Index case
A 69-year-old female hypertensive patient presented to the emergency department with complaints of noisy breathing and exertional shortness of breath for the last 1 month which worsened over the last 2 days to NYHA class IV. On examination she was conscious, and her vital signs revealed pedal edema, elevated jugular venous pressure, tachypnea (RR 35-40/min) with usage of accessory muscles of respiration, sinus tachycardia (HR 120/min), elevated blood pressure (BP 160/90 mmHg) and hypoxia (SpO2 85% in room air). She got intubated with 7mm Endotracheal tube in view of worsening respiratory distress and was managed further in intensive care unit. Her chest x ray revealed peri-hilar infiltrates and bilateral pleural effusion consistent with pulmonary edema, 2D Echocardiography revealed a reduced Ejection Fraction of 35% with regional wall motion abnormality in left anterior descending artery territory. Her serial ECGs showed Q waves in anterior leads with no dynamic changes and cardiac enzymes (Troponin I and CK-MB) were normal. She was diagnosed as a case of ischemic cardiomyopathy with HFrEF (Heart failure with reduced ejection fraction). She was managed with diuretic infusion, antiplatelets and statins. She improved clinically and was extubated after 24 hours and was given pre-emptive NIV after extubation.
Her tachypnoea persisted and an audible stridor was heard. She showed no improvement in spite of diuretics and NIV. On probing, her attendants revealed that in the past, she was managed as a case of HFrEF and pulmonary edema, 2 months before her present admission. During that admission, she was intubated and was on mechanical ventilator for 3 days. Her extubation was uneventful during her previous admission and was discharged on anti-platelets, statins and diuretics. However, she experienced noisy breathing associated with breathlessness since then which later worsened and led to her current admission.
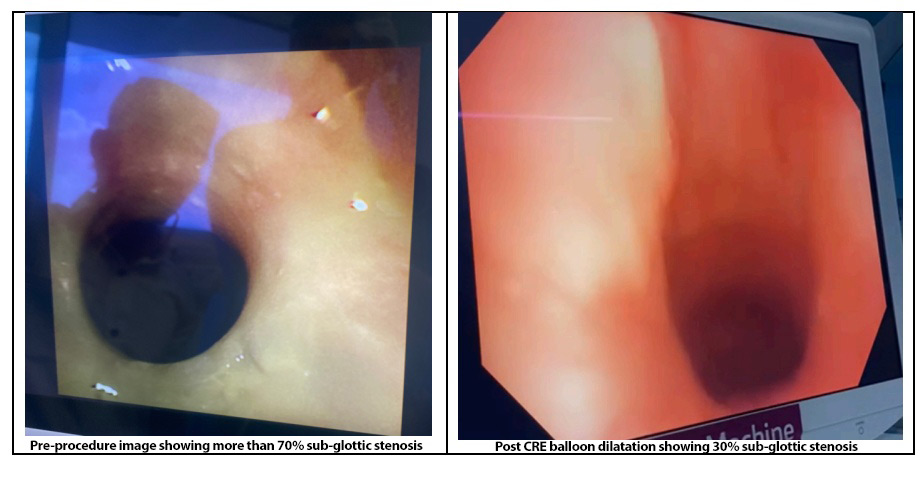
On this background history, an audible stridor and extubation failure during current admission, a diagnosis of post intubation tracheal stenosis (PITS) was suspected. Computed tomography scan of her chest and neck revealed more than 70% stenosis in the subglottic region. She was taken to the OT and using LMA as conduit, check bronchoscopy was done which confirmed a 70% subglottic stenosis with a concentric ring. Balloon dilatation was done using CRE (controlled radial expansion) balloon and stenosis improved to 30%. There was significant vocal cord and sub-glottic mucosal edema. Patient was intubated and was kept on elective mechanical ventilation post procedure. She was treated with systemic steroids (Inj Methyl prednisolone 40mg i.v q6 hourly for 48 hours) after which a cuff leak test was performed, and she was extubated successfully. She remained stable and her stridor resolved. Biopsy from the sub-glottic region revealed ischemic necrosis with inflammation which was consistent with the diagnosis of PITS (post intubation tracheal stenosis). She was put on tapering dose of steroids and was discharged with advice to follow up after 2 weeks for check bronchoscopy.
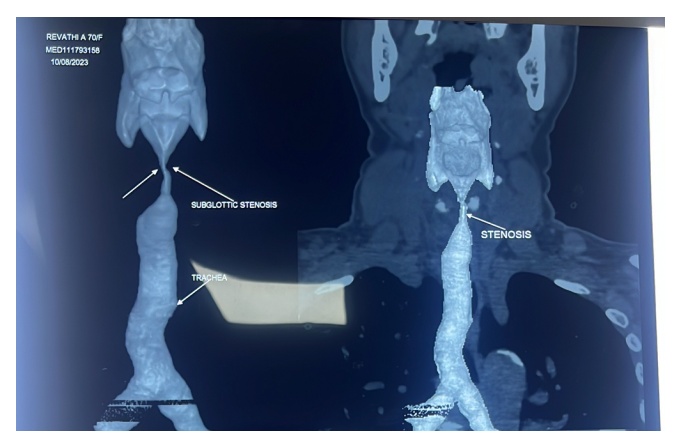
3D reconstruction of CT neck showing severe sub-glottic stenosis
Discussion:
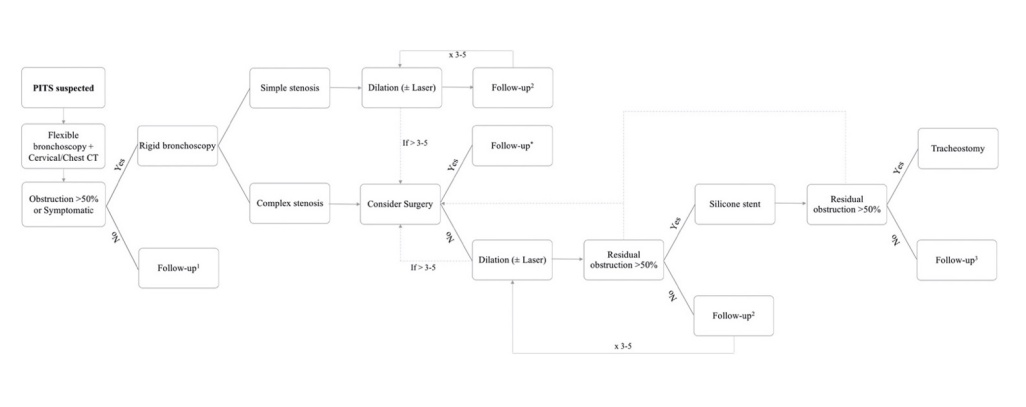
Sub-glottic stenosis is narrowing of airway between the vocal cords and lower border of cricoid cartilage. PITS (post intubation tracheal stenosis) is the most common cause for sub-glottic stenosis. Inappropriate endotracheal tube size (too large), female sex, older age, high tracheal cuff pressures(>30cmH20), traumatic intubation, hypotension during mechanical ventilation are some of the risk factors for PITS.
Pathophysiology:
The above-mentioned risk factors interfere with the blood supply to tracheal mucosa leading mucosal ischemia, necrosis and ultimately resulting in stenosis.
Severity classification:
The severity of sub-glottic stenosis is assessed by Meyer-cotton grading scale.
• Grade 1 stenosis is lumen obstruction less than 50%.
• Grade 2 stenosis is lumen obstruction between 51% and 70%.
• Grade 3 stenosis is lumen obstruction between 71% and 99%.
• Grade 4 stenosis is complete lumen obstruction
Simple vs complex PITS:
• Simple PITS: short (<1 cm), regular, and concentric
• Complex PITS: irregular, large, involvement of sub-glottic region or 2 or more sites
of trachea, associated with tracheomalacia
Clinical features:
Tracheal stenosis up to 50% can be asymptomatic unless the patient involves in some strenuous activity. Stenosis 50-70% causes stridor and breathlessness on severe exertion whereas a stenosis more than 70% is symptomatic even at rest
Diagnosis:
• CT virtual bronchoscopy as in the index case
• Flow volume loop in spirometry reveals fixed airway obstruction pattern
• Video bronchoscopy gives direct visualisation of the extent and severity of narrowed
Management:
Simple PITS can be managed by bronchoscopy and dilatation whereas complex PITS usually requires surgical intervention. However, if the patient is unfit/unwilling for surgery, bronchoscopic interventions can be considered in complex PITS. Bronchoscopic interventions include: Balloon bronchoplasty, rigid bronchoscopy and coring, electrocautery incision, laser and cryotherapy. Recurrences are fairly common and most cases would need two to three bronchoscopic dilatations. Local steroid instillation seems to reduce the recurrence risk.
 Dr. R. Nithiyanandan
Dr. R. Nithiyanandan
Associate Consultant – Pulmonology
Kauvery Hospital, Chennai.