Introduction
Post operative Neuro surgical patients who require monitoring are retained in ICUs for longer duration leading to increasing expenditure. In lower-acuity settings like wards, they require ongoing monitoring: either manually or using cardiac monitors. Manual measurement of vital signs at fixed intervals is the standard clinical practice in hospital wards once every 4 hours.
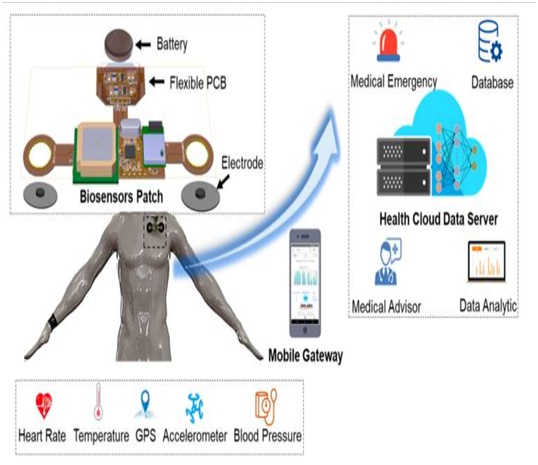
Early Warning Scores (EWS) measured may not be reliable owing to their limitations like fixed intervals, incorrect scoring and variability in person. Conventional monitors used are large which impair patient mobility, require wires which interfere with rehabilitation exercises. Wearable biosensor is portable, wireless, non-invasive and single use device which can monitor vital parameters. The Data collected by sensors are transmitted and assessed remotely on a common console in a nurse station or a mobile device. It is also used to monitor many patients simultaneously
Methodology and results:
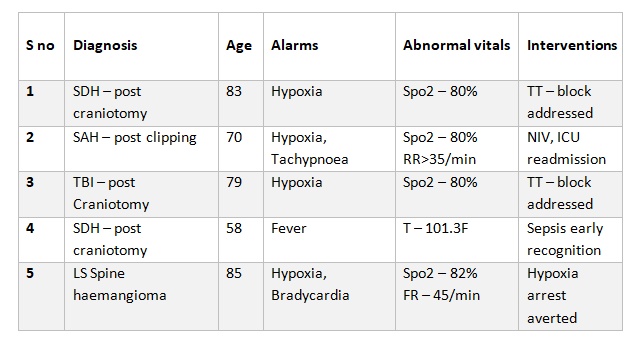
5 patients with primary neurological pathology post neurosurgery who required ongoing monitoring were selected. FDA approved single-use device which was applied to left infraclavicular area with adhesive pad detects two-channel ECG, heart rate, respiratory rate, body posture, skin temperature and SpO2.
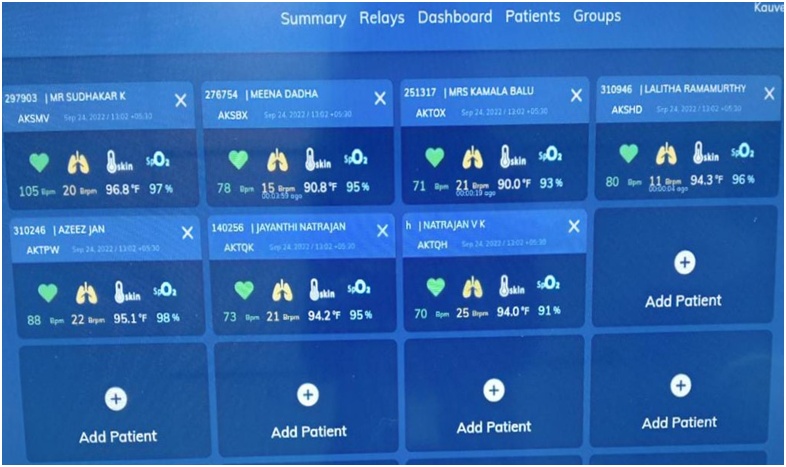
All parameters for multiple patients were accessed remotely on a Control Centre Dashboard. Alarms customized as per patient’s physiology and all alerts were addressed physically. All patients were monitored for durations as deemed necessary by the treating clinical team.
A worsening of the EWS lead to activation of Rapid response team in the hospital as per protocol. All alerts were managed by the Rapid Response Team and appropriate interventions were taken
Discussion:
Patients with neurological pathology need to be monitored for vitals as well as body position. These patients have a low GCS, they can’t change position themselves. This helps in avoiding bedsores and associated infections.
Hypothalamic dysfunction can cause neuropathic fever. Fever is associated with poor neurological outcomes and increases cerebral oxygen consumption, resulting in increased blood volume. Shivering increases metabolic rate and heat production, promotes vasoconstriction to reduce heat loss, and causes hypercapnia, acidosis, hypoxemia, or hypotension. These signs can cause a sympathetic increase in cerebral blood flow.
Increased cerebral blood volume increases ICP and poses a risk of decreased cerebral perfusion pressure leading to tissue ischemia. Patient hyperventilation may be a sign of elevated ICP. Hypertension, bradycardia, and irregular breathing or apnea with increased pulse pressure (increased systolic pressure and decreased diastolic pressure) indicate a brainstem hernia (Cushing’s triad) that requires urgent intervention.
Early detection of fever prompts an evaluation of sepsis and timely administration of antibiotics. Most of the Neurosurgery patients may require tracheostomy, these patients can also be monitored in low acuity settings for tube block.
Advantage of wearable biosensors:
Biosensors are smaller, light-weight, greater sampling frequency, relay information wirelessly. Patient mobility is not compromised and non-invasive sensors are well tolerated. This reduces multiple monitors and wires around patients which helps them in physiotherapy.
Alerts are generated remotely in a console at nurse station, there is no disturbance to patients or panic family attenders. Archived data can be retrieved whenever needed and the trends can be reviewed, compared and stored. Decreased manual work for the nurses and saves time– 1 nurse can monitor up to 15 patients simultaneously. Can be used in limiting contact in pandemic situation/high infection transmission. Most alerts occurred during evenings and nights when patients are vulnerable to unnoticed deterioration
Conclusion:
Remote continuous monitoring with automated alerts has the potential for early recognition of physiological decline in Post operative Neurosurgery patients. These biosensors may be used for round-the-clock detection of EWS in such patients. This may be cost and resource-effective means of enhancing patient safety in low-acuity care settings. Future studies should focus on their diagnostic accuracy, clinical benefit and cost effectiveness.
References:
⦁ Vix, Michel & Rodriguez, Maylis & Ignat, Mihaela & Marescaux, Jacques & Diana, Michele & Mutter, Didier. (2020). Postoperative Remote Monitoring with a Transcutaneous Biosensing Patch: Preliminary Evaluation of Data Collection. Surgical Innovation. 27. 155335062092946. 10.1177/1553350620929461.
⦁ Joshi M, Ashrafian H, Aufegger L et al. Wearable sensors to improve detection of patient deterioration, Expert Review of Medical Devices. 2019 Feb;16(2):145-154
⦁ Weenk M, Koeneman M, van de Belt TH et al. Wireless and continuous monitoring of vital signs in patients at the general ward, Resuscitation 2019; Mar;136:47-53
⦁ Breteler MJM, Huizinga E, van Loon K et al. Reliability of wireless monitoring using a wearable patch sensor in high-risk surgical patients at a step-down unit in the Netherlands: a clinical validation study. BMJ Open. 2018 Feb 27;8(2): e020162


 Dr. S. Arun Sathish
Dr. S. Arun Sathish Dr. Aparna Pande
Dr. Aparna Pande