▸BODY TEMPERATURE
Heat production (THERMOGENESIS)
Heat loss (THERMOLYSIS)
▸HEAT – product of metabolism ]
lost in the environment ] —> Temperature Maintained
▸Normal CORE BODY TEMPERATURE IS 36. 5°C -37.3° C
Peripheral temperature is typically 2°c -4°c lower than core temperature
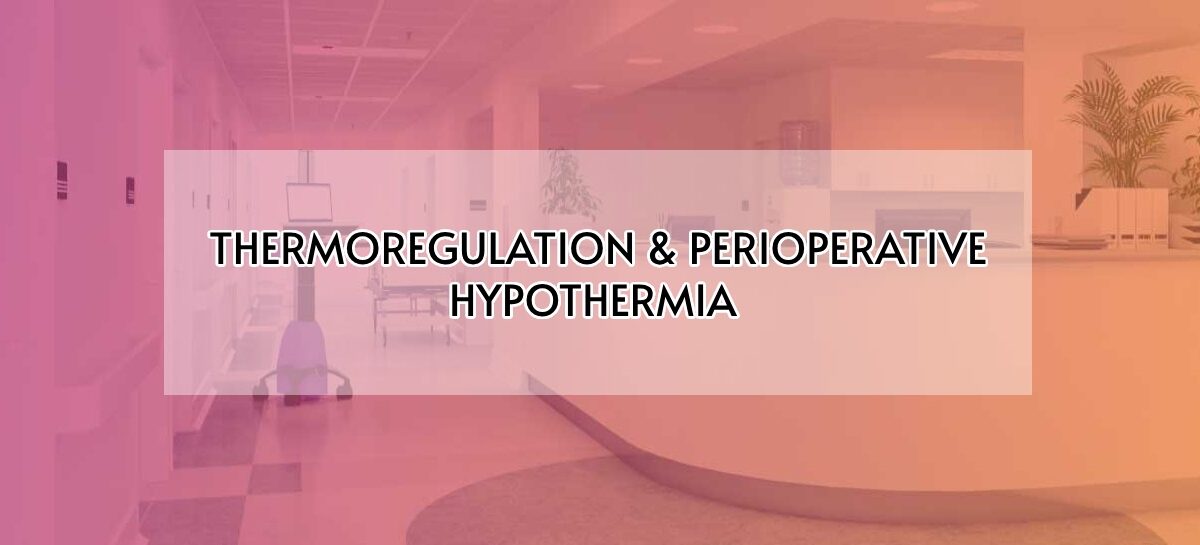
DEFINITIONS :
Thermoregulation: Haemostatic process that aims to maintain a constant core temperature.
Hypothermia: An abnormally low core body temperature, below the physiological normal limit.
Mild – > 32°c to 35 °c
moderate – 28°c to 32°c
severe – <28°c
Hyperthermia : An elevated core body temperature, above the physiological normal limit.
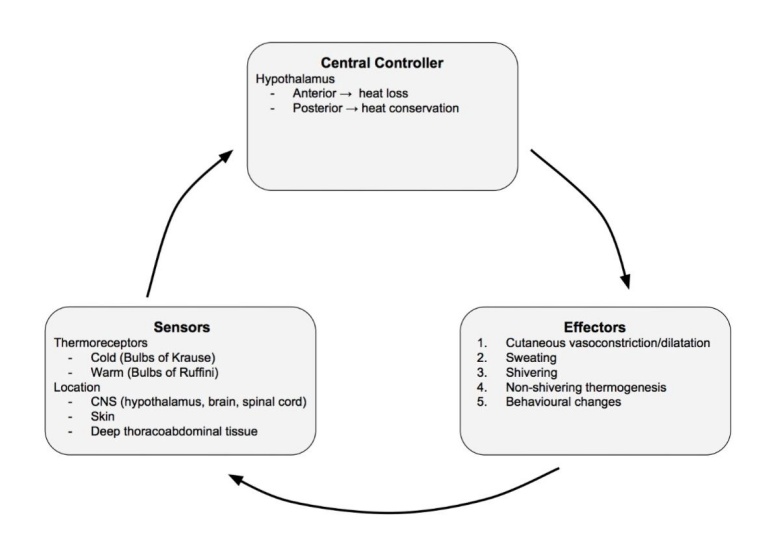
Inter threshold range: The range of core temperature over which no autonomic thermoregulatory responses occur.
Approximately 37°c + /-0.2 c in non-anaesthetised state.
Balance between heat production / Loss
Heat production
Main sources of heat production are
- Basal metabolic process( under endocrine control )
- Sympathetic activity, vascular tone
- Muscular activity
- Hormonal activity
Heat Loss
Important mechanisms of Heat loss
- Radiation
- Conduction
- Convection
- Evaporation
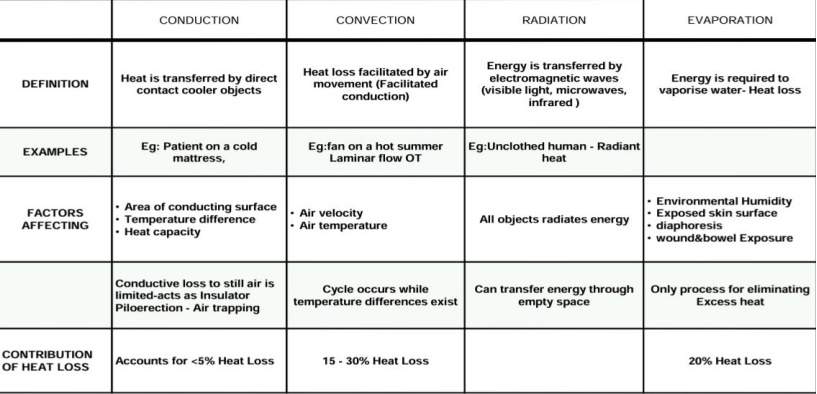
PATHWAY OF THERMOREGULATION
Cold receptors – A alpha fibres Heat loss – Sweating Vasodilation
Warm receptors – C fibres Heat conservation – Shivering Vasoconstriction
Behavioural responses: Dressing appropriately Modifying environmental temperature Assumption of body positions which oppose skin surface, Increasing voluntary movements to generate heat.
NON-SHIVERING THERMOGENESIS/CHEMICAL THERMOGENESIS
- Increase in rate of metabolism in Brown Adipose Tissue
- Stimulated by Sympathetic system or Catecholamine.
- Brown Adipose tissue – Interscapular space, around great vessels
- Brown fat has lot of Mitochondria (rich in ATP) & Sympathetic innervation.
- Can produce heat as much as 200%
- Lipolysis & Heat generation is mediated – Beta adrenergic receptors.
- Adults rarely have brown fat.
SHIVERING
- Increases body heat production in response to decreased core body temperature
- Skeletal Muscle activity is a major source of heat.
- Shivering arises from posterior hypothalamus
- However, shivering is inefficient & induces significant metabolic demand.
Cutaneous blood flow
▸Major determinant of heat loss
▸It is regulated by sympathetic nervous system
▸In adult blood flow is 400ml/min, decreased to 50ml/min cold, 2800ml/min in heat
▸Subcutaneous venous plexuses hold large volume of blood- fingers, palms ,toes and earlobes -arteriovenous anastomosis – causes significant heat loss during circulation.
Acute haemorrhage —– sympathetic nervous system vasoconstriction —- transfer large blood from venous plexus to central circulation —– important blood reservoir
Acute Haemorrhage less tolerated in warm environment
Hypothalamic Vasodilator response overrides vasoconstrictor response to Hypovolemia
Thermoregulation during general anaesthesia
▸ Body temperature is determined by cold environment -poikilothermic
- Resetting Hypothalamic thermostat
- Reduced temperature (outside)
- Administration of cold iv fluids
- Decreased basal metabolic rate
- Drug induced vasodilation
- Core compartment exposed to room temperature
- Heat required to humidify dry gases
Under GA, behavioural response is not relevant as patient are unconscious.
Thus, thermoregulatory responses under anaesthesia include Autonomic response & External thermal management
Therefore under GA, alterations in autonomic threshold include:-
- Increase in warm response threshold
- Decrease in cold response threshold
- Increase in interthreshold range 2-4°c
- Impaired shivering response due to muscle paralysis
Non shivering thermogenesis not significant in adult
Thermoregulation under regional anaesthesia
Behavioural response is impaired
Inhibition of autonomic thermoregulatory responses, core temperature decreases, skin temperature increases due to vasodilation. Therefore, patient doesn’t feel cold in spite of having a reduced core temperature
Also, RA blocks all thermal input from anaesthetized regions. Inhibit tonic cold signals from legs to thermoregulatory center
The hypothalamus wrongly interprets this as warming of legs
Decreases threshold to trigger vasoconstriction and shivering by 0.6 °c
Peripheral vasoconstriction and shivering is inhibited in blocked areas.
Reduction in threshold is proportional to the number of spinal segments blocked
Thermoregulation in combined G. A & R. A
Core temperature doesn’t plateau
Thus, it continuous to decrease throughout surgery.
Phases of hypothermia under general anaesthesia
Phase 1: Redistribution phase
- Occurs during the first hour of G. A
- Causes the largest drop in core temperature (0.5- 1.5°c). Peripheral temperature increases from 33°c to 35°c
- Redistribution is caused by vasodilation induced by G. A. Redistribution of heat from core to periphery.
Phase 2: Linear phase
- Occurs for next 2-4 hrs after G. A
- Linear reduction in core temperature. Mainly due to heat loss exceeds heat production.
- Heat loss occurs by radiation >convection> evaporation > conduction
Phase 3: Plateau phase
- Occurs after 3-4 hrs of G. A
- Core temperature stops reducing and stabilizes. Heat loss = heat production
Reduces heat loss from body. This phase absent in perpheral / autonomic neuropathy.
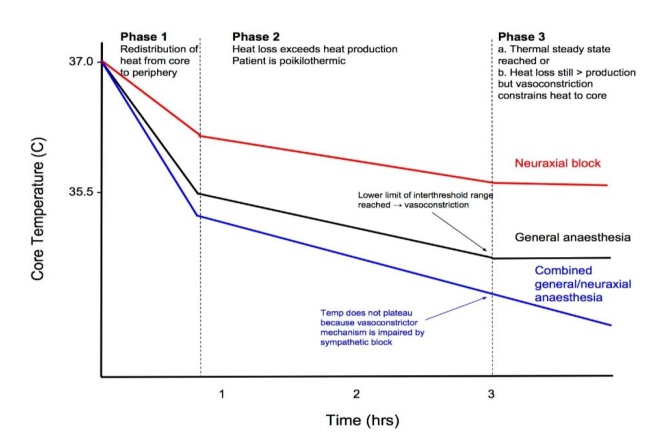
Phases of hypothermia during Regional anaesthesia
Phase 1: Redistribution phase
- Core temperature reduces first one hour due to vasodilation.
- Peripheral temperature increases due to redistribution
- Large drop in core temperature during R. A
Phase 2: Linear phase
- Occurs during next 2- 4 hrs after R. A
- Mainly due to heat loss exceeding heat production
Phase 3: Plateau phase
- Absent in R. A. This is because RA blocks nerve supply to blood vessels in the legs.
- These prevents any thermoregulatory vasoconstriction.
Thermoregulation in Newborns
- No shivering or effective vasoconstriction occurs.
- Having a large surface area to weight ratio which increases heat loss.
- Lesser subcutaneous fat for insulation.
- Non-shivering thermogenesis is however very effective.
- No thermoregulatory sweating occurs in newborns.
- No sweating ability
- Higher metabolic rate compared to adults (per kg)
- Brown fat & non shivering thermogenesis is more important in neonates.
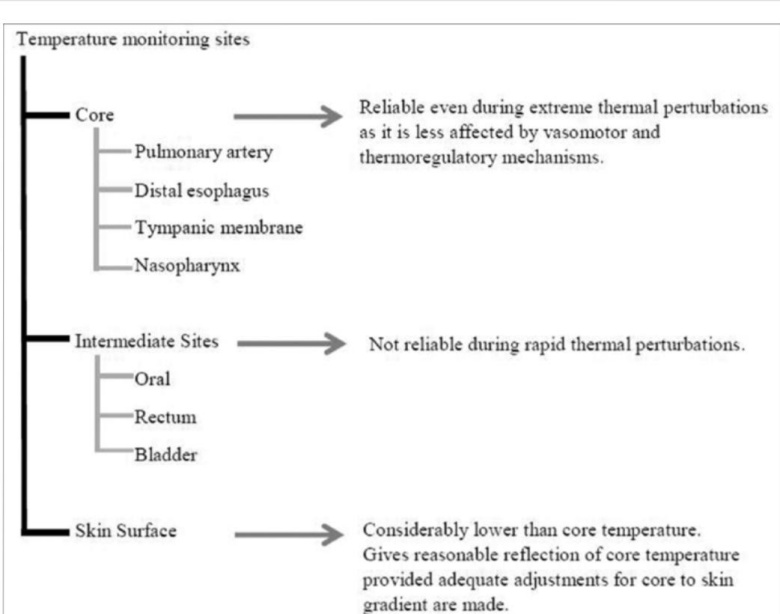
Sites of temperature monitoring
Effects of hypothermia
Thermoregulatory response: cutaneous vasoconstriction Shivering
Non shivering thermogenesis (infants)
Behavioural changes
Pathological responses
CVS: Heart rate decreases – slowing of discharge from SA node
- Paradoxical vasodilation
- Hypotension, Dysrhythmias, MI
- Cardiac output & venous capacitance
- Increase peripheral and pulmonary vascular resistance
CNS: <34 °c —mental confusion
- <32°c —– loss of consciousness
- Decreases CMRO2
- Protects against cerebral ischemia
- Delayed awakening
Haematology: Coagulopathy
Local effect: Impaired wound healing
- Drug metabolism
- Decreases reliability of pulse oximetry, Ecg, IBP
Oxygenation: Shift of oxyhemoglobin curve to left
- Increase O2 consumption and co2 production
- Increase tissue hypoxia and metabolic acidosis
Effect of Hyperthermia
Thermoregulatory response: cutaneous vasodilation, sweating & behavioural changes
Pathological Responses
Cvs : Inc. HR, inc cardiac output
-
-
- P remain stable due to vasodilation
-
Cns : Irritability — heat stroke,
>42°c — loss of consciousness
Musculo skeletal: Fluid & electrolyte loss —– muscle cramps
Beneficial effect of perioperative hypothermia
- Hypothermia reduces the metabolic demand
- O2 consumption 5% _ 7% for every Degree Celsius
- 1-3”C decrease protects against cerebral ischemia and arterial hypoxemia
- Mild Hypothermia (33-36)- Beneficial: cardiac surgeries, aneurysmal clipping, cardiac arrest, stroke, traumatic brain injury acute MI, birth injury
- Surface cooling causes hypothermia – shivering which delays core cooling
Risk factors
- Young age
- Low core temperature preoperatively
- Male sex
- General > Regional anaesthesia
Prevention of hypothermia in Adults
- Maintain OT temperature between 21_23°c
- Maintain intraoperative normothermia
- Adequate pre-warming for 30 mins prior to regional anaesthesia
- Correct underlying problems —- Sepsis
- IV fluids and blood at 4°c reduces core temperature by 0.25 ° c. So warmed iv fluids and blood products useful.
Prevention of hypothermia in Neonates
Maintain neutral thermal environment
Skin surface warming:
- Hot water warmers
- Infrared radiant heaters
- Convection heaters
- Use plastic wrap/ covers / hats / head caps
Prevent heat losses:
- Transport newborn in incubator and not bed with overhead heaters.
- Increases OT temperature to maximum levels (around 26°c if tolerable)
- Air humidification
- Place forced air warming blanket to reduce conductive heat loss
- Use of warm iv fluids – place fluid warmer close to iv access site.
TREATMENT
- Supplemental Oxygen

 Dr. Velmurugan Deisingh
Dr. Velmurugan Deisingh
Head of Department of Anaesthesia
Kauvery Hospital, Chennai
 Dr. Varalakshmy
Dr. Varalakshmy
2nd DNB Resident – Anaesthesia
Kauvery Hospital, Chennai