Introduction
Headaches are experienced by most people from time to time, which affects relatively large minority of the people. Among them Migraine and tension headaches are the two most commonly encountered headaches. But cervicogenic headaches are contributes only 0.4-4% of people, which often misdiagnosed due to its complex presentation. It affects younger age group between 30 to 50 years. This disease needs early diagnosis and management to stop the chronicity and complex presentation. Hence the early management reduces the burden of medication overuse in this age group to more severe pain. Now a day’s ultrasound based therapeutic pain intervention plays a vital role in cervical spine related pain procedure. It would be consider as a best in diagnostic blockade and therapeutic management in these condition.
Cervicogenic headache Management
The cervicogenic headache was usually begins with neck region, but due to the multiple connections of cutaneous branches with trigeminal nerve neucleous the headache was referred to periorbital, temporal and occipital areas. This unique pathophysiology leads to sharing of the common area of pain with the primary headaches and disease chronicity. The etiology of cervicogenic heaadache is confirmed by the usual imaging modalities for head and neck region. The most frequent findings in the literature were a rectilinearization of the cervical spine and/or disc protrusions. A cervicogenic headache is thought to be referred pain arising from C1, C2, and C3 spinal nerve; therefore, any structure innervated by the C1–C3 spinal nerves could be the source of a cervicogenic headache. Now a days ultrasound guided injections are routinely used in anaesthesia and pain practices. Depends upon the etiology the ultrasound guided diagnostic anesthetic blocks was utilized to confirm the diagnosis, which require specialized skills.
Usg guided interventions
In cervicogenic headache the treatment includes physical therapy, exercise, and interventional procedures. An anesthetic blockade with real time USG successfully utilized for temporary pain relief, which enhance the patient’s tolerance for physical therapy.
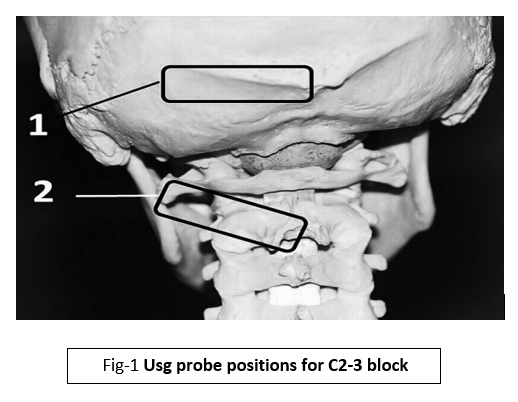
Another treatment option for a cervicogenic headache is interventional treatment with usg guidance, which was target oriented, effective and less complicated. As we know the etiology, C2-C3 dorsal rami was the principal nerve which involved in this condition. The C2-C3 nerve was targeted with Usg in the neck region near the occiput either sitting or lateral position. The nerve was usually sandwiched between semispinalis capitis and inferior obliqus muscles . This was the area where the probe was positioned and the nerves were blocked.
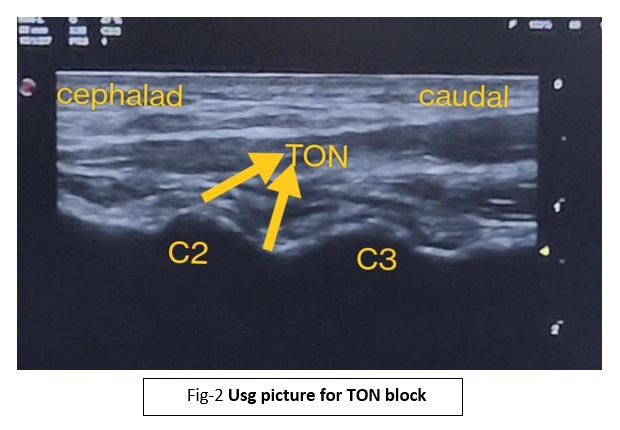
The next one was the third occipital nerve , for which patient was placed in lateral position and keep the probe along cephalic caudal direction. Usually at the level of C2 superior artricular facet the third occipital nerve (TON) was identified and blocked.
Third occipital nerve block (TON)
These procedures can be performed as daycare basis; local anaesthetics and steroid are used. Some patients may require 2 to 3 injections for complete cure. In chronic condition radiofrequency (RF) ablation technique was successfully used for long-term pain relief. In this technique, real time ultrasound was used for ideal needle placement near the nerves for successful ablation.
Conclusion
Cervicogenic headache is a common cause of a chronic headache that is often misdiagnosed due to complex and similar presentation with the primary headache syndromes. Management of this condition requires a multidisciplinary approach. Early diagnosis and treatment are important to decrease desensitization and alleviate pain in these patients. Ultrasound guided pain interventions are consider to be very useful tool in early diagnosis and safe therapeutic modality in this condition.
References
1.Govind J, Bogduk N. Sources of cervicogenic headache among the upper cervical synovial joints. Pain Med 2021:pnaa469. Doi: 10.1093/pm/pnaa469.
2.Shimohata K, Shimohata T. [Clinical Aspects of Cervicogenic Headache]. Brain Nerve 2020;72:251-8.
4.Fredriksen TA, Sjaastad O. Cervicogenic headache: current concepts of pathogenesis related to anatomical structure. Clin Exp Rheumatol. 2000;18(2 Suppl 19):S16–8.
5.Biondi DM. Cervicogenic headache: diagnostic evaluation and treatment strategies. Curr Pain Headache Rep. 2001;5:361–8.

Dr. Karthick Raja
Consultant Anaesthesiologist
Kauvery Hospital, Chennai



