A 37-year-old male came with abdominal pain for 2 days which started after alcohol intake. A clinical diagnosis of acute pancreatitis was made. Serum lipase was 1019 U/L. Liver function test was normal. CT Abdomen plain showed chunky calcifications in head and uncinate process of pancreas with dilated main pancreatic duct. Mild peripancreatic fat stranding with adjacent duodenal wall thickening – features suggestive of chronic calcific pancreatitis. Patient was taken up for endoscopy in view of dilated pancreatic duct for assessment of ampulla which showed normal ampulla and edematous posterior wall of duodenal bulb. His Serum calcium, lipid and thyroid profile were within normal limits. He was managed conservatively and discharged after 5 days.
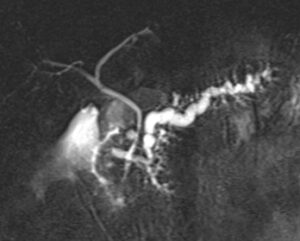
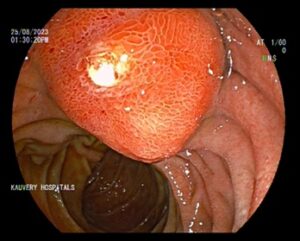
Patient got readmitted after 2 days with severe abdominal pain. His serum lipase was 354 U/L. His previous CT Abdomen was reviewed, and a detailed discussion was made with radiologist, there was a prominent bulge in the duodenal lumen with focal calcification at D1-D2 junction and calcification in uncinate process of pancreas and dilated main pancreatic duct (fig 1). For further evaluation MRCP was done which showed crossing over sign of pancreatic duct with common bile duct suggestive of pancreatic divisum with a calculus obstructing the duct of Santorini at the duodenum (fig 2). He was taken up for ERCP which showed an impacted stone at the minor papilla (fig 4). The stone was retrieved, and his abdominal pain subsided. He had no further episodes of abdominal pain on follow-up. This situation of impacted stone in minor papilla causing acute pancreatitis in pancreas divisum has been reported in only four other cases in the literature.
FIGURE 1: CT ABDOMEN showing focal calcification at D1-D2 junction
FIGURE 2: MRCP showing crossing over sign
FIGURE 3: Normal major papilla
FIGURE 4: Bulging minor papilla with impacted stone
FIGURE 5: Minor papilla stone extraction after sphincterotomy
DISCUSSION
Introduction:
Pancreas divisum is the most common congenital anomaly of pancreas, occurring in 10% of individuals. It occurs when ventral and dorsal pancreatic buds fails to fuse properly during fetal development, resulting in formation of two separate pancreatic ducts instead of one, so that the pancreatic drainage is accomplished mainly through the accessory minor papilla.
More than 95% of patient with pancreatic divisum are asymptomatic. Recent studies suggest that pancreas divisum do not predispose to development of pancreatitis. However, combination of pancreas divisum and small accessory orifice result in dorsal duct obstruction.
Pancreas divisum variants:
- Type 1- total non-union of ventral and dorsal ducts
- Type 2- absent ventral duct
- Type 3 – rudimentary communication between the ventral and dorsal ducts.
In our case, initially alcohol was attributed to acute pancreatitis as no other causes like cholelithiasis, trauma, medications, infections, hypertriglyceridemia, hereditary and auto-immune conditions were identified. In subsequent episode of pancreatitis, a detailed discussion with the radiologist was done regarding the CT findings and pancreasdivisum (type 2) with a calculus obstructing the duct of santorini, which was evident on MRCP was the cause of recurrent acute pancreatitis.
Diagnosis:
Diagnosis is often made with imaging studies such as endoscopic ultrasound, abdominal CT scan, MRCP. ERCP is done for patients with MRCP evidence of pancreas divisum in whom therapeutic intervention such as dorsal duct stenting or minor papilla sphincterotomy is planned.
In our case with a ERCP scope, a bulging minor papilla with an impacted white stone and surrounding edema was seen. Using Heubridge needle knife, pre-cut sphincterotomy was done to retrieve the impacted stone and minor papilla extended sphincterotomy was done (fig 5). The stone was retrieved. PD-Stent was not placed as there was only one stone in Santorini duct causing obstruction.
Conclusion:
Pancreas divisum is a rare cause of acute pancreatitis. An impacted stone at the minor papilla is even rarer. In this case a detailed discussion with a radiologist has revealed a rare ductal anatomy with a cause of obstruction which was therapeutically managed to give a cure.
References:
- Tadao Tsuji et al: Endoscopic treatment of pancreatic diseases via Duodenal Minor Papilla: 135 cases treated by Sphincterotomy, Endoscopic Pancreatic Duct Balloon Dilation (EPDBD), and Pancreatic Stenting (EPS): Annals of Clinical Gastroenterology and Hepatology, 08 July 2019: ISSN: 2640-2750
- Farooqi R, Burke C, Chahal P, et al. (August 25, 2019) Acute Pancreatitis in Pancreas Divisum Secondary to an Impacted Stone in the Minor Papilla. Cureus 11(8): e5481. doi:10.7759/cureus.5481
- Hart P.A., & Conwell D.L., & Krishna S.G. (2022). Acute and chronic pancreatitis. Loscalzo J, &Fauci A, & Kasper D, & Hauser S, & Longo D, & Jameson J(Eds.),Harrison’s Principles of Internal Medicine, 21e. McGrawHill. https://accessmedicine.mhmedical.com/content.aspx?bookid=3095§ionid=264533282
 Dr Pawan Kumar PR
Dr Pawan Kumar PR
DNB Resident, Department of General Medicine
Kauvery Hospital, Chennai
 Dr. S. Sivaram Kannan
Dr. S. Sivaram Kannan
Clinical Lead & Chief Consultant Physician
Kauvery Hospital, Chennai
 Dr Vadivel Kumaran S
Dr Vadivel Kumaran S
Senior Consultant, Department of Medical Gastroenterology
Kauvery Hospital, Chennai