Introduction
Peripheral artery disease (PAD) is an atherosclerotic disease that has emerged as a major health problem. Common risk factors include ageing, smoking, diabetes and hypertension. PAD can be asymptomatic and presents later as CLI (critical limb ischemia) with gangrene and rest pain. PAD now commonly exhibits a multilevel nature, extending both supra-inguinal and infra-inguinal. If untreated it can lead to amputation of extremity mortality. In this article, we present the case of a patient with non-healing ulcer and rest pain who responded to timely endovascular revascularization overcoming the challenges of intervention in a multilevel complex arterial lesion of extremity.
Case Report
A 78 yrs, diabetic and hypertensive gentleman presented with severe disabling claudication in the right lower limb and gluteal region, worsened over the past 2yrs to rest pain in the right foot. He gave a previous history of Left femoro-popliteal bypass, CABG, and stroke.

His clinical examination revealed signs of ischemia in the right leg with a 3rd toe non-healing ulcer. Examination of the right lower limb revealed absent popliteal and distal tibial pulses; the femoral artery pulse was feeble. On auscultation, bruit was heard in the right femoral artery and in the right side carotid region. Doppler revealed monophasic flow in the right popliteal, posterior tibial artery (PTA) and peroneal artery. Absent flow in the anterior tibial vessel. ABI was 0.47 in the right and was 0.84 in the left. Echo showed dilated LV with mild systolic dysfunction, with an ejection fraction 40-45%. CT Angiogram revealed multilevel disease, 40-50% ostial stenosis of the right common iliac artery, focal superficial femoral (SFA) stenosis, isolated Popliteal segment occlusion involving TP trunk, anterior tibial artery (ATA) and proximal peroneal artery. Peroneal was reformed in midleg, distally traced up to ankle where it forms PTA and plantar artery in the foot.
He was diagnosed to have Rutherford class V critical limb ischemia. Revascularization was planned as a two-stage procedure. He was planned for right iliac artery angioplasty and stenting initially followed by infra inguinal angioplasty and stenting as a second stage.
Percutaneous transluminal angioplasty was carried out under local anesthesia. Right common femoral artery retrograde access, and angiogram showed 70% stenosis at the right common iliac ostium. Balloon expandable stent was deployed across the stenosis. Infra-inguinal angiogram showed 80% focal stenosis in proximal SFA and another at adductor hiatus beyond which artery was totally occluded. A short isolated mid-popliteal segment was seen. Sural artery and genicular artery was seen arising from that. Anterior tibial was not visualized. Proximal SFA lesion crossed with 0.035 hydrophilic guidewire and balloon angioplasty carried out. The popliteal lesion was crossed sub-intimal and re-entered into the patent mid-popliteal segment. Popliteal lesion balloon angioplasty was carried out. The wire could not be passed further down to the Peroneal artery. Under ultrasound guidance, retrograde posterior tibial access was used to cross from posterior tibial lesion into the popliteal artery. Posterior tibial lesion angioplasty was carried out. An angiogram showed recoil and a dissection flap in the TP trunk; hence a drug-eluting coronary stent was deployed across the TP trunk. Proximal popliteal and SFA were covered with a Vascular mimetic stent. Angiogram showed distal popliteal dissection; hence stented. Proximal SFA lesion showed recoil and was also stented. Post-procedure,a posterior tibial artery pulse was palpable. Doppler showed good flow in dorsalis pedis artery via plantar arch. Postoperatively his rest pain was relieved. Post endovascular ABI score improved to 0.91 in the right lower limb. The third toe tip ulcer healed after 1week.
Discussion
Multilevel arterial disease with CLI poses a significant challenge. Unfortunately, our patient was a high-risk candidate for open surgery with poor cardiac status and no suitable vein for bypass. Percutaneous endovascular intervention has become the preferred treatment of choice in such fragile elderly vascular patients because of decreasing surgical and anaesthetic risks.
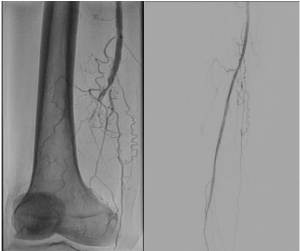
Fig 2. Check angio-Tight stenosis at the adductor hiatus level beyond which CTO of popliteal artery Completion angio- showing restoration of flow in popliteal
One of the main concerns in this patient was the development of contrast-induced acute kidney injury. To avoid that we planned our procedure as two stages with adequate hydration of the patient.
Stenting is generally the accepted clinical practice for chronic Iliac artery occlusions. Lesions with high elastic recoil balloon-expandable stents are favored because of their radial strength and accurate placement.
The second stage of the procedure was to revascularize the infrainguinal arteries. There were two difficulties we faced during the second procedure. One was the anatomical position of the popliteal artery behind the knee in the popliteal fossa. Repetitive flexion and extension of the knee with angulations of up to 120 degrees increases mechanical stress as the artery shortens and twists, causing stent fractures in popliteal segments. This makes the management of atherosclerotic lesions in popliteal artery segments difficult. A Vascular mimetic stent can be used in this popliteal segment as it adapts to the anatomy of the segment, mimicking the vessel’s natural behavior. They are found to be better in extreme mechanical stress and for lesions of long lengths.

Fig.3. The first image shows the occluded distal popliteal and TP trunk with the reformation of the peroneal, the second image showing opened up arteries with the flow to peroneal and posterior tibial
The other difficulty was to cross the lesion in popliteal trifurcation to re-enter into the tibial vessel. To overcome the challenges, techniques that we used were sub-intimal angioplasty to enter the isolated popliteal segment and a retrograde posterior tibial access. Tibial access increases the success of staying in the true lumen, as it provides more control. There is a reduced tendency of wire to get diverted into collateral branches.
Arterial dissections were managed with uncovered self-expandable stents which were used to tack the intimal flaps and maintains patency. This prevents acute vessel re-thrombosis after PTA.

Fig. 4. In-line flow to the foot is restored, showing flow up to dorsalis pedis artery
Conclusion
Endovascular therapy for combined supra-inguinal and infrainguinal peripheral artery disease is feasible and provides similar angiographic and clinical outcomes compared to open surgery and is often associated with lower procedural morbidity and mortality rates in experienced hands. Newer techniques are available to ensure success in infra-inguinal revascularization albeit at a high cost.
References
1.Norgren, L, Hiatt, WR, Dormandy, JA,et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J VascEndovasc Surg. 2007; 33(suppl 1):S1–S75. doi: 10.1016/j.jvs.2006.12. 037.
2.Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, Mills JL, Ricco JB, Suresh KR, Murad MH; GVG Writing Group. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg.2019;69(6S):3S-125S.e40. doi:10.1016/j.jvs.2019.02.016.
3.Dalai, S., Narayana, R.V., Pati, R. et al. Supera Stent for Management of Occlusive Popliteal Artery Disease: \
4.Tamunoinemi Bob-Manuel, Koyenum Obi and Zola N’Dandu Successful Revascularization of Infrapopliteal Chronic Total Occlusions Using the Plantar Arch as a Conduit and Retrograde Pedal Access Ochsner Journal June 2021, 21 (2) 209-213; DOI: https://doi.org/10.31486/toj.20.008.
5.Goltz JP, Ritter CO, Kellersmann R, Klein D, Hahn D, Kickuth R. Endovascular treatment of popliteal artery segments P1 and P2 in patients with critical limb ischemia: initial experience using a helical nitinol stent with increased radial force. J EndovascTher. 2012 Jun;19(3):450-6. doi: 10.1583/11-3591MR.1. PMID: 22788900.

Dr. Archana Rajan
DNB Resident – Department of Vascular Surgery