In this report, we aim to present a case of 45 years old male patient came with complaints of giddiness and fall, left upper and lower limb weakness, dysarthria. Patient underwent CT-cerebral angiogram to rule out stroke.
Cerebral angiogram shows circumferential wall thickening with suspicious peripheral wall enhancement seen in distal cervical, petrosal and laceral part of right ICA causing moderate luminal narrowing and near total narrowing in the laceral part of ICA. However, there is normal contrast opacification in distal vessels.
The possible differential diagnosis includes vasculitis and dissection.
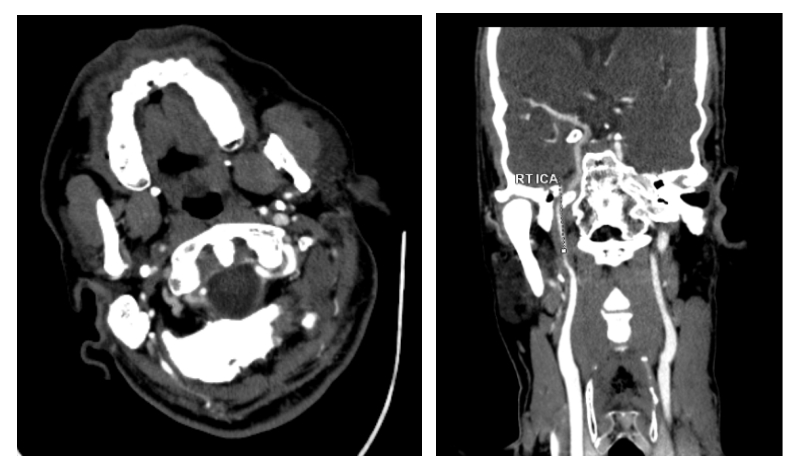
FIG 1:(A & B) CT cerebral angiogram shows concentric thickening of petrosal portion of right ICA. There is subtle peripheral enhancement surrounding the thickening.
To rule out dissection, MRI brain was taken. Multifocal acute infarcts with low ADC values noted in right frontoparietal region (both cortical and subcortical), right basal ganglia and right superior perisylvian region. Crescentic T2w/T1wFS hyperintense signal involving the canalicular segment of right ICA with mild attenuation of flow signal – imaging findings are concern for dissection.


FIG 2 :(A & B) MRI T1 and T1FS images show crescentic high signal seen in in right laceral part of Internal carotid artery-Reflecting intramural hematoma.
IV thrombolysis was deferred in view of increased risk of bleeding. Interventional Radiologist opinion was sought for intracrnial mechanical thrombesctomy and was adviced to manage conservatively. High dose antiplatelet with statins and anticoagulation was initiated.
Follow up MRI was taken. It showed new infarcts in right perisylvian region. MRA showed significant luminal narrowing (~70-80%) of right ICA from origin with attenuated flow in rest of the cervical ICA.
Patient was able to tolerate chair mobilization and attempting to stand with Knee brace. He was adviced to continue physiotherapy.
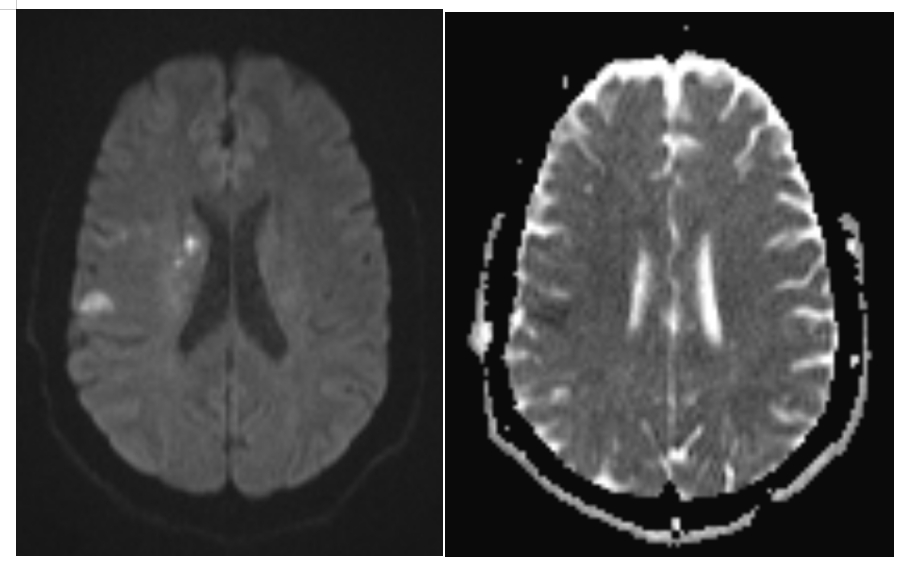
FIG 3 (A & B):Diffusion restriction with low ADC values seen in right perisylvian region

FIG 4:Significant luminal narrowing (~70-80%) of right ICA
Discussion
Internal carotid artery (ICA) dissection is characterized by blood entering the arterial wall through a tear in the intima, similar to other types of arterial dissection. This condition is notably recognized as a prevalent cause of stroke among younger individuals. Dissections can occur at any age, they are particularly common in patients under 45, where they account for approximately 20-25% of strokes in this demographic (1). The annual incidence rate of ICA dissection is estimated to be between 2.6 and 2.9 cases per 1,00,000 individuals (2).
The mechanism behind ICA dissection involves the formation of an intramural hematoma due to the intimal tear, which can lead to compromised blood flow and subsequent ischemic events in the brain. This dynamic process may result in either stenosis or occlusion of the artery, increasing the risk of stroke.
In angiography, the string sign—indicating high-grade filiform stenosis of the ICA -is a typical but not exclusive finding in dissection cases (3). Flame sign in DSA and CT angiography -gradual tapering of contrast opacification in the mid-cervical internal carotid artery[1], sparing the carotid bulb. The term “flame sign” to describe the appearance of a totally occluded ICA in angiography when the string (the narrowed lumen) is no longer visible.
Goldberg et al. (4) described a phenomenon where the hematoma appears to “spiral around the lumen.” This observation aligns with our finding that hematomas are typically located on the convex side of the vessel. While we cannot provide a definitive explanation for this, we hypothesize that, possibly due to arterial pressure, subintimal hemorrhage may penetrate more easily along this side because of its greater diameter.
Conservative medical management is frequently sufficient for patients, primarily involving antiplatelet therapy accompanied by anticoagulation. If patient experience ischemic events inspite of medication, endovascular treatment can be advantageous.
Differential diagnosis:
Fibromuscular dysplasia
Bilateral involvement of ICA. Multifocal stenosis with adjacent dilatations also referred to as the string of beads sign. Type II FMD (stenotic type) mimic as ICA dissection in DSA.
Atherosclerosis
Involves the carotid bulb. Ulcerated plaque may mimic an intimal flap on axial images.
References
1.Kadkhodayan Y, Jeck DT, Moran CJ, Derdeyn CP, Cross DT. Angioplasty and stenting in carotid dissection with or without associated pseudoaneurysm. American Journal of Neuroradiology. 2005 Oct 1;26(9):2328-35.
2.Blum CA, Yaghi S. Cervical artery dissection: a review of the epidemiology, pathophysiology, treatment, and outcome. Archives of neuroscience. 2015 Oct;2(4).
3.Wilms G, Marchal G, Demaerel P, Decrop E, Van Hecke P, Baert AL. Spontaneous dissection of the cervical internal carotid artery. Diagnosis by MRI. Journal de Radiologie. 1989 Mar 1;70(3):225-7.
4.Goldberg HI, Grossman RI, Gomori JM, Asbury AK, Bilaniuk LT, Zimmerman RA. Cervical internal carotid artery dissecting hemorrhage: diagnosis using MR. Radiology. 1986 Jan;158(1):157-61.
 Dr. Kanagasabai Kamalasekar
Dr. Kanagasabai Kamalasekar
Consultant Radiology
Kauvery Hospital, Chennai
 Dr. Firdhous Begum
Dr. Firdhous Begum
Post Graduate Resident – Radiology
Kauvery Hospital, Chennai
 Dr. Ameer Hussain MBBS, MD(RD), MICR
Dr. Ameer Hussain MBBS, MD(RD), MICR
Consultant Radiologist
Kauvery Hospital, Chennai