HISTORY
A 49-year-old female brought to ER with h/o increased lethargy and drowsiness with generalized poor response noted by the attenders since morning with occasional eye opening. Pt was on psychiatric drugs for hallucinations, anxiety, and insomnia with no other proceeding or associated significant symptoms H/o recent increase in dosage of her psychiatric drugs [t. Cirq plus 10mg (zolpidem tartrate and melatonin), t. sizodon md 0.5 mg (risperidone)] 3 days back. No h/o fever, cough, vomiting, sob, seizure, chest pain, abdomen pain, bowel and bladder incontinence
EXAMINATION
On examination pt was afebrile, not tachypneic, Heart rate was 79/min and BP of 100/60 mm hg. Her room air saturation was 71% and her GCS were 8/15 with roving of eye movement seen. On systemic examination her power, sensation was not assessable, hypotonia was noted in all 4 limbs and Reflexes were decreased. Other systemic examination didn’t show any abnormalities
Investigations:
Initial ABG with 15L Of o2 showed PH – 7.36, pCO2 – 44, pO2 – 299, Na+ – 135, K+ – 3.4, Cl – 104, Ca++ – 1.09, Hct – 33%, Glu – 129, Lac – 3.8, tHb – 10.6, MetHb – 66.2, Hco3 – 24.9, sO2 – 96.6 %
Despite of 15 l of oxygen supply spo2 was 71% and progressively worsening GCS. Bedside blood sampling was drawn and was dark blue in color, Suspicious of methemoglobinemia

TREATMENT
Pt was treated with Inj. Methylene blue 1-2 mg/kg over 5 mins and was started on Inj. Ascorbic acid 1gm in 500 ml ns iv infusion over 4 hrs. In view of low GCS pt was intubated. In the intensive care she underwent Exchange transfusion and continuous renal replacement therapy (CRRT). Her methb dropped from 70% TO 20%, however pt suffered HIE and succumbed to the condition
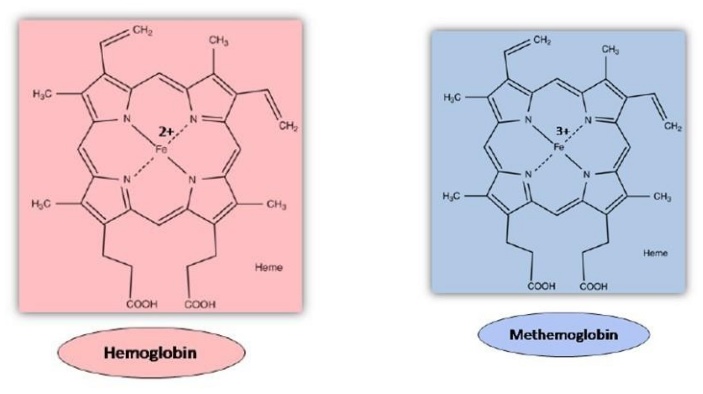
PATHOPHYSIOLOGY
 In Normal situation
In Normal situation
- Redcells constantly exposed to oxidant stress
- NADH MetHb reductase keeps oxidative stress in check by reducing MetHb to Fe2+ state
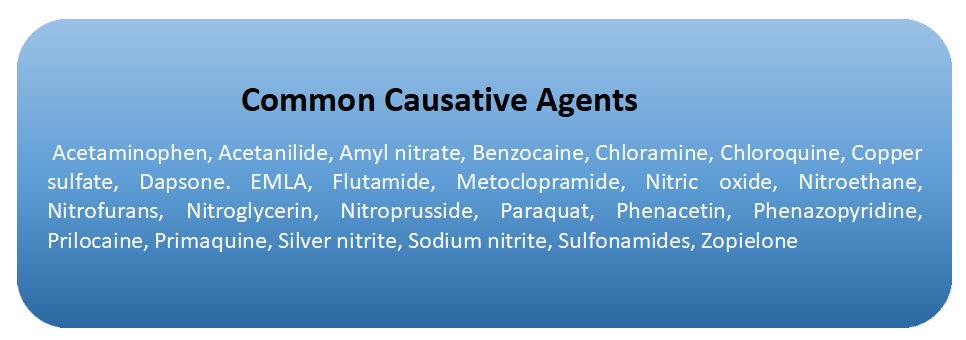
Methemoglobinemia occurs when either There is a deficiency of the reducing enzyme (NADH MetHb reductase) Or there is increased oxidative stress that cannot be handled by the body
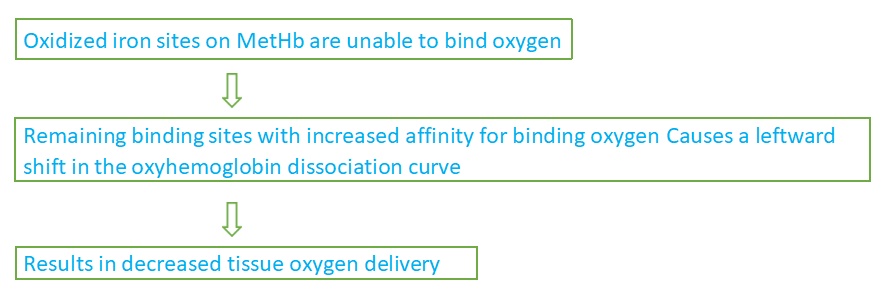
Signs & Symptoms
- Low 2 saturation that does not respond to supplemental O2
- Key diagnostic feature (sat < 85% w/o response to 100% FiO2)
- Wavelength averaging by the pulse oximeter causes a falsely low O2 reading
- Since there is no true decrease in O2 saturation, there will be no response to 100% FiO2
- Severity of symptoms correlates closely to MetHb level and severity of impaired O2 delivery
- Symptoms will be worse for any MetHb level in patients with baseline impairment of O2 delivery (i.e. CHF, pneumonia, COPD, anemia)
Complications:
- Central nervous system depression: Symptoms include extreme drowsiness, slurred speech, and slow reflexes.
- Seizures: A sign of seizures is loss of consciousness or uncontrollable jerking motions.
- Metabolic acidosis: Signs include rapid breathing, increased heart rate, and confusion.
- Organ damage: If left untreated, methemoglobinemia can damage the heart, lungs, liver, and other organs.
- Death: In rare cases, severe methemoglobinemia can be life-threatening, especially if not treated promptly.
Management
- Source identification, removal (if possible) and decontamination
- Basic Supportive Care
- Provide 100% FiO2 – lack of response should raise suspicion of methemoglobinemia
- Diagnostic Testing
- Arterial blood gas , will reveal a normal PaO2
Administer Methylene Blue 1-2 mg/kg IV
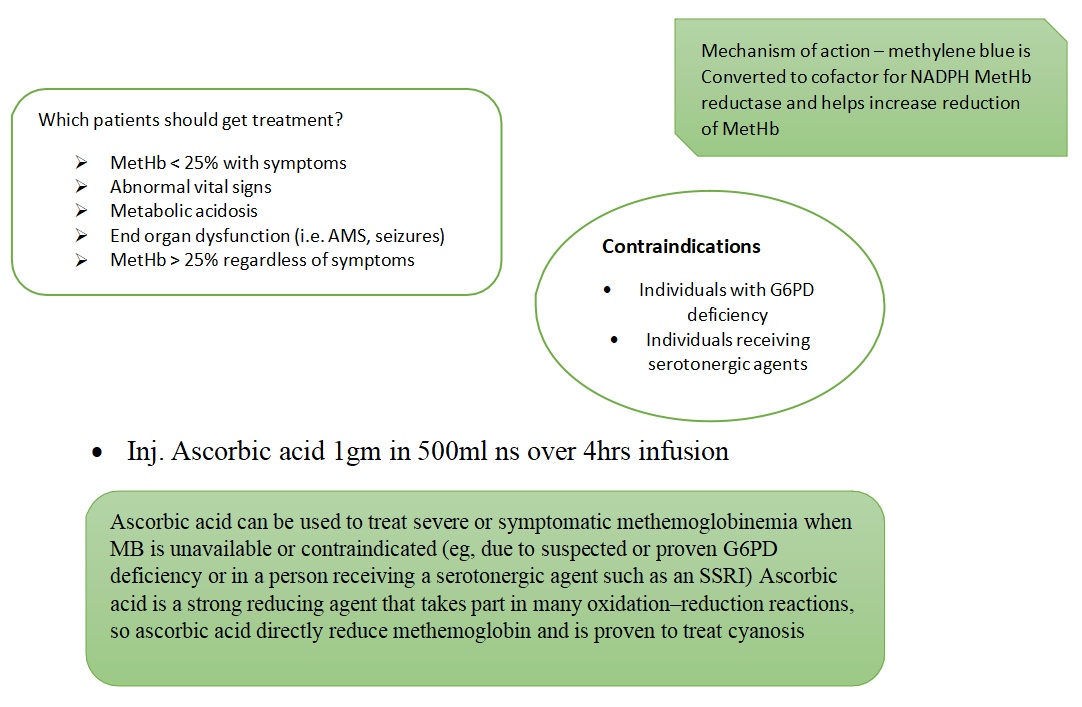
- Exchange transfusion can be used to treat methemoglobinemia when other treatments are Automated exchange transfusions may be more effective than manual ones
References
- Benz EJ, Ebert BL. Hemoglobin variants associated with hemolytic anemia, altered oxygen affinity, and In: Hoffman R, Benz EJ, Silberstein LE, eds. Hematology: Basic Principles and Practice. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 43.
- Letterio J, Pateva I, Petrosiute A, Ahuja Hematologic and oncologic problems in the fetus and neonate. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin’s Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 79.
- Means RT. Approach to the anemias. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 149
- Wolak E, Byerly FL, Mason T, Cairns Methemoglobinemia in critically ill burned patients. Am J Crit Care. 2005 Mar;14(2):104-8 [PubMed]
- Reeves DJ, Saum LM, Birhiray I.V. ascorbic acid for treatment of apparent rasburicase-induced methemoglobinemia in a patient with acute kidney injury and assumed glucose-6-phosphate dehydrogenase deficiency. Am J Health Syst Pharm. 2016 May 1;73(9):e238-42. doi: 10.2146/ajhp150591
 Dr. Abishwin
Dr. Abishwin
MEM / MRCEM Resident – Emergency Medicine
Kauvery Hospital, Chennai
 Dr. Vidya Saketharaman
Dr. Vidya Saketharaman
Consultant -Emergency Medicine
Kauvery Hospital, Chennai
 Dr. Ashok N
Dr. Ashok N
Consultant and Clinical lead – Department of Emergency Medicine
Kauvery Hospital, Chennai