identified from the Spine and Neurosurgery database. Out of these 14 were male and 36 were female patients. The mean age of 49 out of 50 patients was 73 years with one outlier (17 years). 32 patients (64%) were identified to have osteoporotic spine fractures, 6 patients (10%) had metastatic tumour, 8 patients (16%) had traumatic injury, 3 patients (6%) had infection and 1 patient had diffuse idiopathic skeletal hyperostosis (DISH).
48 out of 50 patients had an MRI spine done in the initial assessment, 1 patient has a CT scan DL spine, and 1 patient had a PET CT done. DEXA scan was done in 25 out of the 32 patients (78%) with osteoporosis. Serum calcium was measured in 27 out of the 32 patients (84%) and serum phosphorus in 18 out of 32 patients (56%) with osteoporosis. Serum PTH was not measured in the patients and RFT was done in 8 out of 50 patients.
Following the surgery, the patients had an average of 6.4 days of hospital stay. 49 (98%) of the patients had an uneventful post – op period, and 1 patient had developed pneumonia in post-operative period which was managed with antibiotics.
All the patients (100%) were given dietary advice according to their medical history and co- morbidities. The discharge summaries given to the all the patients, clearly stated their diagnosis and contained information about red flag symptoms, regular medications and emergency contact.
The pharmacological intervention was not uniform and was dependent on DEXA scan scoring, co-morbidities and socio-economic factors. Since some of the patients might have procured the medications from outside pharmacy, concrete data about medical possession rate was not achievable. Telephonic follow-up with these patients revealed the reasons for treatment discontinuation which were lack of awareness about duration of treatment (56%), lack of care giver (33%) and allergic reaction (4%).
Conclusion
Patient education is vital to improve compliance and continuous monitoring strategy is needed to improve the persistence in OVF patients. Standardized management protocol will improve adherence to medical management among treating surgeons.
Recommendations
1. Osteoporosis should be recognised as a medical disease which will inculcate an attitude of continuous management as in diabetes mellitus and systemic hypertension.
2. Nursing staff education will improve patient compliance and adherence to treatment.
3. Osteoporosis package may decrease the lapse in laboratory and radiological investigations.
4. Treatment options and relative contraindications are as follows