Carotid body is a chemoreceptor located at the carotid bifurcation and is part of the extra adrenal paraganglia system. They are critical for response to hypoxia and release neurotransmitters. Carotid body tumour, also known as paraganglioma or chemodactoma is a rare tumour. It occurs more in females. It can be familial, bilateral or be part of multiple endocrine syndromes. One identifiable risk factor has been chronic hypoxia due to pulmonary disease and those who live at high altitude
CBT is a slow growing tumour and commonly presents as a painless neck mass at the carotid triangle. Rarely a functional tumour may produce palpitation and tachycardia. Although CBTs are benign lesions, they have a tendency to turn into malignant tumours in approximately 10% of all cases. Ct angiogram is diagnostic. It shows the highly vascular tumour at the carotid bifurcation causing characteristic splaying of the carotids. Blood supply to the tumour is usually from the external carotid. These tumours have been classified into 3 types depending on the involvement of the carotid artery. Surgical excision is considered as the treatment of choice. Surgical excision is challenging since the tumour is highly vascular. It requires careful dissection of the tumour by cauterising the multitude of tiny feeders from the carotid without injuring the carotid artery. Larger type 3 tumours require preoperative embolization to reduce the vascularity and facilitate resection. Some cases require excision of the carotid along with the tumour and reconstruction of the internal carotid artery.
CASE REPORT
52-year-old man presented with painless, intra-oral swelling of 3months duration. Physical examination revealed vague fullness in the right carotid triangle with palpable carotid on right side and no bruit. There was abulge in the right lateral pharyngeal wall with medial displacement of the right tonsil (Fig.A). A firm mass of 4x5cm was palpable at intra-oral examination. Cranial nerve examination was normal. CT angiogram of the neck demonstrated a large highly vascular mass lesion noted in the right carotid and parapharyngeal space. There was lateral displacement and splaying of right internal and external carotid arteries and the tumour was extending cephalad up to skull base and medially was causing bulge over the pharyngeal wall (Figure B). Since the lesion was large extending up to the base of skull, a multidisciplinary approach was carried out. Preoperative embolization was planned. Digital subtraction arteriogram revealed that the tumour was predominantly supplied by Pharyngeal branches of Ascending pharyngeal artery and superior thyroid artery. Selective embolization of feeding vessels, were done using PVA particles and gel foam (Figure C).There was significant reduction in tumour blush post procedure. Surgical excision planned 24hrs later
Based on the preoperative imaging findings we were prepared for mandibulotomy if the upper extent of the tumour was not accessible. Hence, a transverse upper neck incision was used to expose the tumour. Surgical resection of tumour in toto after dissecting from vessels, ligating the feeding branches was done without the necessity for mandibulotomy. Pre-operative embolization helped in reducing the intra-operative bleeding. No blood transfusion was required. Ansa cervicalis, hypoglossal and the vagus nerve were identified and preserved. Post-operative period was uneventful (Figure D&E)
RESULTS
Surgical pathology of tumour was consistent with paraganglioma and negative for malignancy.
CONCLUSION
Proper clinical examination and imaging can help in diagnosing a carotid tumour. Large vascular tumours with extension up to skull base restricts the access to distal internal carotid in the neck. So endovascular embolization should be considered and the surgeon should be ready to do mandibulotomy to reach the base of skull.
References
- Power AH, Bower TC, Kasperbauer J, et al. Impact of preoperative embolization on outcomes of carotid body tumor resections. J Vasc Surg. 2012;56(4):979–989.
- Large series discussing the ef ect of preoperative embolization. Sevilla Garcia MA, Llorente Pendas JL, Rodrigo Tapia JP, Garcia Rostan G, Suarez Fente V, Coca Pelaz A. [Head and neck paragangliomas: revision of 89 cases in 73 patients]. Acta Otorrinolaringol Esp. 2007;58(3):94–1

Fig A : Showing bulge in right lateral pharyngeal wall with medial displacement of tonsil
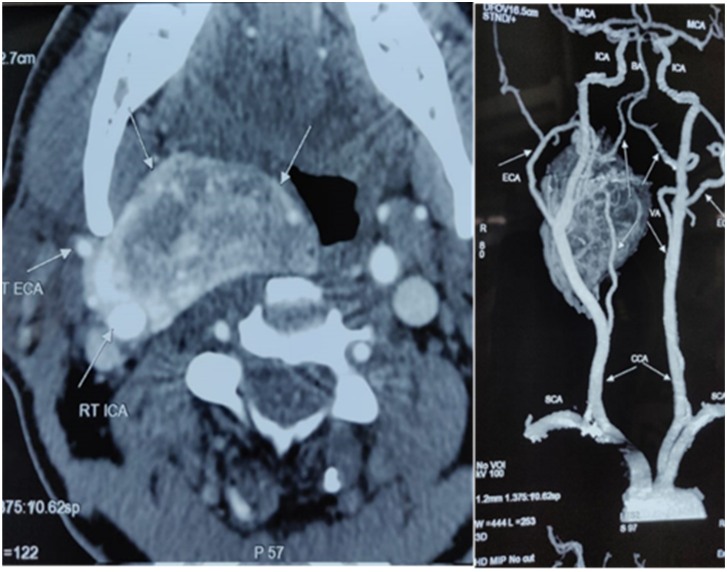
Fig B: A large vascular tumor seen at carotid bifurcation which is placed medially, compressing oropharynx
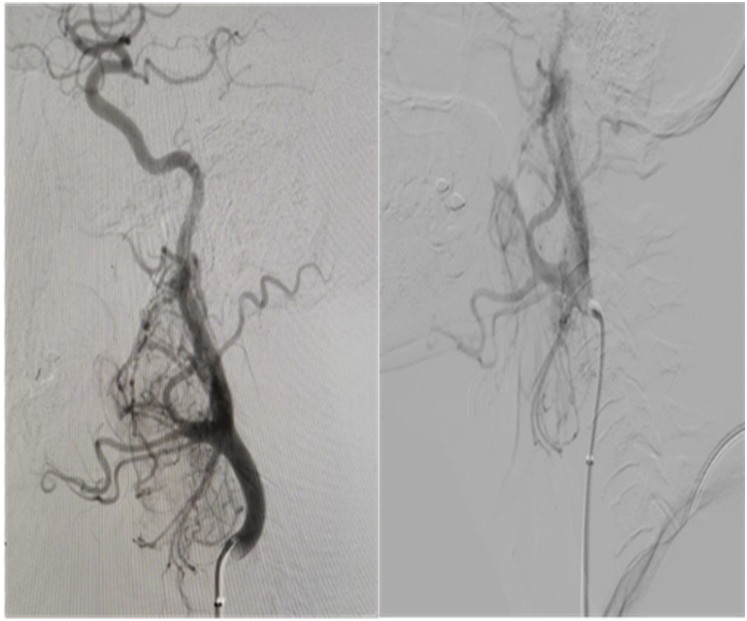
Fig C:Tumour blush noted measuring about 4.3 x 3.6 cm fed by ascending pharyngeal and superior thyroid arteries mainly. Significant reduction in Tumour blush post procedure
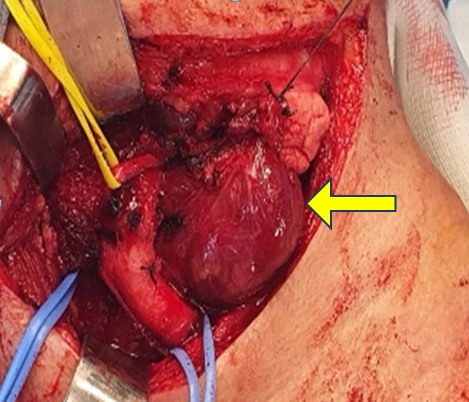
Fig D: Intra-op picture showing carotid artery and the CBT (arrow). Yellow looped structure is hypoglossal nerve and the two blue loops shows the carotid
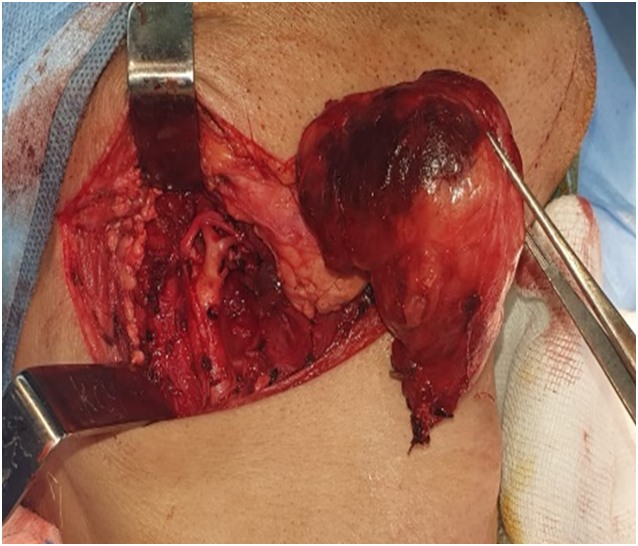
Fig E: Shows the Specimen of carotid body tumour removed from body


 Dr. Archana, MBBS, DNB (General Surgery)
Dr. Archana, MBBS, DNB (General Surgery)