A 35-year-old man from Bangladesh presented with intermittent mild right upper upper-quadrant pain for 2 years. His systemic examination was normal except for mild tenderness. His vital signs were normal. He is a known case of recurrent pyogenic cholangitis, S/P open cholecystectomy/ ERCP with CBD stone extraction/stenting/surgery with left lateral segmentectomy of liver/ Re- ERCP with CBD stone extraction/ stenting (November 2021 – February 2023). When his symptoms started 2 years back, he visited an hospital in Bangladesh and was diagnosed to have choledocholithiasis with hepatolithiasis. MRCP done showed multiple stones in left hepatic duct, common hepatic duct and common bile duct with the largest measuring 12*14 mm in CBD with upstream dilatation of intrahepatic bile duct and CHD (about 12 mm); CBD was dilated (11 mm); Gall bladder was normal in size; Pancreas was normal in morphology and signal characteristics; main pancreatic duct was normal. The liver function test revealed mildly elevated alkaline phosphatase. Patient underwent open cholecystectomy and choledocholithotomy in November 2021. T tube cholangiogram done 1 month later revealed retained calculus in CHD. ERCP with stenting-papillotomy with balloon sphincteroplasty and partial stone extraction was done in January 2022. The patient was planned for CBD stent removal after 3 months and he did not follow up. 8 months after ERCP stenting, he presented with fever and RUQ pain to the same hospital where previous procedures were done. MRCP revealed dilated CBD with multiple filling defects and CBD stent insitu. Left lateral section of liver (segment III ) was atrophied. Left lateral segmentectomy of liver and choledocholithotomy (stone extraction, stent removal) was done in October 2022. Multiple stones with sludge was seen in CBD. Histopathology of left lobe of liver showed no evidence of malignancy. Patient developed epigastric intrabdominal abscess after the surgery for which abscess drainage and iv antibiotics were administered. USG abdomen done 2 months after the surgery in December 2022 showed CHD, CBD dilation with distal CBD calculus and CBD sludge. He again developed RUQ abdominal pain and fever in February 2023. MRCP done revealed choledocholithiasis with proximal dilatation of biliary tree, cholangitis with abscess formation. Blood investigation showed elevated alkaline phosphatase and ESR. ERCP done in February 2023 revealed multiple stones with sludge in CBD and RIHBT; a double pigtail biliary stent was deployed at CBD. Cholangitis was treated with iv antibiotics. The pancreas and main pancreatic duct were normal in all the imaging studies done in the past 2 years. Tumor markers (AFP, CA 19-9, CA 125, CEA) were all negative. The patient, now, came to our hospital with recurrent mild RUQ abdominal pain. MRCP done revealed mild dilatation of IHBR with pneumobilia, mildly prominent CHD and proximal CBD. ERCP, done however, showed no calculus or stricture; there was no CBD stent insitu indicating spontaneous expulsion.
Recurrent pyogenic cholangitis, also known as Hongkong disease, oriental cholangiohepatitis, biliary obstruction disease of Chinese is a disease prevalent in Southeast Asia. Risk factors include low socioeconomic class, poor hygiene1,2. Infection with Clonorchis sinensis, Opisthorchis species and Ascaris lumbricoides are cited as contributors of RPC. Chronic infection with these helminthes causes inflammation of biliary epithelium, decreases host immune response and predisposes the individual to translocation of gut pathogens such as Escherichia coli, Proteus, Klebsiella upstream 4,5. A unique feature of RPC is hepatolithiasis resulting in intrahepatic calcium bilirubinate calculi which unlike cholesterol stones do not cause obstruction but cause biliary epithelial inflammation and stricture formation. Intrahepatic duct stones were present in 82% of patients with in Korean study3. Only half of the patients with RPC 6,7,8 have evidence of infection in the form of eggs in concentrated stool specimen9, eggs or intact worms in biliary/ duodenal aspirate, peripheral eosinophilia and elevated IgE levels 10. Other causes of RPC are low fat diet (esp. saturated fats) as it can reduce gall bladder contractility and cause stone formation. Severe malnutrition causes deficiency of D- glucarolactone (beta glucuronidase inhibitor) and result in bilirubin deconjugation/ stone formation.
Treatment of RPC is with IV antibiotics, antihelminthic drugs. ERCP/ Hepatic resection +/- Hepaticojejunostomy are useful treatment options.
Images :
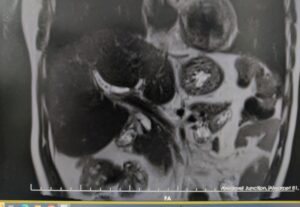
1) This MRCP image shows dilated right hepatic duct.
2) Dilated biliary system (right hepatic duct, left hepatic duct and common hepatic duct) is seen in the coronal section of MRCP
3 & 4) ERCP shows no stricture or stone in the biliary system.
1.
2.
3.

4.
1) Nagase M, Hikase Y, Soloway R, et al. Gallstones in Western Japan. Factors affecting the prevalence of intrahepatic stones. Gastroenterology 1980;78:684–90.
2) Kim M, Sekijima J, Lee S. Primary intrahepatic stones. Am J Gastroenterol 1995;90:540–8.
3) You MS, Lee SH, Kang J, Choi YH, Choi JH, Shin BS, Huh G, Paik WH, Ryu JK, Kim YT, Jang DK, Lee JK. Natural Course and Risk of Cholangiocarcinoma in Patients with Recurrent Pyogenic Cholangitis: A Retrospective Cohort Study. Gut Liver. 2019 May 15;13(3):373-379. [PMC free article] [PubMed]
4) Kaufman HS, Magnuson TH, Lillemoe KD, Frasca P, Pitt HA. The role of bacteria in gallbladder and common duct stone formation. Ann Surg. 1989 May;209(5):584-91; discussion 591-2. [PMC free article] [PubMed]
5) Suzuki Y, Kobayashi A, Ohto M, Tsuchiya Y, Saisho H, Kimura K, Ono T, Okuda K. Bacteriological study of transhepatically aspirated bile. Relation to cholangiographic findings in 295 patients. Dig Dis Sci. 1984 Feb;29(2):109-15. [PubMed]
6) Chou S, Chan C. Recurrent pyogenic cholangitis: a necropsy study. Pathology 1980;12:415–28.
7) Yellin A, Donovan A. Biliary lithiasis and helminthiasis. Am J Surg 1981;142:128–36.
8) Carmona R, Crass R, Lim Jr RC, et al. Oriental cholangitis. Am J Surg 1984;148:117–24.
9) Lim J. Oriental cholangiohepatitis: pathologic, clinical and radiologic features. Am J Roentgenol 1991;157:1–8.
10) Liu L, Harinasuta K. Liver and intestinal flukes. Gastroenterol Clin North Am 1996;25:627–36.


 Dr Azharuddin M
Dr Azharuddin M Dr Arvind M A
Dr Arvind M A