Mitral stenosis(MS) is one of the commonest valvular lesions seen in patients with Rheumatic heart disease. Patients with severe MS are at increased risk of developing complications such as perioperative pulmonary edema, cardiac failure, arrythmias, embolic events, hemoptysis, infective endocarditis, pulmonary infection, etc, during the perioperative period. Hence adequate preop optimization and planning is necessary before the surgery. We are going to discuss about one such a case posted for hemiarthroplasty
History
69/F came to ER with a history of giddiness and fall, sustained left intertrochanteric fracture of femur. She is a known case of diabetes mellitus, Rheumatic heart disease with Severe mitral stenosis, Chronic Atrial fibrillation with CVR on T.Digoxin, Calcium channel blocker, T.Acenocoumarol and Hypothyroid on medical management. While receiving, patient heart rate was 132-140 per minute(variable), BP – 100/50mmHg ECG showed AF with FVR. Hence amiodarone infusion was started as per Cardiologist advice and the patient was shifted to CCU for further evaluation and treatment. Hemiarthroplasty was planned for IT fracture and so investigations such as CBC, RBS, RFT, LFT, PTINR, ECG were done, Echo was taken which showed Ejection fraction 30%, Severe PAH 64mmHg, Severe MS MVA 0.8, Severe TR, Moderate AS. PTINR was found to be 6.5 and four units of FFP were transfused before taking up for surgery. Trop I was found to be positive and thereby started on Heparin iv 8th hourly

Pre-op optimisation
Patient was monitored continuously in CCU. Patient was started on dopamine infusion in the view of hypotension and bradycardia. Coronary angiogram revealed no significant coronary artery disease. Thorough preoperative examination was done as part of pre anaesthetic check up and the patient attender was counselled about the risk involved & need for postoperative elective ventilation. On the day of surgery, centre line and arterial line was inserted and fascia iliaca block(FICB) was given as a part of multimodal pain approach. FICB helps to block the femoral nerve, lateral femoral cutaneous nerve & sometimes branches of the obturator nerve & hence provides excellent pain relief after hip surgery. Surgery was proceeded with general anaesthesia with the preoperative peripheral nerve block. All standard ASA monitors were connected along with arterial & CVP monitoring. Induction was done with agents such as Inj.Etomidate 10 mg, Inj. Fentanyl 100mcg and Inj Atracurium 30mg . Glycopyrrolate was avoided to prevent tachycardia. Anaesthesia was maintained with Oxygen and air with Desflurane. Nitrous oxide was avoided in view of severe PAH. Dopamine infusion was continued throughout intra operatively. Intraoperative period was uneventful, and the patient was shifted to CCU for elective postoperative ventilation. Patient was extubated in CCU after two hours. Patient was shifted to the ward two days later.
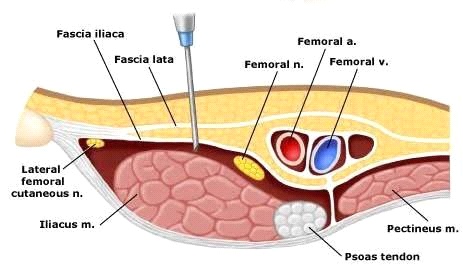
FASCIA ILIACA BLOCK
Discussion
Mitral stenosis is found to be a common valvular lesion in Rheumatic heart disease. Patients will be usually asymptomatic for more than 10 years and generally symptoms arises when valvular area reaches 1.5 to 2.5 cm²
Haemodynamic changes
- Increase the left atrial pressure and left atrial enlargement
- Increased chances of atrial fibrillation and thromboembolic events
- Decreased LV filling
- Left ventricular end diastolic volume and left ventricular end diastolic pressure are reduced
- Increase in pulmonary venous and pulmonary arterial pressure
- Right ventricular hypertrophy, Right ventricular dilation and failure
Chest Xray
- Enlarged LA (2nd heart shadow)
- Enlarged RV and RA in advanced disease
- Pulmonary edema
ECG
- P mitrale in LAD
- AF
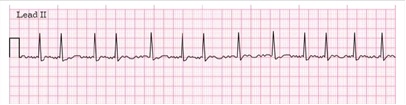
ATRIAL FIBRILLAION

P MITRALE
Echo
- To assess valvular anatomy, surface area and gradient across valve
Normal valve area – 4 to 6 cm²
Mild stenosis 1.5 to 2cm²
Moderate stenosis 1 to 1.5 cm²
Critical stenosis less than 1 cm²
- To assess any thrombus in LA
Symptoms
- Includes exertional dyspnoea, palpitations, hemoptysis and thromboembolic symptoms.
- Angina can occur as a result of RVH rather than coronary artery disease.
- Enlarged LA can cause dysphagia, hoarseness of voice.
Signs
- Low volume pulse +/- AF
- Signs of RV failure
- On auscultation there is tapping apex beat, loud S1 with the opening snap and loud P2
- Mid diastolic murmur with presystolic accentuation heard at apex at lateral decubitus position.
Anaesthetic management
- MS patients will have fixed cardiac output.
- Neuraxial anaesthesia is therefore avoided as it compromises hemodynamic stability. Hence General anaesthesia is preferred.
Goals
- Sinus rhythm should be maintained.
- Tachycardia should be avoided for sufficient diastolic filling time
- Preload – Maintain normovolemia as they are susceptible for pulmonary edema
- Afterload – Decrease in SVR can affect coronary perfusion.
- Hypoxia, Hypercapnia, Acidosis should be avoided.
Intraop management
- Intubation response should be blunted as it could increase heart rate.
- Ketamine is avoided as it cause tachycardia
- Avoid N20 in case of PAH
- Invasive hemodynamic monitoring is required.
- Pulmonary artery catheter and Transesophageal echo if required.
- Emergency drugs such as adrenaline, phenylephrine, milrinone, beta blockers, amiodarone should be kept ready
- Inhaled nitric oxide or prostacyclin for pulmonary hypertension.
Post op management
- Anticoagulants should be initiated as early as possible as a part of both DVT and thromboembolic prophylaxis
- Adequate pain control with multi modal analgesia should be continued
Conclusion
- Anaesthetists are an integral part of any team involving the management of patients with mitral valve disease. It is essential to have a thorough pre op evaluation and optimisation before commencing the surgery & careful monitoring during the perioperative period to avoid complications.
 Dr Mohamed Najibullah
Dr Mohamed Najibullah
Consultant, Department of Anesthesiology
Kauvery Hospital, Chennai
 Dr Nirmalraj Murugesan
Dr Nirmalraj Murugesan
DNB Resident 2nd Year
Department of Anesthesiology
Kauvery Hospital, Chennai